Perioperative blood transfusions are often necessary to stabilize patients undergoing major surgery, especially those with cancer. However, a comprehensive new study, The ARCA-1 Trial, published in Anesthesia & Analgesia (April 2025) by Cata et al., raises concerns about their long-term safety. The study presents strong evidence that perioperative transfusion of packed red blood cells (pRBCs) in cancer surgery is linked with increased 1-year mortality and adverse postoperative outcomes.
Study overview: the ARCA-1 trial
The ARCA-1 (Perioperative Care in the Cancer Patient-1) trial is the largest prospective, international, multicenter observational study to date examining the impact of perioperative blood transfusions on outcomes following major cancer surgery.
Study design
- Type: Prospective observational cohort
- Participants: 1079 patients undergoing elective noncardiac cancer surgery with curative intent
- Time frame: July 2020 – December 2021
- Centers: 16 centers across North America, Asia, and Europe
Objectives
- Primary endpoint: 1-year all-cause mortality
- Secondary endpoints:
- 30-day morbidity and mortality
- Cancer-specific 1-year mortality
- Overall survival (OS)
- Postoperative complications
Major findings
Transfusion rates and triggers
- 21.1% of patients received perioperative pRBC transfusions.
- Transfusions typically occurred when hemoglobin (Hb) fell between 7 and 9 g/dL.
- Only 9% of transfusions were due to overt organ hypoperfusion, indicating a potentially liberal use of transfusions.
Mortality impact
- 1-year mortality was 19.7% in transfused patients vs 6.5% in non-transfused.
- Dose-response relationship observed:
- 0 units: 7.2% mortality
- 1–2 units: 18.2%
- 2 units: 31%
Cancer progression and survival
- Cancer progression within 1 year:
- Transfused: 32.6%
- Nontransfused: 18.9%
- Cancer-specific 1-year mortality:
- Transfused: 13.6%
- Nontransfused: 4.6%
- Overall survival:
- Transfused patients had an 85% higher hazard of death
- Transfused patients had an 85% higher hazard of death
Why might transfusions worsen outcomes?
Several mechanisms may explain this association:
- Transfusion-related immunomodulation (TRIM):
- pRBCs contain > 3000 proteins that suppress immune functions.
- Inhibition of cytotoxic T cells and monocytes.
- Increased levels of prostaglandins, growth factors, and angiogenic cytokines.
- Promotion of cancer microenvironment:
- Enhances conditions favorable to tumor recurrence and metastasis.
- Enhances conditions favorable to tumor recurrence and metastasis.
- Storage-related damage:
- Longer storage times increase oxidative stress and decrease red cell efficacy.
Postoperative complications in transfused patients
Transfused patients had significantly more postoperative issues, including:
- Higher ICU admission rates
- Longer hospital stays (median: 7 vs 4 days)
- Higher rates of:
- Sepsis
- Acute kidney injury (AKI)
- Postoperative bleeding
- Wound infections
- Delirium
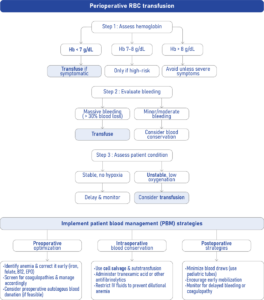
Implementing patient blood management (PBM)
A structured PBM program can help mitigate risks associated with transfusions. The World Health Organization (WHO) supports global adoption of PBM protocols.
1. Identify and treat preoperative anemia
- Hemoglobin check at least 4 weeks before surgery
- IV or oral iron supplements
- Erythropoiesis-stimulating agents when appropriate
2. Minimize intraoperative blood loss
- Laparoscopic over open surgery where possible
- Use of antifibrinolytics (e.g., tranexamic acid)
- Normothermia to support coagulation
3. Adopt restrictive transfusion thresholds
- Consider transfusion only when Hb < 7 g/dL in stable patients
- Evaluate organ function and perfusion
4. Educate clinicians and patients
- Regular training and awareness programs
- Multidisciplinary teamwork
Conclusion
The ARCA-1 study provides robust, international data demonstrating that perioperative blood transfusions in cancer surgery are associated with significantly worse outcomes, including 1-year mortality, cancer progression, and postoperative complications. The findings advocate for a paradigm shift toward personalized transfusion practices and comprehensive patient blood management strategies.
For patients and providers, the message is clear: Blood is life-saving, but not risk-free. Use it wisely.
Reference: Cata JP et al. The Association Between Perioperative Red Blood Cell Transfusions and 1-Year Mortality After Major Cancer Surgery: An International Multicenter Observational Study. Anesth Analg. 2025;140:782-794.
For more information on blood transfusions, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
AI On Call: Case of the Week
A 67-year-old man is scheduled for elective open colon cancer resection. He has mild anemia (Hb 10.2 g/dL) but is hemodynamically stable. Intraoperatively, his Hb drops to 8.6 g/dL. Should you transfuse?
Here’s what the Anesthesia Assistant recommends doing: