Mechanical Ventilation and Pediatric Brain Risk
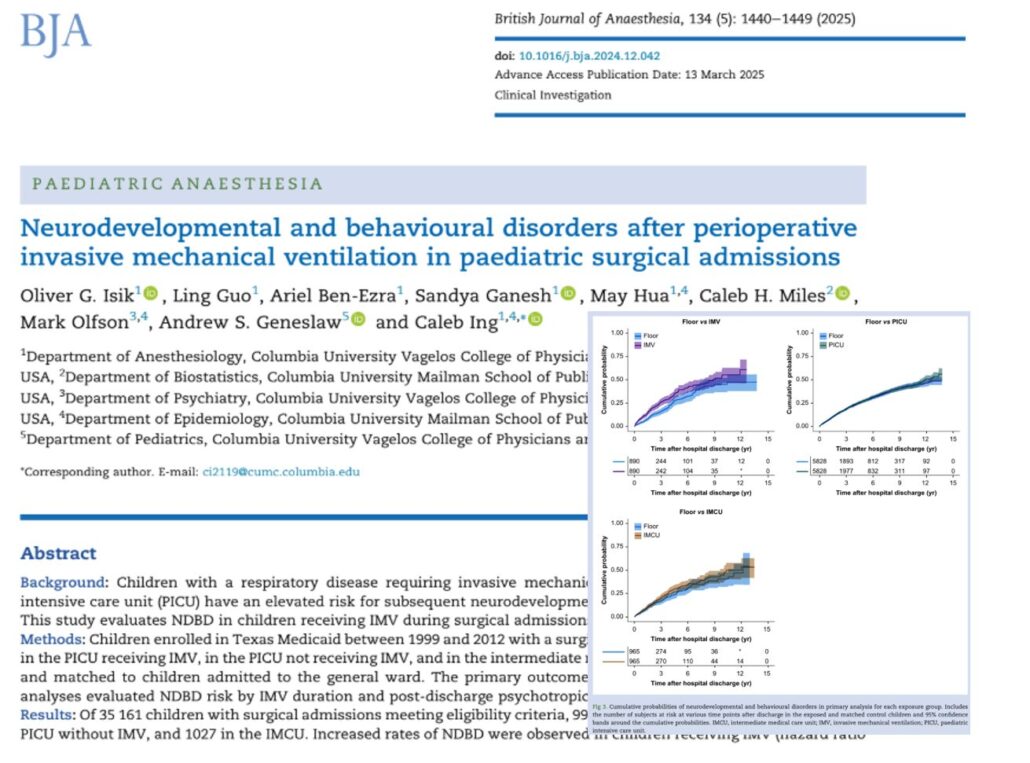
A major study by Isik et al., published in the British Journal of Anaesthesia (2025), has revealed compelling evidence that children requiring invasive mechanical ventilation (IMV) during surgical admissions face significantly increased risks of developing neurodevelopmental and behavioral disorders (NDBDs) after hospital discharge.
Conducted by a team from Columbia University and based on a comprehensive Medicaid database of pediatric patients, this study brings to light the long-term mental health consequences of life-saving interventions in the pediatric intensive care unit (PICU).
Why this study matters
Children admitted to intensive care often undergo mechanical ventilation to manage critical respiratory issues. While this intervention is essential for survival, concerns are growing about its long-term neurodevelopmental impact.
Key highlights:
- Children who received IMV during surgical admission had a 91% higher risk of being diagnosed with NDBDs after discharge.
- Children ventilated for over 96 hours face a 302% increase in risk.
- Only the IMV group showed increased post-discharge psychotropic medication use.
- Children in the PICU without IMV and those in intermediate care units (IMCU) did not show significant increases in risk.
What did the study find?
Neurodevelopmental and behavioral disorders (NDBDs)
These included:
- Attention-deficit/hyperactivity disorder (ADHD)
- Autism spectrum disorder (ASD)
- Speech and language disorders
- Intellectual disabilities
- Anxiety and mood disorders
Statistical findings:
Children admitted to the pediatric intensive care unit (PICU) and who required invasive mechanical ventilation (IMV) had a 91% higher risk of developing neurodevelopmental and behavioral disorders after discharge compared to children admitted to the general hospital ward. This association was statistically significant.
In contrast, children admitted to the PICU who did not require IMV had only a 12% increased risk, and this result was not statistically significant.
Children treated in the intermediate care unit (IMCU) actually had a 12% lower risk compared to the general ward group, but this difference was also not statistically significant.
When looking at the duration of ventilation:
- Children who were mechanically ventilated for more than 96 hours had a 202% increased risk of developing neurodevelopmental or behavioral disorders. This finding was highly significant.
- Those ventilated for less than 96 hours had a 32% increased risk, but this was not statistically significant.
Psychotropic medication use
Children receiving IMV were also:
- 3.2 times more likely to require long-term psychiatric medication.
- This trend remained significant even after excluding anti-epileptic drugs.
Real-world impact
Children exposed to extended IMV may:
- Struggle with language and motor skills.
- Develop attention and learning problems in school.
- Require ongoing mental health care.
Why might IMV increase these risks?
Possible mechanisms:
- Hypoxia and ischemia: Reduced oxygen can affect brain development.
- Inflammation: Systemic inflammation during critical illness may impair neural pathways.
- Sedatives and analgesics: These drugs can disrupt synaptic development.
- Delirium: Common in PICU, delirium has been linked to long-term cognitive deficits.
- Immobility: Extended bed rest can limit sensory and motor development.
These factors may act synergistically, especially during vulnerable developmental windows.
Conclusion
While IMV is an essential tool in pediatric surgical care, this study highlights an urgent need to consider its potential long-term effects. The findings support integrating developmental follow-up into routine care for these vulnerable patients and advocate for minimizing IMV duration where possible.
With increased awareness and proactive management, we can improve not only the survival but also the quality of life for children recovering from surgical critical care.
Reference: Isik OG et al. Neurodevelopmental and behavioural disorders after perioperative invasive mechanical ventilation in paediatric surgical admissions. Br J Anaesth. 2025;134:1440-1449.
For more information on this topic, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights, all in one place. Download the app today and experience the future of anesthesia education and decision-making.