Belen De Jose Maria, Luc Tielens, and Steve Roberts
EPIDURAL ANESTHESIA IN CHILDREN
INTRODUCTION
Epidural analgesia is commonly used in addition to general anesthesia and to manage postoperative pain. Effective postoperative pain relief from epidural analgesia has numerous benefits including earlier ambulation, facilitating weaning from ventilators, reducing time spent in a catabolic state, and lowering circulating stress hormone levels. Precise placement of epidural needles for single-injection techniques and catheters for continuous epidural anesthesia ensures that the dermatomes involved in the surgical procedure are selectively blocked, allowing for lower doses of local anesthetics to be used and sparing unnecessary block in nondesired regions. The approach to the epidural space can be at the caudal, lumbar, or thoracic level.
ANATOMY AND PHYSIOLOGICAL IMPLICATIONS
There are significant anatomical differences in children com-pared with adults that should be considered when using neuraxial anesthesia. For instance, in neonates and infants, the conus medullaris is located lower in the spinal column (at approximately the L3 vertebra) compared with that in adults, in whom it is situated at approximately the L1 vertebra. This is a result of different rates of growth between the spinal cord and the bony vertebral column in infants. However, at approximately 1 year of age, the conus medullaris reaches the L1 level similar to that in an adult.
NYSORA Tips
- In neonates and infants, the conus medullaris ends approximately the L3 level as opposed to adults, where it is located approximately at the L1 vertebra.
- At approximately 1 year of age, the conus medullaris reaches the L1 level, similar to that in an adult.
The sacrum of children is also more flat and narrow compared with the adult population. At birth, the sacral plate, which is formed by five sacral vertebrae, is not completely ossified and continues to fuse until approximately 8 years of age (although it may take until 21 years of age). There is a 6% incidence of sacral atresia. The incomplete fusion of the sacral vertebral arch forms the sacral hiatus. The caudal epidural space can be accessed easily in infants and children through the sacral hiatus. Because of the continuous development of the sacral canal roof, there is considerable variation in the sacral hiatus. In young children, the sacral hiatus is located more cephalad than in older children, and the dural sac may end more caudally: at S4 in infants younger than 1 year and at S2 in older children. Therefore, because of the increased risk of accidental dural puncture, caution is warranted when placing caudal blocks in infants.
NYSORA Tips
- In young children, the sacral hiatus is located more cepha-lad than in older children, and the dural sac may end more caudally (at S4 in infants younger than 1 year).
- Caution with the use caudal blocks is warranted in infants because of the risk of dural puncture.
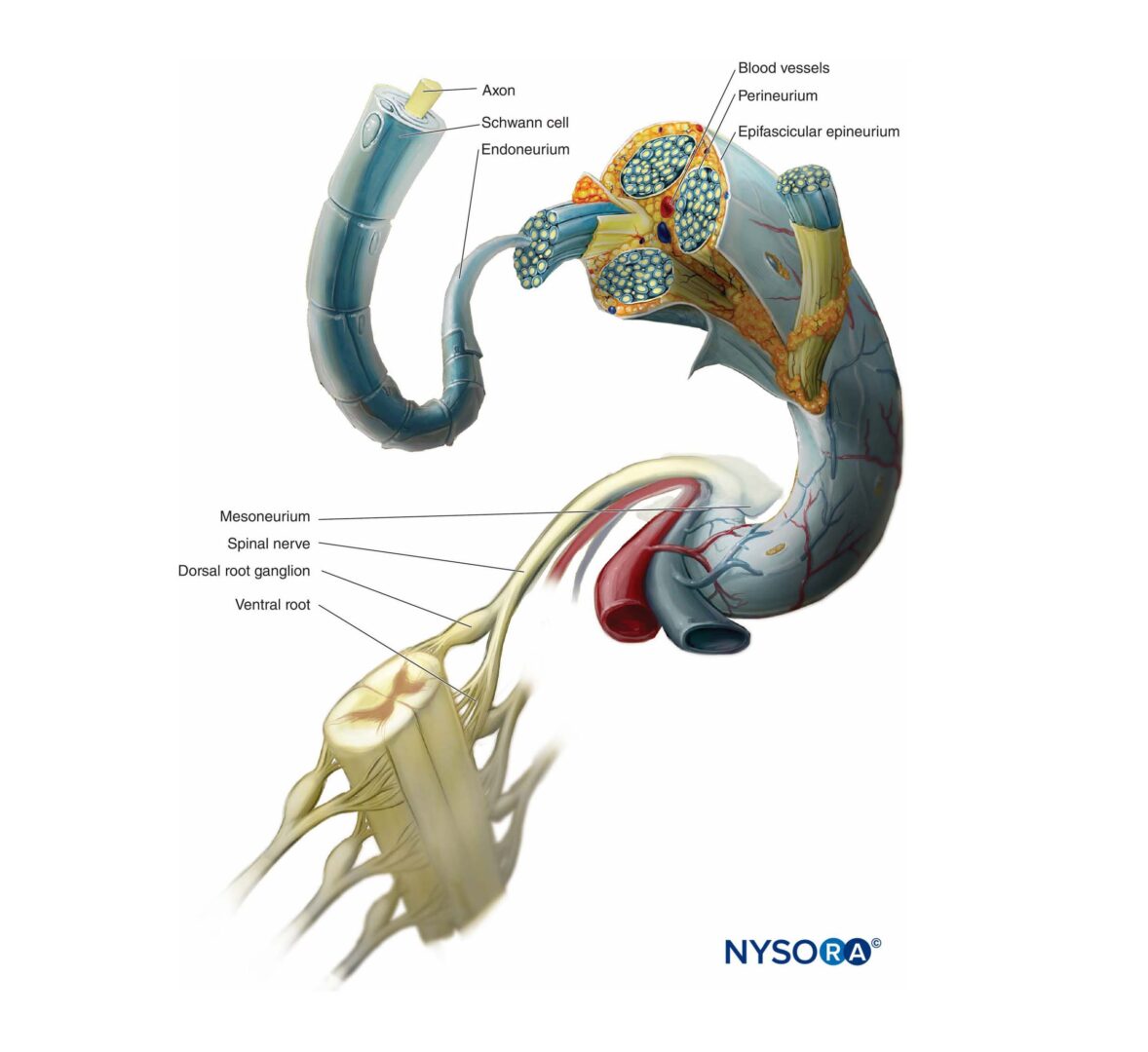
Ultrasound (US) assessment of the neuraxial structures is less challenging in younger children because ossification is less developed. In infants, the spinal cord fibers, the cerebrospinal fluid (CSF), and the dura mater are easily identified using linear high-frequency US probes. It has also been suggested that the epidural fat is less densely packed in children than in adults. The loosely packed epidural fat may facilitate the spread of local anesthetic and help achieve a quicker block onset. It may also allow the unimpeded advancement of epidural catheters from the caudal epidural space to the lumbar and thoracic levels. However, the final placement of a catheter’s tip is best monitored directly under US guidance or indirectly by identifying the injection of local anesthetic.
The amount of CSF per body weight is higher in neonates and infants (4 mL/kg) compared with adults (2 mL/kg), and the CSF is localized primarily in the spinal canal. In addition, the spinal cord in neonates is still nonmyelinated, meaning that lower concentrations of local anesthetic can be effectively used.Because children have a higher cardiac output compared to adults, the systemic absorption of local anesthetic occurs faster. This can lead to toxic plasma levels and a shorter duration of block.
NYSORA Tips
- Compared to older children, the sacral hiatus in neo-nates is located more cephalad, and the dural sac ends lower, increasing the risk of accidental dural puncture.
- US imaging can be used to evaluate the neuraxial anat-omy and the approach to the epidural space.
LOCAL ANESTHETICS FOR EPIDURAL ANESTHESIA IN CHILDREN
Since most pediatric patients receive epidural analgesia in conjunction with a general anesthetic, the main purpose of the epidural catheter is to deliver enough local anesthetic solution for effective intraoperative and postoperative analgesia. As with epidural anesthesia in adults, local anesthetic concentration and volume are important factors in determining the density and level of block. However, in pediatric patients, knowledge of total drug dose is also important to avoid local anesthetic toxicity. A more detailed description of local anesthetic solutions, their characteristics, and toxicity potential has been described in Clinical Pharmacology of Local Anesthetics.
Bupivacaine, ropivacaine, and levobupivacaine are the most commonly used local anesthetics for neuraxial anesthesia in children. Lidocaine is not often used because of its excessive motor block. As a general rule, high concentrations of local anesthetics, such as 0.5% bupivacaine or 0.5% ropivacaine, are seldom used in epidural blocks in children. Instead, larger volumes of more dilute local anesthetic are more commonly used to cover multiple dermatomes. Body weight is usually a better correlation than patient age in predicting spread of local anesthetic after a caudal block. The maximal safe dose of bupivacaine is 2.5 mg/kg. For caudal use, the optimum concentration of bupivacaine is 0.125%–0.175%. Compared with the 0.25% preparation, this concentration provides a similar dura-tion of postoperative analgesia (4–8 hours) but with less motor block. Some clinicians prefer administering doses on a volume-per-weight basis. A dose of 1.0 mL/kg of a dilute solution, such as 0.125% bupivacaine, to a maximum volume of 20 mL can sometimes provide T10 sensory block without exceeding the maximum levels recommended in the literature. In infants, higher volumes, such as 1.25 mL/kg or even 1.5 mL/kg, may be administered to provide a more cephalad block without the risk of local anesthetic toxicity. For continuous epidural infusion, a commonly accepted dosage guideline for bupivacaine is 0.2 mg/kg/h for neonates and 0.4 mg/kg/h for older children. Cumulative toxicity is a concern even at lower rates of local anesthetic solution infusions. Therefore, duration of neonatal epidural infusions should be limited to 48 hours.
Ropivacaine has a higher therapeutic index than the older local anesthetic bupivacaine. At low concentrations, ropivacaine may produce less motor block and equivalent analgesia compared to bupivacaine with a decreased incidence of cardiac and central nervous system toxicity. Because of its possible vasoconstricting properties, ropivacaine may undergo slower systemic absorption than bupivacaine. This may have clinical implications when a prolonged local anesthetic infusion is used in children with impaired hepatic function. For a single-injection caudal block, a bolus of 1 mL/kg of 0.2% ropivacaine is recommended. An infusion of 0.1% ropivacaine at 0.2 mg/kg/h in infants and 0.4 mg/kg/h in older children, lasting no longer than 48 hours, has also been shown to be effective and safe.
Levobupivacaine, the S (–)-isomer of bupivacaine, is less likely to cause myocardial depression and fatal arrhythmias and is also less toxic to the central nervous system than racemic bupivacaine. A dose of 0.8 mL/kg of 0.25% levobupivacaine injected caudally provides analgesia in children having penile or groin surgery. For continuous epidural infusion, the dose for levobupivacaine is similar to that for racemic bupivacaine.
NYSORA Tips
- High concentrations of local anesthetic, such as 0.5% bupivacaine or 0.5% ropivacaine, are not recommended in the pediatric population. As the myelination is not complete, lower concentrations of amino amide local anesthetics are effective (eg, 0.125% levobupivacaine).
- Instead, larger volumes of more dilute local anesthetics are more commonly used to cover several dermatomes of interest.
- In the pediatric patients, body weight provides a better correlation than patient age in predicting spread of local anesthetic after a caudal block.
- A simple rule for a caudal single injection in children under 20 kg is to use bupivacaine 0.125%–0.175% or ropiva-caine 0.2% and give a bolus of one of the following:
- 0.5 ml/kg to achieve a sacral surgical level
- 1.0 ml/kg to achieve a high lumbar surgical level
- 1.25 ml/kg to achieve a low thoracic surgical level
- For continuous epidural infusion, bupivacaine 0.125% at a rate of 0.2 mg/kg/h for neonates and 0.4 mg/kg/h for older children is often used. Ropivacaine 0.1% at a rate of 0.2 mg/kg/h for neonates and 0.4 mg/kg/h for older children for 48 hours has been shown to be an effective and safe regimen.
ADJUVANTS FOR EPIDURAL ANESTHESIA IN CHILDREN
A single-injection caudal block with local anesthetic is used primarily for minor surgery because of its limited duration of analgesia. Adjuvants may be used to prolong the duration of block, and several drugs have been trialed. The most commonly used adjuvant to local anesthetics has been epinephrine. Epinephrine in a concentration of 1:200,000 is used to decrease the absorption rate of local anesthetic and has the added benefit of serving as a possible marker for an inadvertent intravascular injection. Recent research has focused on the use of a multitude of adjuvants. Midazolam and neostigmine have also been studied; however, there is no evidence that these drugs provide any analgesic benefit when administered epidurally. Opioids, clonidine, and ketamine all deserve more consideration and will therefore discussed in greater detail.
Opioids
Epidural opioids may enhance the effect of local anesthetics and prolong analgesia. However, some opioids may not be advisable in an ambulatory setting because of the potential for respiratory depression and other unacceptable side effects (eg, nausea and vomiting, itching, urinary retention). As a result, the use of caudal epidural opioids in children should be restricted to special clinical situations outside the outpatient setting. A dose of 2 mcg/kg of fentanyl for single-injection caudal anesthesia along with the standard local anesthetic solution has been recommended for more extensive or painful procedures and in patients who have a urinary catheter in the postoperative period. The addition of 1–2 mcg/mL fentanyl to 0.1% bupivacaine for continuous epidural infusions has also been used with success in children in a well-monitored inpatient setting. However, fentanyl should not be used in neonatal epidural infusions.Epidural morphine may also be used for inpatients undergoing major abdominal or thoracic surgery. When added to single-injection caudal epidural blocks, it will enhance the level of block because of its rostral dispersion (as morphine is a hydrophilic molecule). Doses of caudal morphine vary from 30–90 mcg/kg depending on the type of surgery. Epidural morphine carries a potential risk for respiratory depression; therefore, continuous pulse oximetry is recommended with lower doses of caudal morphine and is mandatory with medium doses. When higher doses of caudal morphine are used, postoperative admission to intensive care must be planned.
Clonidine
Of the various nonopioid adjuncts used in epidural blocks in children, clonidine offers the best profile. Clonidine is an α1-agonist and acts by stimulating the descending noradrenergic medullospinal pathways, which inhibits the release of nociceptive neurotransmitters in the dorsal horn of the spinal cord. The addition of clonidine (1–5 mcg/kg) can improve the analgesic effect of local anesthetics for single-injection caudal block and prolong the local anesthetic duration of action without the unwanted side effects of epidural opioids. For continuous epidural infusions, clonidine 0.1 mcg/kg/h has been used with good effect. It should be cautioned that higher doses have been associated with sedation and hemodynamic instability in the form of hypotension and bradycardia. With bolus doses of 2 mcg/kg, these side effects are unusual. In addition, epidural clonidine blunts the ventilatory response to increasing levels of end-tidal carbon dioxide (PCO2). Although respiratory depression does not appear to be a common problem, apnea has been reported in a term neonate who received a caudal block consisting of 1 mL/kg of 0.2% ropivacaine with clonidine 2 mcg/kg. Caution should be exercised when using clonidine in very young infants because of the sedation and hypotension that may ensue.
Ketamine
The addition of S-ketamine to a single-injection caudal block prolongs the analgesic effect of local anesthetics. The main disadvantages of ketamine are its psychomimetic effects. However, at small doses (0.25–0.5 mg/kg), ketamine is effective without noticeable behavioral side effects. Ketamine 1 mg/kg can also be used as an effective caudal analgesic solely without the addition of local anesthetic solution. The combination of S (+)-ketamine (0.5–1 mg/kg) and clonidine (1 or 2 mcg/kg) has been shown to provide effective analgesia after inguinal herniotomy in children with a prolonged duration of effect (> 20 hours) without any adverse central nervous system (CNS) effects or motor impairment. One concern regarding the use of ketamine in neonates relates to a controversial series of animal studies suggesting that ketamine can produce apoptotic neurodegeneration in the developing brain. Other infant animal studies have demonstrated that ketamine may have a neuroprotective effect. Nevertheless, many anesthesiologists are hesitant to introduce caudal S-ketamine into their routine clinical practice, and ketamine is unlikely to be widely adopted in countries where preservative-free formulas are unavailable.
COMPLICATIONS ASSOCIATED WITH EPIDURAL ANESTHESIA
Major complications from either single-injection or continuous epidural blocks are rare if proper technique is used.
Neurologic Injury
A large prospective study, which summarized data from over 15,000 central blocks in children, reported no incidence of permanent neurologic injuries and concluded that the incidence of complications is rare. However, three infant deaths and two other incidences of paraplegia and quadriplegia were reported in another large retrospective report published in 1995 with over 24,000 epidural blocks in children. This study also reported two cases of transient paresthesia. Although the overall risk seems low, devastating complications from direct damage to the spinal cord can occur, particularly with thoracic and high lumbar epidural needle placement. In addition, hypotension can compromise spinal perfusion. Because the placement of epidural needles and catheters is usually performed with the patient under sedation or general anesthesia, the fact that unconscious patients are unable to report pain or paresthesia (the currently accepted warning sign of needle encroachment on the spinal cord) raises concern. Keeping the patient spontaneously breathing while performing the neuraxial block has been suggested as a safety measure. Preprocedural US scanning of the neuraxial anatomy where available is highly recommended to assess depth to the epidural space.
A case report of spinal cord injury after placing a single-injection thoracic epidural under general anesthesia for appendectomy highlights the importance of the routine assessment of the risk–benefit ratio of placing a direct thoracic epidural for less extensive surgery. In particular, the use of thoracic and high lumbar epidural catheter placement should be reserved only for extensive thoracic and abdominal procedures and should be performed by anesthesiologists with experience in thoracic epidural placement.To minimize the risk of spinal cord injury (and the risk of dural puncture), knowledge of the expected depth of the epidural space is important. As a general rule, the epidural space in children weighing more than 10 kg is found at 1 mm/kg of body weight. There are other formulas based on the patient’s body weight or age to calculate this depth. However, the best option is to measure the depth by preprocedural US imaging of the neuraxial anatomy (Table 1)
NYSORA Tips
As a general rule, the epidural space in children weigh-ing more than 10 kg is found at a depth of 1 mm/kg of body weight. However, preprocedural US imaging is useful to determine the depth of the epidural space.
TABLE 1. Formulas to determine depth of epidural space from skin.
| Note: | An individual preprocedural ultrasound assessment is the preferred method of determining the depth of epidural space from the skin. |
| 1. Rough estimate: 1 mm/kg body weight | |
| 2. Depth (cm) = 1 + (0.15 × age in years) | |
| 3. Depth (cm) = 0.8 + (0.05 × weight in kilograms) |
Epidural Hematoma
Epidural hematoma associated with epidural analgesia in chil-dren is rare. This may be because anticoagulation protocols are rarely indicated during the perioperative period in pediatric patients. Nonetheless, epidural analgesia should be avoided in patients with clinically significant coagulopathy or thrombocytopenia. Guidelines for the use of epidural anesthesia in adult patients should also be applied in pediatric patients receiving antithrombotic or thrombolytic therapy.
Infection
Although the overall infection rate associated with caudal epidural catheters appears to be low, isolated case reports exist of infection related to epidural catheters in children. Compared with lumbar epidural catheters, there is some concern regarding catheter infection with the prolonged use of caudally placed catheters owing to the proximity of the sacral hiatus to the rectum. Although studies have not found clinical evidence of higher infection rates with the caudal approach, bacterial colonization has been reported to be higher. Staphylococcus epidermidis is the predominant microorganism colonized on the skin and catheters of lumbar and caudal epidurals. Gram-negative bacteria have also been found on the tips of caudal catheters. Even with widely used single-injection caudal blocks, infections such as sacral osteomyelitis can still occur. To reduce the risk of contamination by stool and urine, techniques such as catheter tunneling and fixing the catheter with occlusive dressing in a cephalad direction can be used. A strict aseptic technique including the use of a sterile closed-infusion system should also be used, and care should be taken to avoid local tissue trauma. Daily inspection of the dressing and entry site is also important, although the dressing should not be changed unless strictly necessary. If the child develops a persistent fever greater than 38°C of unknown origin, the catheter should be removed and sent for culture.
Dural Puncture and Postdural Puncture Headache
Dural puncture during caudal epidural analgesia is uncommon if caution is taken to avoid advancing the needle too far into the sacral canal. The use of real-time US imaging to control needle position makes this risk extremely low. Treatment for postdural puncture headache (PDPH) includes bed rest, oral or intravenous (IV) hydration, analgesia (eg, regular acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]), and anti-emetics. Bed rest, although relieving the severity of the headache, has no effect on the incidence or duration of PDPH.
In adults, caffeine has been used for both the prophylaxis and treatment of PDPH. Caffeine causes cerebral vasoconstric-tion by blocking adenosine receptors, which dilate vessels when activated. Reducing cerebral blood flow decreases the amount of blood in the brain and may lessen the traction on pain-sensitive intracranial structures, thus relieving PDPH. However, caffeine is not frequently used in children for relief of PDPH, and an optimal dose is unknown.The use of epidural blood patch to treat PDPH has been used with success in adults since 1960. There are now many reports of its successful use in children as well. An epidural blood patch is thought to be effective through the formation of a gelatinous cover over the dural hole by the injected blood. In the short term, the epidural blood patch seals the hole and relieves CSF hypotension both by mass effect from CSF cranial displacement and by increasing intracranial volume and presure. Actual healing takes place over the longer term. In children, it is recommended that approximately 0.3 mL/kg of autologous blood be injected in the awake or mildly sedated patient, if possible, to detect the appearance of radicular symptoms. A more complete discussion on PDPH is presented in Postdural Puncture Headache.
Hemodynamic Effects and Total Spinal Anesthesia
Significant changes in blood pressure are uncommon in pediatric patients after the accurate administration of epidural analgesia. A high sympathetic single-injection caudal block to T6 has been found to evoke no significant changes in heart rate, cardiac index, or blood pressure in children. Even when thoracic epidural block is combined with general anesthesia, cardiovacular stability is usually maintained in otherwise healthy pediatric patients. Therefore, hypotension should raise the suspicion of total spinal anesthesia and/or an intravascular injection leading to local anesthetic toxicity. After these complications are ruled out, other causes, such as hydration status, intravascular filling pressure, and inotropic state, and the depth of anesthesia should be assessed.
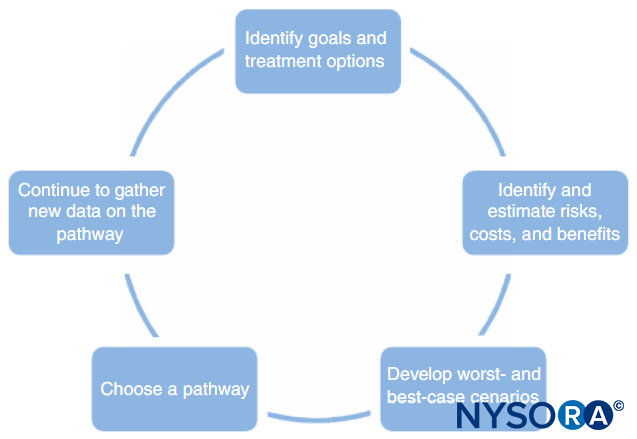
If total spinal anesthesia has occurred, supportive measures must be provided until the effect of the block has dissipated. However, in the event of a life-threatening extension of a total spinal anesthesia, if attempted supportive measures are neither effective nor an option, cerebrospinal lavage may be considered as a last maneuver. A case report has suggested that 20–30 mL of CSF can be withdrawn and replaced with 30–40 mL of preservative-free normal saline, Ringer’s lactate, or Plasmalyte via the epidural catheter. This intervention may shorten recovery time, minimize the potential neurotoxic insult, and reduce the incidence of postdural puncture. However, in light of the limited experience and information on cerebrospinal lavage, the potential risks and benefits should be evaluated on a case-by-case basis before using this technique in children.
NYSORA Tips
- Epidural anesthesia and analgesia in otherwise healthy children rarely causes cardiovascular instability.
- The occurrence of hypotension should raise the suspicion of total spinal anesthesia and/or an intravascular injection leading to local anesthetic toxicity.
- After these complications are ruled out, other causes, such as hydration status, intravascular filling pressure, and inotropic state, and the depth of anesthesia should be assessed.
Local Anesthetic Systemic Toxicity
Local anesthetic systemic toxicity (LAST) often stems from accidental intravascular injection into epidural blood vessels. This complication can often be avoided by using careful aspiration and test dosing. Table 2 summarizes recommendations for test dosing in epidural block. For a single-injection caudal block, vascular puncture and local anesthetic absorption are more likely to occur when sharp-tipped needles are used. For continuous epidural infusion, neonates and very young infants are at greater risk for local anesthetic toxicity than older children. Seizures have been reported in children receiving cotinuous infusions of local anesthetics. This can be avoided by using dilute solutions of local anesthetics (≤ 0.125% bupivacaine) and by following current dosing recommendations (see “Local Anesthetics for Epidural Anesthesia in Children,” above).
More importantly, vigilant monitoring during the administration of epidural analgesia should be a priority. Guidelines for LAST treatment should be readily accessible in all hospital areas where local anesthetics are used. All personnel of wards where patients undergoing epidural infusion are cared for should be trained in the recognition of symptoms and treatment of LAST. In addition, a complete record of the regional technique and infusion used in each case should be present alongside the patient’s observations chart.
TABLE 2. Test dosing for epidural block.
| 1. | Use test dosing routinely, even though test dosing for all available agents is not 100% sensitive. In addition, because the true incidence of intravascular placement is relatively low, most positive tests (ie, heart rate increases) will be false-positives. When there is a borderline response, repeating the test dose increases the specificity and sensitivity of the test. |
| 2. | Continuously monitor the ECG, and cycle the blood pressure cuff repeatedly. With epinephrine-containing solutions, if the heart rate does not increase, an increase in blood pressure should raise suspicion of intravascular placement. |
| 3. | Avoid performing test dosing when the child is in a very light plane of anesthesia or when there is stimulation (eg, repo-sitioning the patient on the operating table, instrumentation of the airway, incision). Performing the test dose under these conditions increases the likelihood of false-positive, stimulation-induced increases in heart rate or blood pressure. |
| 4. | After the test dose, the remainder of the full dose should be administered incrementally. Incremental dosing and con-tinuous monitoring help increase the odds that an intravascular placement will be detected and that further injection will be halted before full cardiodepressant doses are administered. |
| 5. | Whenever possible, keep the patient under spontaneous ventilation throughout the placement and initial dosing of the epidural block. Any change in the patient’s breathing pattern is an alert that an inadvertent intravascular or intra-thecal injection may have taken place: tachypnea if pain on injection; respiratory depression if there has been systemic absorption of local anesthetic; or tachypnea followed by bradypnea caused by total spinal anesthesia if local anesthetic has been administerd intrathecally. |
Other Adverse Effects
In a retrospective review based on prospective collected data from 286 pediatric patients, pruritus (26.1%), nausea and vomiting (16.9%), and urinary retention (20.8%) were the most common side effects encountered during epidural anesthesia using an infusion of bupivacaine and fentanyl. Sedation and excessive block each occurred in less than 2% of patients. The incidence of respiratory depression was 4.2%, but the administration of naloxone for severe respiratory depression was never necessary. Perforation of the rectum may occur if the caudal needle is angled too steeply. Table 3 summarizes the recommended treatments for common adverse effects.
TABLE 3. Summary of recommended treatments of effects in epidural blocks.
| Itching | |
| 1. Exclude and/or correct other remediable causes. | |
| 2. Use low-dose naloxone infusions, partial agonist–antagonists (eg, nalbuphine), or antihistamines. | |
| 3. If itching persists, remove the opioid from the epidural infusion, and consider clonidine. | |
| Nausea | |
| 1. Exclude and/or correct other remediable causes. | |
| 2. Use 5-HT antagonists (eg, ondansetron, dolasetron) | |
| 3. Use low-dose naloxone infusions or nalbuphine | |
| 4. Avoid opioids in infusions, and consider clonidine. | |
| Ileus and bowel dysfunction | |
| 1. Exclude and/or correct other remediable causes. | |
| 2. Give laxatives if not otherwise contraindicated. | |
| 3. Avoid opioids in infusions, and consider clonidine. | |
| 4. Use low-dose naloxone infusions or nalbuphine. | |
| 5. Use peripherally or enterally constrained opioid antagonists; for example, methylnaltrexone or alvimopan (currently investigational). | |
| Sedation or hypoventilation | |
| 1. Exclude and/or correct other remediable causes. | |
| 2. Depending on severity, reduce or hold dosing of opioids or clonidine. | |
| 3. Awaken, stimulate, and encourage deep breathing. | |
| 4. If severe, consider naloxone or assisted ventilation as needed. | |
| Urinary retention | |
| 1. Exclude and/or correct other remediable causes. | |
| 2. Avoid using anticholinergics or antihistaminics if alternatives are available. | |
| 3. Use low-dose naloxone infusions or nalbuphine. | |
| 4. Use bladder catheterization. | |
EPIDURAL block FOR PEDIATRIC SURGERY: TECHNIQUES
Epidural analgesia can be delivered via a single-injection or continuous-infusion technique. The needles and catheters can be inserted at the caudal, lumbar, or thoracic level. The main goal of the epidural technique is to accurately position the needle and/or catheter in the epidural space. Aspiration tests and test doses indicate possible inadvertent intravascular or intrathecal drug administration. Epidural stimulation, epidural electrocardiogram (ECG), and US techniques have been developed in addition to conventional X-ray imaging to assist with accurate epidural needle or catheter placement.
Confirmation of Proper Epidural Needle or Catheter Placement
Aspiration and Test Dose
An aspiration test performed before local anesthetic injection is used to avoid total spinal and intravascular injections. However, a negative aspiration of blood or CSF should not be considered an absolute indicator of proper needle and catheter placement. Veins are so small they may collapse easily on aspiration; therefore, it is recommended to use a 2-mL syringe, aspirate slowly, and consider opening to air to look for free flow.
The patient’s ECG should be continuously monitored while injecting local anesthetic into the caudal space. The ECG specificity changes (ie, > 25% increase in T wave) after the injection of an epinephrine test dose (0.5 mcg/kg) can help predict intravascular injection.
If possible, the patient should be kept under spontaneous ventilation throughout the placement and initial dosing of the epidural block. Any change in the patient’s breathing pattern is an alert that something might accidentally be happening: respiratory depression if there is systemic absorption of local anesthetic; tachypnea if there is pain on injection; or tachypnea followed by bradypnea if there has been an intratecal administration of local anesthetic (see Table 2). Table 4 summarizes various methods for confirming epidural catheter placement.
TABLE 4. Confirmation of epidural catheter position.
| Intraoperatively (while the patient is under general anesthesia) |
| 1. Ultrasonography is highly recommended to assess the spread of local anesthetic at the tip of catheter or within the epidural space. |
| 2. Ensure negative aspiration; inject the local anesthetic slowly in small increments through the catheter; and evaluate response to surgery. If possible, maintain spontaneous ventilation. |
| 3. Radiography with contrast. |
| 4. Electrical stimulation and/or ECG technique. |
| Postoperatively (while the patient is awake, whether or not he or she can give verbal responses) |
| 1. Ultrasonography is the currently recommended method. This is painless and can be done in the PACU without bothering the child too much. |
| 2. If US is not available, the chloroprocaine test can be used. This involves incremental dosing of a chloro-procaine 3% solution to demonstrate analgesia (by self-report or behavioral measures as appropriate) and signs of segmental effect: a. Lumbar catheter tip: • At least partial sensory and motor block in both legs • Warming of the volar surface of the toes b. Lower thoracic catheter tip: • Reduced strength in hip flexion • Reduced abdominal skin reflexes • Some reduction in heart rate and blood pressure c. Upper thoracic catheter tip: • Some reduction in heart rate and blood pressure • Warming of the volar surface of the hands • Unilateral or bilateral Horner syndrome |
Radiographic Methods
X-ray imaging in conjunction with a contrasting agent precisely identifies the tip of the catheter at a specific spinal level.
A radiograph without contrast, however, cannot distinguish inadvertent intrathecal or subdural catheter placement from correct epidural placement. In addition, standard X-ray does not allow the anesthesiologist to adjust the position of the catheter during insertion unless fluoroscopy is used. Although fluoroscopy allows for real-time monitoring and adjustment of advancing catheters, it requires additional setup, incurs increased expense, and increases the patient’s exposure to ionizing radiation. As a result, fluoroscopy is not routinely recommended and is usually limited to difficult and/or special circumstances, such as longterm epidural catheter placement for cancer pain.
Epidural Stimulation Test (Tsui Test) and Epidural ECG Technique
A low-current electrical stimulation test (the Tsui test; Figure 1) has been suggested to monitor and guide the position of the epidural catheter during insertion. The set-up requires the cathode lead (black for block) of the nerve stimulator to be connected to the epidural catheter via an electrode adapter while the anode lead is connected to an electrode on the patient’s skin as the grounding site. To avoid misinterpretation of the stimulation response (eg, a local muscle contraction may be confused with epidural stimulation), the grounded electrode is placed on the lower extremity for thoracic epidurals and on the upper extremity for lumbar epidurals. Correct placement of the epidural catheter tip (1–2 cm from the nerve roots) is indicated by a motor response elicited with a current between 1 mA and 10 mA. A motor response observed with a significantly lower threshold current (< 1 mA) suggests that the catheter is in the subarachnoid or subdural space or is in close proximity to a nerve root. Although chronic spinal cord stimulation is a safe and effective means of pain management, the safety of this epidural stimulation test is not completely known. However, it is anticipated that the risk of a brief intermittent electrical stimulation from this test is minimal. Table 5 summarizes the different catheter locations according to motor response and electrical current.
TABLE 5. Electrical stimulation test.
| Catheter Location | Motor Response | Current |
|---|---|---|
| Subcutaneous | None | > 10 mA |
| Subdural | Bilateral (many segments) | < 1 mA |
| Subarachnoid | Unilateral or bilateral | < 1 mA |
| Epidural space | ||
| - Against nerve root | Unilateral | < 1 mA |
| - Nonintravascular | Unilateral or bilateral | 1–10 mA (threshold current increase after LA injection) |
| - Intravascular | Unilateral or bilateral | 1–10 mA (no change in threshold current after LA injection) |
One disadvantage of the epidural stimulation technique is that it cannot reliably be performed if any significant clinical neuromuscular block is present or if local anesthetics have been administered in the epidural space. To overcome this limitation, an alternative monitoring technique using ECG monitoring has been suggested. A reference ECG is monitored at the required spinal level for surgery; this is then compared to the ECG formed from the epidural catheter tip as it is threaded cephalad. Unfortunately, this technique cannot easily differentiate subtle QRS complexes where the catheter is threaded a short distance; neither does it recognize intravascular or intrathecal catheter positioning.
Ultrasound-Guided Techniques
Since the main goal of an epidural block is to accurately place the needle and/or catheter in the epidural space, knowledge of the expected depth from the skin surface to the epidural space is extremely important. Table 1 summarizes some formulas to calculate this depth in children. Where available, US allows for the real-time identification of anatomical landmarks and a much more precise estimation of epidural space depth. It is highly recommended to scan the anatomy with ultrasonography in all children before performing the block and especially in difficult cases, such as patients with scoliosis or sacral dimples. US also allows for needle visualization within the epidural space in neonates. In infants, US can detect epidural catheter advancement, either directly or indirectly by observing the injection of fluid.
Epidural Approaches
The most common types of epidural analgesia are caudal analgesia (which constitutes the most commonly used regional technique in children), lumbar epidural analgesia, and thoracic epidural analgesia.
Caudal Epidural Analgesia: Single-Injection Technique
Single-injection caudal epidural block is widely used to provide perioperative analgesia in pediatric practice. As a single injection, it offers a reliable and effective block for patients undergoing urologic, general, and orthopedic surgery involving the lower abdomen and lower limbs. A single-injection caudal epidural may not be suitable for every case because it has a limited dermatomal distribution and a short duration of action. New local anesthetics and adjuvants, as well as continuous catheter approaches, may overcome these limitations.
Choice of Needle for Caudal Analgesia
A variety of needles are available for single-injection caudal block. The size or type of needle does not appear to affect the rate of success or the incidence of complications of caudal block. Short-bevel Tuohy or Crawford needles (5 cm in length) with stylets offer a better tactile sensation when the sacrococcygeal ligament is punctured. For children aged 1 year or older, a 22-gauge needle is used; for children younger than 1 year of age, a 25-gauge needle may be used. The use of a styletted needle may reduce the risk of introducing a dermal plug into the caudal space, although an epidermal cell graft tumor in the epidural space has yet to be reported. Some authors advocate the use of a 22-gauge angiocath, suggesting that it is easier to detect intravascular placement and intraosseous placement with this needle. The angiocath is used only for the single-injection caudal block and is withdrawn after the dose is administered (ie, it is not intended to be an epidural caudal catheter). To avoid tissue coring with the angiocath, the needle must be removed before any injection is made.
Technique for Performing a Single-Injection Caudal Epidural Block
In all children, it is important to ensure adequate prevention of heat loss during the proce-dure. In infants, we recommend preventing heat loss with a sterile transparent drape as this will also allow visualization of patient’s breathing (Figure 2). The patient is placed in a lateral decubitus position with the neck flexed and the knees drawn up to the chest. After proper positioning, the landmarks for caudal epidural block (Figure 3) are easily identified in children: Initially the coccyx is identified, and, continuing to palpate in the midline in a cephalad fashion, the sacral cornua can be felt on either side of the midline approximately 1 cm apart. The sacral hiatus is felt as a depression between two bony prominences of the sacral cornua. Under sterile conditions, the needle is inserted and advanced into the sacral hiatus at approximately a 70-degree angle to the skin until a distinctive “pop” is felt as the sacrococcygeal ligament is punctured. After this puncture, the angle of the needle should be reduced to approximately 20–30 degrees while the needle is advanced 2–4 mm into the caudal canal. Any advancement past this point is not recommended because the risk of inadvertent dural puncture increases significantly. If an angiocath is used, the plastic catheter should be easily advanced over the needle into the caudal epidural space.

FIGURE 2. Transparent cover used in neonates and infants to allow for visualization of the patient and to prevent heat loss. The US machine is placed on the opposite side.
NYSORA Tips
Care should be taken to ensure the prevention of heat loss during the procedure.
US can be used to assess the caudal anatomy prior to the landmark-based technique or to guide needle placement. Pre-assessment is particularly useful in screening children with cutaneous stigmata of spinal dysraphism. The patient is placed in the lateral decubitus position with the knees flexed toward the chest. The US machine is placed opposite the operator so that he or she can look over his or her hands toward the screen. The patient is prepared, and the US probe is sterilely covered. A high-frequency probe is used: A linear hockey-stick probe is used in infants, whereas a probe with a large footprint is preferable in children weighing more than 10 kg, as it allows more intervertebral spaces to be imaged at a time in the sagittal plane.
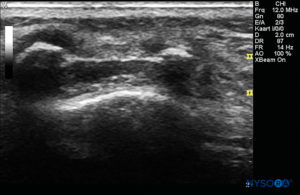
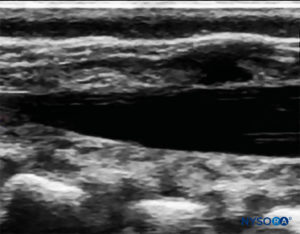
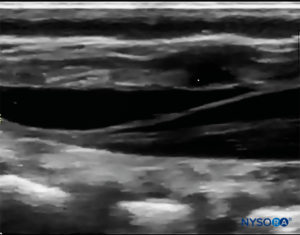
The probe is positioned first in a transverse plane at the sacrum level; this is called the short-axis view (SAX). The exact position of the cornua and the sacrococcygeal membrane (SCM) are defined (Figure 4). With the sacrococcygeal membrane in the middle of the image (Figure 5), the probe is then rotated 90 degrees into a midline sagittal position over the lower sacrum, which is called the long-axis view (LAX; Figure 6). The SCM and the ventral and dorsal layer of the os sacrum, with the caudal epidural space in between, are easily identified. In small children, the dural sac may be visible in this position, although in older children you need to scan more in a more cephalad direction (Figure 7). These movements can be performed in the opposite order, but a complete exploration of the space in both axes is recommended.
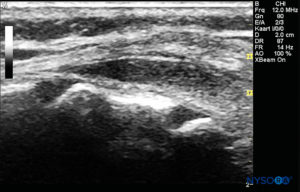
FIGURE 7. US image in the long-axis view showing the sacrococcygeal membrane and caudal epidural space in the os sacrum
After this preprocedural US assessment of the caudal anatomy, the needle can be introduced into the sacral hiatus with the probe in either axis. If the probe is held in the SAX, the needle insertion will be automatically in the out-of-plane (OOP) approach (Figure 8). If the probe is held in the LAX, the needle insertion will then be in the in-plane (IP) approach (Figure 9).
The needle insertion angle is noted during the scan. The needle may be advanced 2–4 mm into the caudal space, and the stylet is removed. To ensure optimal caudal placement of the needle, a small bolus of saline or local anesthetic is administered under US guidance with the probe in the midline (LAX; Figure 10). The probe is positioned as cephalic as needed to visualize the dural sac in the US screen (Figure 11). When the injection starts, you will notice the dura being displaced ventrally, especially in younger children. The spread of local anesthetic can be monitored by moving the probe cephalic up the spine in the midline or in a paramedian sagittal axis (Figure 12). The same dura movement can be visualized with the probe in the SAX in the more cephalic positions (Figures 13 and 14).
Confirmation of Correct Local Anesthetic Distribution
The classic “pop” felt as the SCM is pierced is usually sought to confirm proper caudal needle placement. The absence of subcutaneous bulging and the lack of resistance upon injection are additional signs of correct needle placement and local anesthetic distribution. Aspiration of the needle should be clear of blood and CSF, and a negative response to a test dose of epinephrine should also be used to rule out intravascular placement. US has been used to provide real-time needle guidance into the caudal space and to assess the spread of local anesthetic. Recent US studies have shown that the volume of local anesthetic does not correlate with its cranial spread during caudal block in infants and children. Initially, US assessment of the spread of local anesthetic was thought to be a predictor of the dermatome reached, but this proved not to be the case as the majority of caudal blocks are successful despite an immediately monitored lack of spread cephalad. However, it has been found that there is a secondary spread of local anesthetic in the epidural space. This occurs in two patterns: a horizontal intrasegmental redistribution from the dorsal to ventral epidural space and a delayed longitudinal cranial spread as the dura returns to its original position, thus pushing the epidural local anesthetic cephalad. The observed bidirectional movement of CSF (referred to as the “CSF rebound mechanism”) also helps explain a component of the difference between the initial US-assessed spread and the final more cephalad effect determined by cutaneous testing. More studies with ultrasonography are needed to determine how best to predict in the spread of local anesthetic.
Caudal Epidural Analgesia: Continuous Technique
Continuous caudal epidural analgesia overcomes the limited duration and segmental effect of a single-injection technique. Caudal catheters can be advanced to the lumbar or thoracic level. The technique for needle insertion for continuous caudal analgesia is very similar to the single-injection caudal approach. It can be done with an IV catheter (an 18-gauge angiocatheter for a 20-gauge epidural catheter or a 16-gauge angiocatheter for a 19-gauge epidural catheter) or with an 18-gauge Crawford or Tuohy needle inserted through the sacrococcygeal membrane, as described for the single-injection technique. The epidural catheter is then advanced carefully from the caudal space to the target level. Minor resistance to the passage of the catheter can usually be overcome by simple flexion or extension of the patient’s vertebral column and/or by simultaneously injecting normal saline through the catheter. Some authors use a specialized stimulation epidural catheter (the Epidural Positioning System using the Tsui test, Arrow International Inc., Reading, PA).
It is extremely important to know where the tip of the catheter is finally located: too low a catheter tip level will result in poor analgesia; too high may cause respiratory depression. However, because catheters don’t travel linearly in the epidural space, measuring the length of the catheter against the patient’s back does not accurately determine the targeted surgical level. Therefore, the location of the catheter tip should be verified using an objective test, as described as in the previous section (ie, radiography, nerve stimulation, electrocardiography, or, preferably, US).
These techniques may be considered cumbersome or redundant, and in children above 1 year of age, the development of a lumbar curve during infancy might prevent easy cephalad advancement of the catheter. Therefore, some have suggested that caudal catheter placement should be limited to patients younger than 1 year of age. It is the opinion of the authors that, at least in children older than 1 year of age, catheters should be placed as close to the surgical dermatome as possible. Appropriate pediatric and ultrasonographic training is therefore recommended in all cases and mandatory prior to performing lumbar or thoracic epidurals in young children.
Lumbar Epidural Anesthesia
Lumbar epidural analgesia is commonly used for continuous infusions and is rarely used as a single-injection technique. A direct lumbar approach is indicated primarily for pain control during and after lower extremity surgery. Lumbar epidural placement, particularly in young children, is performed after the induction of general anesthesia. However, this approach may also be performed awake in a select group of cooperative children and adolescents. Caution should be exercised whenever performing lumbar epidural analgesia above the level of spinal cord end to avoid direct needle trauma.
A midline approach to lumbar epidural needle placement is preferred. Identification of the epidural space is commonly achieved by loss of resistance (LOR) to saline. LOR to air should be avoided due to the risk of introducing a venous air embolism, particularly in neonates and infants. Children should be positioned in the lateral decubitus position for direct lumbar epidural placement. In children over 1 year of age, an 18-gauge, 5-cm Tuohy needle, marked every 0.5 cm, with a 20-gauge epidural catheter is often used. In children under 1 year of age, a 20-gauge, 5-cm Tuohy needle, marked every 0.5 cm, with a 22-gauge catheter should be considered. However, these narrower catheters get kinked, occlude, and leak more often. Although identification of the intervertebral space and ligamentum flavum in most pediatric patients is easy, the ligamentum flavum can be less tensile in children; hence a distinctive “pop” may not be easily felt when penetrating this layer. In addition, the distance from the skin to the epidural space can be very superficial. Formulas for estimating the distance from skin to epidural space have been proposed (see Table 1). However, formulas are only a guideline and change according to the angle of epidural needle placement. Today, the best available method to assess the epidural depth is US imaging. With the probe in a paramedian oblique sagittal plane, the distance from the skin to the ligamentum flavum is measured with the US machine’s caliper. This measurement provides a good estimate of the depth at which the LOR is going to be felt. Therefore, a preprocedural US assessment of each individual patient is highly recommended.
For an exact description of the lumbar epidural technique, see “Thoracic Epidural Anesthesia,” below (figures illustrate a thoracic epidural placement).
Lumbar-to-Thoracic Epidural Approach
Catheters placed via the lumbar route may be advanced cephalad to thoracic vertebral levels. Similar to the problems encountered when advancing catheters in the caudal space in older children, significant resistance also prevents the easy advancement of lumbar epidural catheters to the thoracic levels. Despite favorable results using stimulation via a caudal approach, only one case report has demonstrated the successful placement of a thoracic epidural catheter via the lumbar route with epidural stimulation guidance. Therefore, the authors recommend placing the catheter as close as possible to the surgical site.
Thoracic Epidural Analgesia
Controversy exists concerning the safety of placing thoracic epidurals under heavy sedation or general anesthesia, because unconscious patients are unable to report symptoms that may warn the anesthesiologist of potential neurologic complications Direct needle trauma to the spinal cord during epidural insertion is rare but can cause devastating complications. Reports have detailed cases of direct needle trauma to the spinal cord during epidural placement in both awake and anesthetized patients. For thoracic surgery, the catheter should be introduced as close to the dermatomal level of incision as is possible.
The advancement of catheters from the lumbar and caudal epidural spaces to the thoracic level is an alternative only in children upto 1 year of age. However, the advancement of catheters in the epidural space becomes increasingly difficult with advancing age because of the development of the lumbar curvature.
Direct placement of thoracic epidural catheters is more common at tertiary care centers, where well-trained pediatric anesthesiologists perform the blocks on children undergoing major surgery. Preprocedural ultrasonography imaging is strongly recommended. Moreover, the authors believe that training in US-assisted thoracic epidurals should be provided for anesthesiologists willing to perform thoracic epidurals in children.
NYSORA Tips
- Children require a significantly higher volume (dose) of local anesthetic compared with adults to achieve the same dermatomal spread.
- Intended high thoracic catheter advancement from a lumbar insertion site is rarely successful.
- Thoracic epidural catheter insertion should be performed only by practitioners experienced in pediatric thoracic epidural technique.
- Epidural needle insertion in pediatric patients can be performed at any thoracic interspace using either a mid-line or paramedian approach; however, a midline approach is often preferred.
Thoracic Epidural Analgesia: Midline Approach
The use of the midline approach offers the advantage of being similar to the lumbar approach (with the needle angulated in only one plane). Using the midline approach, insertion of the needle is easier at the lower thoracic level (T10–T12) than at the midthoracic (T4–T7) level. The lower border of the shoulder blade, which is level with the seventh thoracic vertebra, is commonly used as an anatomical landmark. The patient is placed in the lateral decubitus position, and care is taken to prevent heat loss. An assessment of the patient’s anatomy may be done in a nonsterile set-up before the block is performed; this is also helpful for teaching purposes.
The spinous process of the targeted vertebral level should be identified by counting up from Tuffier’s line and by counting down from the most prominent C7 cervical vertebra (Figure 15). Preprocedural US imaging is performed with the probe in three planes: transverse (SAX), median sagittal (median LAX), and paramedian oblique sagittal (paramedian oblique LAX). The distance from the patient’s skin to the epidural space can thus be measured.In the SAX (Figure 16), the window between two spinous processes must be found, and the anterior complex of the vertebral column (posterior longitudinal ligament, anterior dura, and vertebral body) in the depth of the image will be the first structures to be identified. The posterior complex (ligamentum flavum and posterior dura) may be more difficult to visualize but will be approximately at the level of the lamina (Figure 17).

FIGURE 16. Preprocedural scanning with nonsterile set-up for teaching purposes; the US probe is in the short-axis view.

FIGURE 17. US image in the short-axis view, showing the posterior complex with the dura (white arrow).
If the patient is an infant, and the bony structures of the vertebral column are not yet fully ossified, a median LAX (Figure 18) provides clear, real-life imaging of the anatomy involved. With this probe position, the spinous process in the image will almost reach the skin (or the top of the US screen). In between the spinous process, the dura mater will be seen as a white double layer; it is found a little less deep than the level at which the posterior complex is found in the SAX (Figure 19).In the paramedian oblique LAX (Figure 20), the transverse process and/or the lamina may be visualized, depending on how far lateral and oblique the probe is placed. The anterior complex is again easily visualized, and most of the time the pia mater can be seen in small children. The characteristic “horse heads” may be found in the image, and the dura mater will be seen in between, at a deeper level (Figure 21). The depth of the dura mater will be more or less equal, as in the SAX and median LAX positions.

FIGURE 18. Preprocedural scanning with nonsterile set-up for teaching purposes; the US probe is in the median long-axis view. The probe must be exactly in the midline, but in this photo, it has been positioned in the paramedian long-axis view to see the direction.

FIGURE 20. Preprocedural scanning with nonsterile set-up for teaching purposes; the US probe is in the paramedian oblique long-axis view. The tilting of the probe can be compared to that shown in Figure 16.
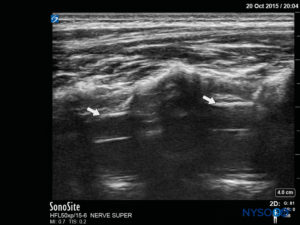
FIGURE 21. US image in the paramedian oblique long-axis view, showing the posterior complex with the dura (white arrows).
After the preprocedural imaging to measure the depth at which the epidural space will be reached, the child’s skin is prepared and draped (Figure 22). An 18-gauge Tuohy epidural needle, 5cm long, with markings every 0.5 cm, is then inserted at the interspace at a cephalad angle of approximately 70 degrees to the longitudinal axis of the spine. A useful maneuver is to insert the needle at a similar angle to that with which the US probe was held when the distance toward the epidural space was measured (Figure 23). Continuous resistance should be felt as the needle is inserted through the supraspinous and interspinous ligaments. When the interspinous ligament is reached, the stylet is removed and a saline-filled LOR syringe is connected to the needle. Continuous pressure is placed on the plunger as the needle is farther advanced (Figure 24). In older children, an increase in resistance is initially felt as the ligamentum flavum is entered, just before the LOR is felt. However, in younger children, the resistance met at the ligamentum flavum may not be noticeably different from that of the other ligaments.

FIGURE 24. Needle advancement with continuous pressure placed on the plunger with the right hand as the left hand advances the needle.
The needle must not be inserted to a depth greater than the preprocedural US–estimated depth of the epidural space. The thoracic epidural space is identified with LOR to saline; air is not recommended in children. The syringe is then removed, and, after ruling out dural puncture, the catheter is inserted (Figure 25). The length of the catheter inserted should be only about 2 cm beyond the needle tip if the epidural puncture has been performed at the appropriate level. If the puncture has been performed one level beneath, the catheter can be inserted up to 3–4 cm, but it must be kept in mind that in small children, a few centimeters may represent several vertebral segments.
After withdrawing the needle and ensuring that an adequate length of catheter is kept in place, the connector is attached to the catheter. At this point, it is imperative to check for a falling meniscus and perform slow and careful aspiration through the catheter to check for blood or CSF (Figure 26). The filter is then connected, and incremental doses of local anesthetic can be administered with the spread assessed under US imaging.
We recommend tunneling the catheter or using a liquid bandage or the topical skin adhesive Histoacryl to close the entrance hole to prevent leakage. Preventing local anesthetic leakage in pediatric patients is important, as leaked anesthetic may consist of a significant percentage of the total drug delivered. Leaking underneath the fixation device or Tegaderm may present a problem for catheter fixation itself. A transparent epidural fixation device is recommended to allow for observation of any local anesthetic leakage or signs of infection (Figure 27).
NYSORA Tips
- Various formulas exist for calculating the volume of local anesthetic required to block a given number of segments.
- A bolus of 1.0 mg/kg of 0.25% bupivacaine or 0.2% ropivacaine is administered to establish the block.
- In preschool-aged children and especially infants, irritability or agitation may occur despite an apparently well-functioning epidural analgesia. This is most likely the result of the IV line, nasogastric tube, urinary catheter, or the hospital environment.
- Satisfactory sedation can be achieved with either of the following:
– IV boluses of morphine 25 mcg/kg as required, or
– Adding clonidine 0.5 mcg/mL to the epidural mixture
POSTOPERATIVE EPIDURAL INFUSION MANAGEMENT
For effective and safe epidural analgesia, a systematic and protocol-based approach to patient care is advised. A dedicated pediatric acute pain team, consisting of anesthesiologists and nurses, is vital to ensure standardized assessments of pain, vigilant patient monitoring, and the proper treatment of adverse effects. Precise placement of epidural needles and catheters is the key to successful epidural analgesia. This requires the use of a reliable method to confirm the location of the catheter tip (ie, US, epidural stimulation). The average length of epidural infusion is about 72 hours, although it may be necessary to continue the infusion for longer periods, especially in children with complicated medical histories or a prolonged need for analgesia. In neonates, the length of epidural infusion should be limited to 48 hours due to the risk of systemic toxicity. A team of dedicated personnel with a focus on pain management should care for such patients. When plans to discontinue the epidural infusion are in place, an opioid should be considered to enable adequate analgesia. Finally, the success of the process is based on properly written orders—a crucial part of executing adequate analgesia.
NYSORA Tips
For postoperative analgesia, either bupivacaine 0.125% or ropivacaine 0.1–0.2%, with or without fentanyl 1–2 mcg/mL, is administered at the following rates:
- Age > 3 months: 0.20–0.35 mL/kg/h (< 0.4 mg/kg/h bupivacaine)
- Age < 3 months: 0.1–0.15 mL/kg/h (< 0.2 mg/kg/h bupivacaine)
SPINAL ANESTHESIA IN CHILDREN
INTRODUCTION
Spinal anesthesia is perhaps one of the oldest and most studied modalities for providing pain relief in patients undergoing surgery. J. Leonard Corning is credited with administering the first spinal anesthetic in 1885, and his experience was subsequently published in a medical journal. Although the use of intrathecal anesthesia administration in children was described in the early twentieth century, this technique was seldom used in the pediatric population until Melman reported a series of high-risk infants who underwent successful surgery under spinal anesthesia. Reports of apnea following general anesthesia in preterm infants appeared in the literature in the early 1980s, and a series from Abajian et al. offered practitioners an impetus to offer an alternative technique with reportedly fewer complications than general anesthesia. A number of series have since been reported in all age groups for a variety of surgical procedures attesting to the safety and efficacy of spinal anesthesia.
TABLE 6. Anatomic differences between adults and infants in the spinal canal.
| Conus medullaris ends at L2–L3 in infants versus L1 in adults. |
| Infants have a small pelvis, and the sacrum begins more cephalad than in adults. |
| The dural sac ends more caudad in infants versus adults. |
ANATOMY
Understanding the anatomical differences between adults and infants is crucial to safely administer spinal anesthesia in children in a technically proficient manner (Table 6). The spinal cord terminates at a much more caudad level in neonates and infants than in adults. The conus medullaris ends at approximately L1 in adults and at the L2 or L3 level in neonates and infants. To avoid potential injury to the spinal cord, dural puncture should be performed below the level of the spinal cord; that is, below L2–L3 in neonates and infants. In adults, spinal anesthesia is often performed at the interspace nearest an imaginary line stretching across the top of the iliac crests, the intercristal or Tuffier’s line, corresponding to the L3–L4 interspace. However, neonates and infants have a proportionally smaller pelvis than adults, and the sacrum is located more cephalad relative to the iliac crests. Therefore, Tuffier’s line crosses the midline of the vertebral column at the L4–L5 or L5–S1 interspace, well below the termination of the spinal cord, making this landmark applicable in all pediatric patients. The dural sac in neonates and infants also terminates in a more caudad location compared with that in adults, usually at about the level of S3 compared with the adult level of S1. The more caudad termination of the dural sac makes an inadvertent dural puncture more likely during the performance of a single-injection caudal block if the needle is advanced too far into the epidural space.
CSF volume is higher on a milliliter-per-kilogram basis in infants and neonates (4 mL/kg) compared with adults (2 mL/kg). In addition, CSF in infants is distributed relatively more in the spinal canal than in the head, as opposed to the distribution in adults. This may, in part, account for the higher local anesthetic dose requirements and shorter duration of action of spinal anesthesia in infants. The high cardiac output characteristic of the pediatric population shortens the duration of spinal blocks in children still further.
LOCAL ANESTHETICS
A variety of local anesthetics and doses have been described in the literature, including bupivacaine86 and ropivacaine. Bupivacaine 0.5%, 0.5–1 mg/kg, is generally used for spinal anesthesia in children weighing less than 10 kg. A dose toward the higher end of the range is preferred for smaller children; the risk of total spinal anesthesia is low as long as the procedure is carried out diligently (Table 7). An “epinephrine wash” of the syringe, rather than a standard dose of epinephrine, is preferred. A hyperbaric bupivacaine solution with glucose 8% provides a block of similar quality and duration than isobaric bupivacaine with glucose 0.9%.
Adjuvants to local anesthetics in spinal blocks have also been described. Clonidine in a dose of 1 mcg/kg added to bupivacaine (1 mg/kg) used in spinal anesthesia for newborn infants has been shown to prolong block duration to almost twice the duration of spinal anesthesia without clonidine. However, the use of 2 mcg/kg of clonidine may cause a transient decrease in blood pressure and greater postoperative sedation. It may be advisable to use a dose of caffeine of 10 mg/kg intravenously to prevent potential postoperative apnea, especially if clonidine is used in the spinal anesthetic solution.
In cases of bilateral hernia repair in former premature infants, the spinal block may be supplemented with a caudal block. The patient is turned on the side of the largest hernia while the block is performed; a spinal injection of 0.8 mg/kg bupivacaine is followed immediately by a caudal injection of 0.1% bupivacaine. This technique prolongs the duration of anesthesia and analgesia. Alternatively, a hypobaric solution of local anesthetic can be injected with the operative side up.
TABLE 7. Spinal anesthesia dosage in children.
| Local anesthetic solution: ropivacaine or bupivacaine 0.5% 0.5–1 mg/kg. | ||
| An easy way to calculate the dose for a single hernia repair in infants is as follows: | ||
| Age (mos) | Weight (kg) | Dose bupivacaine 0.5% |
| 1 | 3 | 1 mg/kg |
| 2 | 4 | 0.8 mg/kg |
| 3 | 5 | 0.6 mg/kg |
| > 4 | 6 | 0.4 mg/kg |
| Possible additives: • Epinephrine wash • Clonidine 1 mcg/kg • Morphine 10 mcg/kg only for cardiac surgery to facili-tate earlier extubation) |
||
ADVERSE EFFECTS
Adverse effects from spinal anesthesia commonly seen in adults are less common in children. These include hypotension, bradycardia, PDPH, and transient radicular symptoms.
Hypotension and bradycardia are uncommon in children despite the high levels of block required. Fluid loading to increase preload is rarely needed in children but, if needed, can be done at a rate of 10 mL/kg. Although some authors obtain venous access in the lower limbs of the patient after the spinal block has been performed (pain-free IV catheter placement), we recommend obtaining venous access before performing the spinal block. Puncuh et al. reported their experience with 1132 consecutive spinal anesthetics in which hypotension was rarely reported: only a mild decrease in blood pressure was reported in 9 of 942 patients younger than 10 years old and in 8 of 190 patients older than 10 years old.
The incidence of PDPH is lower in children than in adults. However, an incidence of 8% has been reported in oncological patients after frequent lumbar punctures for spinal tap. The use of different types of spinal needle was studied in this sub-group of patients, but no difference was found in the incidence of headache (15% Quincke; 9% pencil-point Whitacre; p = 0.43). Moreover, the incidence of headache was not different by age group, with 8 of 11 PDPHs occurring in children under 10 years of age and the youngest reported in a 23-month-old. PDPHs have been treated with bed rest and caffeine in adults but are followed by blood patch if the headache doesn’t resolve. In children, an optimal dose of caffeine is not known, and an epidural blood patch is performed with 0.3 mL/kg of blood when the headache persists.Transient radicular symptoms have been reported in children but without long-term adverse effects.
RELATIVE CONTRAINDICATIONS
The major contraindication for a spinal technique in a nonsedated child is a surgery duration of more than 60 minutes. Spinal anesthesia should be avoided in neonates and children who may have increased intracranial pressure. In children with neuromuscular diseases, ventricular shunts (atrial or peritoneal), and poorly controlled seizures, the use of spinal anesthesia is controversial. Other contraindications to spinal anesthesia are similar to those in the adult population and include severe anatomical deformities, systemic infection or at the site of puncture, underlying coagulopathy, and hemodynamic instability (Table 8).
When considering spinal anesthesia, special consideration should be given to children with a known difficult airway. Although spinal anesthesia may be a reasonable choice in these patients, the first consideration should be the ability of the practitioner to manage the airway. The need for IV sedation in preschool- and school-aged children poses its own set of risks in pediatric patients with a difficult airway. The surgical site, the anticipated length of the procedure, and the surgical position (ie, supine, lateral, or prone) are also important factors to be considered.
TABLE 8. Relative contraindications to spinal anesthesia in children.
| Anatomical abnormalities of the spine |
| Degenerative neuromuscular disease |
| Patient and family dissent |
| Coagulopathy |
| Bacterial infection |
| Increased intracranial pressure |
| Ventriculoperitoneal shunts |
NYSORA Tips
Special considerations for infants and children undergoing spinal anesthesia include the following:
- The expertise of the anesthesia provider
- The motivation of the surgeon
- The estimated length of surgery is less than 90 minutes
SPINAL ANESTHESIA FOR PEDIATRIC PATIENTS: TECHNIQUE
Preparation
Eutectic mixture of local anesthetic (EMLA) cream or LMX (4% lidocaine cream) may be applied to the site of insertion, although the risk of methemoglobinemia must be taken into account in very small premature infants. The operating room should be warmed before bringing the patient into to the room. Warm blankets and radiant heating lamps help to diminish heat loss in infants. With older children, the room should be quiet and, if possible, surgical instruments covered to minimize patient anxiety. Pediatric operating rooms may be equipped with stereo or video equipment, which may be used to distract older children if the block is performed without sedation. Standard monitoring devices (pulse oximeter, electrocardiogram, and blood pressure cuff) should be applied before performing the block.
A plan should be made regarding the concomitant use of IV sedation or inhalational general anesthesia. The approach should be dictated by the medical condition and age of the patient, the comfort level of the anesthesia provider, and the nature and anticipated length of the surgical procedure. General anesthesia may predispose very preterm infants to apnea and bradycardia. Spinal anesthesia in infants lasts no more than 90 minutes due to their physiological characteristics. Therefore, in former preterm infants undergoing lower abdominal procedures of less than 90 minutes’ duration, spinal anesthesia without adjuvant sedation may be performed. However, a short period of inhalational general anesthesia or supplemental IV sedation may sometimes be necessary while the block is being performed, especially if EMLA cream has not been used. Older children may require supplemental sedation or light general anesthesia prior to performing the block. In some cases, spinal anesthesia may be combined with caudal or epidural anesthesia to prolong analgesia.
Patient Position
Spinal anesthesia is customarily administered in the lateral or sitting position in children. If the lateral position is preferred, the patient is positioned at the very border of the surgical table and held firmly by an assistant. Otherwise, the patient can be placed in the middle of the surgical table but on top of several blankets; these will give the necessary height for the anesthesiologist’s hands to be placed comfortably while performing the block (Figure 28). If the sitting position is preferred, special attention must be paid in infants to ensure that the neck is not flexed, as this could result in airway obstruction (Figure 29). It is essential to vigilantly monitor oxygen saturation in infants while performing the spinal to ensure adequacy and patency of the airway. Moreover, neck flexion is not necessary because it does not facilitate the performance of the block in small children. In older children, an assistant should be present to maintain proper positioning and to reassure and distract the child while the block is being performed. The use of a pacifier, while the block is being performed in a nonsedated infant, is usually helpful.

FIGURE 28. Spinal anesthesia in the lateral position. The child is placed on top of several blankets to gain height for the anesthesiologist’s hands while performing the block.

FIGURE 29. Spinal anesthesia in the sitting position. Head flexion must be avoided to prevent airway obstruction.
Technique
In infants, the L4–L5 or L5–S1 interspace should be identified; the L3–L4 interspace may be used in older children. The area should be prepared and draped in a sterile fashion. If topical anesthetic cream was not applied preoperatively, local anesthesia should be administered before the block in awake or lightly sedated patients. The desired dose of spinal local anesthetic should be calculated and prepared in a syringe before dural puncture to ensure that the correct dose is administered. Because the volume of local anesthetic needed may be small in neonates, it is important to measure the volume corresponding to the hub of the needle and to count this volume, too, in the total dose of local anesthetic. An insulin syringe is helpful to measure the exact dose accurately. A short, 22- or 25-gauge spinal needle is often used (Figure 30). A midline approach is usually recommended over a paramedian approach. The ligamentum flavum is very soft in children, and a distinctive “pop” may not be perceived when the dura is penetrated (Figure 31). Once clear CSF is exiting the needle, the drug(s) may be administered and, importantly, must be injected slowly (Figure 32).

FIGURE 30. Equipment used for spinal anesthesia in neonates: spinal needle and syringe with local anesthetic.

FIGURE 32. Spinal anesthesia: Cerebrospinal fluid exits the needle, and local anesthetic is injected.
The barbotage method is not recommended, as it may result in unacceptably high levels of motor block and has a potential for total spinal block. The patient’s lower limbs should not be elevated for the placement of the electrocautery return electrode on the infant’s back, as total spinal anesthesia can result from the spread of local anesthetic to a higher spinal level. To prolong the duration of surgical anesthesia in the case of bilateral hernia repair, spinal anesthesia can be supplemented with a caudal block.
Assessing the Block
Assessing the level of block may prove difficult in infants and young children, particularly in patients who have received sedation or in those in whom the block is being performed under general anesthesia. In infants, pinprick or response to cold stimuli (eg, an alcohol swab) may be used, as well as observation of ventilation rate and pattern. In children over 2 years of age, the Bromage scale is used. Following the block, care should be taken to avoid placing the patient in the Trendelenburg position or lifting the lower limbs; for example, to place an electrocautery pad on the infant’s back. In the event of a rapidly rising level of block, the patient may be placed in the reverse Trendelenburg position.
NYSORA Tips
Evaluation of Spinal Anesthesia: The Bromage Scale
- No block: Free movement of knees and feet is possible
- Partial block: Able only to flex knees but free movement of feet still possible
- Almost complete block: Unable to flex knees but flex-ion of feet still possible
- Complete: Unable to move legs or feet
CLINICAL USES
Apnea and Former Preterm Infants
The most common indication for spinal anesthesia in pediatric patients is in former preterm infants undergoing unilateral inguinal hernia repair (Table 9). Apnea can occur in former preterm patients following a general anesthetic. Regional anesthesia may decrease, if not eliminate, the risk of postoperative apnea and certainly decreases the risk of desaturation and bradycardia.
TABLE 9. Indications for spinal anesthesia in children.
| Inguinal hernia repair |
| Myelomeningocele repair |
| Lower limb and lower abdominal surgery |
| Early extubation desired after cardiac surgery |
However, there is considerable disagreement regarding the incidence of apnea and the conceptual age at which a former preterm infant may safely undergo general anesthesia on an outpatient basis. Lack of uniformity in study design, small patient population sizes, and variations in methodology probably account for the differences noted. Cote at al. performed a meta-analysis of eight studies, comprising 255 patients, investigating postoperative apnea in former preterm infants after general anesthesia. Overall, the risk was independently related to both gestational age and conceptual age. Additional risk factors for postoperative apnea were a hematocrit less than 30% and continued apneic episodes at home. The study stratified infants into two groups: a 5% risk group and a 1% risk group. For patients with a gestational age of 35 weeks, the risk of post-operative apnea did not fall below 5% (with a 95% statistical confidence interval) until patients reached a postconceptual age of 48 weeks and did not decrease below 1% until infants reached a postconceptual age of 54 weeks. In more preterm patients, such as those with a gestational age of 32 weeks, the risk of apnea did not fall below 1% (with a 95% statistical confidence interval) until infants reached a postconceptual age of 56 weeks.
The concomitant use of ketamine as a sedative in former preterm infants was also reported to increase the incidence of postoperative apnea above that reported in control patients. However, these are all somewhat older studies. In the mean-time, there have been substantial advances in the ventilatory management of premature neonates and infants, making the risk of apnea controversial at the present day. Moreover, improvements in anesthesia, such as the extended use of sevoflurane instead of halothane and laryngeal masks instead of tracheal intubation, have further decreased the incidence of the deleterious effects of general anesthesia in infants. Craven et al. reviewed several randomized controlled studies and found only a borderline statistical advantage of spinal anesthetic over general anesthesia. In our opinion, administering sevoflurane while spontaneous ventilation for a short period of time may sometimes be useful to aid in performing the spinal block, especially if no EMLA cream is used.
Spinal anesthesia has also been used for a variety of other procedures, including myelomeningocele repair and other abdominal, urological, and orthopedic procedures in children. The early report by Abajian et al. included not only infants undergoing inguinal herniorrhaphy but also other noninfant patients whom the authors felt faced an increased risk for general anesthesia. This study included patients with a variety of medical conditions, including laryngomalacia, macroglossia, micrognathia, congenital heart disease, Down syndrome, adrenogenital syndrome, failure to thrive, and arthrogryposis. Blaise et al. reported 30 patients aged 7 weeks to 13 years old who underwent spinal anesthesia for a variety of surgical procedures. Kokki et al. reported satisfactory anesthesia in 92 of 93 children aged 1 to 17 years old undergoing spinal anesthesia with ropivacaine for lower abdominal or lower limb procedures.Regional techniques have been used in cardiac surgery to facilitate early extubation. This large series investigating spinal anesthesia for cardiac surgery comes from a prospective randomized analysis from Stanford University. The group who received spinal anesthesia for postoperative pain relief had less opioid requirement in the postoperative period after elective cardiac surgery with early extubation in the operating room.
In summary, spinal anesthesia in pediatrics is most commonly used in preterm infants undergoing anesthesia for inguinal hernia repair. Spinal anesthesia can also be used effectively in children for postoperative pain relief in cardiac surgery, especially if opioids are used.
REFERENCES
- Peutrell JM, Lonnqvist PA: Neuraxial blocks for anaesthesia and analgesia in children. Curr Opin Anaesthesiol 2003;16:461–470. 2
- Suresh S, Long J, Birmingham PK, et al: Are caudal blocks for pain control safe in children? An analysis of 18,650 caudal blocks from the Pediatric Regional Anesthesia Network (PRAN) database. Anesth Analg 2015;120:151–156.
- Gunter JB, Eng C: Thoracic epidural anesthesia via the caudal approach in children. Anesthesiology 1992;76:935–938.
- Larsson BA, Lonnqvist PA, Olsson GL: Plasma concentrations of bupivacaine in neonates after continuous epidural infusion. Anesth Analg 1997;84:501–505.
- Luz G, Innerhofer P, Bachmann B, et al: Bupivacaine plasma concentrations during continuous epidural anesthesia in infants and children. Anesth Analg 1996;82:231–234.
- Berde C: Local anesthetics in infants and children: an update. Paediatr Anaesth 2004;14:387–393.
- Gunter JB, Dunn CM, Bennie JB, et al: Optimum concentration of bupivacaine for combined caudal–general anesthesia in children. Anesthesiology 1991;75:57–61.
- Tsui BC, Berde CB: Caudal analgesia and anesthesia techniques in children. Curr Opin Anaesthesiol 2005;18:283–288.
- Lönnqvist PA: Review article. Toxicity of local anesthetic drugs: a pediatric perspective. Paediatr Anaesth 2012;22:39–43.
- Da Conceicao MJ, Coelho L, Khalil M: Ropivacaine 0.25% compared with bupivacaine 0.25% by the caudal route. Paediatr Anaesth 1999; 9:229–233.
- Eledjam JJ, Gros T, Viel E, et al: Ropivacaine overdose and systemic toxicity. Anaesth Intensive Care 2000;28:705–707.
- Ivani G, Lampugnani E, Torre M, et al: Comparison of ropivacaine with bupivacaine for paediatric caudal block. Br J Anaesth 1998;81: 247–248.
- Karmakar MK, Aun CS, Wong EL, et al: Ropivacaine undergoes slower systemic absorption from the caudal epidural space in children than bupivacaine (table). Anesth Analg 2002;94:259–265.
- Kokko TI, Karinen J, Raiha E, et al: Pharmacokinetics of 0.75% ropivacaine and 0.5% bupivacaine after ilioinguinal-iliohypogastric nerve block in children. Br J Anaesth 2002;89:438–441.
- Gunter JB: Benefit and risks of local anesthetics in infants and children. Paediatr Drugs 2002;4:649–672.
- Bosenberg A, Thomas J, Lopez T, et al: The efficacy of caudal ropivacaine 1, 2 and 3 mg × l(-1) for postoperative analgesia in children. Paediatr Anaesth 2002;12:53–58.
- Ivani G. Ropivacaine: is it time for children? Paediatr Anaesth 2002; 12:383–387.
- Taylor R, Eyres R, Chalkiadis GA, et al: Efficacy and safety of caudal injection of levobupivacaine, 0.25%, in children under 2 years of age undergoing inguinal hernia repair, circumcision or orchidopexy. Paediatr Anaesth 2003;13:114–121.
- Lonnqvist PA: Adjuncts to caudal block in children—Quo vadis? Br J Anaesth 2005;95:431–433.
- Lonnqvist PA, Ivani G, Moriarty T: Use of caudal-epidural opioids in children: still state of the art or the beginning of the end? Paediatr Anaesth 2002;12:747–749.
- Attia J, Ecoffey C, Sandouk P, et al: Epidural morphine in children: pharmacokinetics and CO2 sensitivity. Anesthesiology 1986;65:590–594.
- Ansermino M, Basu R, Vandebeek C, et al: Nonopioid additives to local anaesthetics for caudal block in children: a systematic review. Paediatr Anaesth 2003;13:561–573.
- De Negri P, Ivani G, Visconti C, et al: The dose-response relationship for clonidine added to a postoperative continuous epidural infusion of ropivacaine in children. Anesth Analg 2001;93:71–76.
- Penon C, Ecoffey C, Cohen SE: Ventilatory response to carbon dioxide after epidural clonidine injection. Anesth Analg 1991;72:761–991.
- Fellmann C, Gerber AC, Weiss M: Apnoea in a former preterm infant after caudal bupivacaine with clonidine for inguinal herniorrhaphy. Paediatr Anaesth 2002;12:637–640.
- Passariello M, Almenrader N, Canneti A, et al: Caudal analgesia in children: S(+)-ketamine vs S(+)-ketamine plus clonidine. Paediatr Anaesth 2004;14:851–855.
- Hager H, Marhofer P, Sitzwohl C, et al: Caudal clonidine prolongs analgesia from caudal S (+)-ketamine in children. Anesth Analg 2002; 94:1169–1172.
- Hayashi H, Dikkes P, Soriano SG: Repeated administration of ketamine may lead to neuronal degeneration in the developing rat brain. Paediatr Anaesth 2002;12:770–774.
- Proescholdt M, Heimann A, Kempski O: Neuroprotection of S(+) ketamine isomer in global forebrain ischemia. Brain Res 2001; 904: 245–251.
- Suresh S, Wheeler M: Practical pediatric regional anesthesia. Anesthesiol Clin North Am 2002;20:83–113.
- Giaufre E, Dalens B, Gombert A: Epidemiology and morbidity of regional anesthesia in children: a one-year prospective survey of the French-Language Society of Pediatric Anesthesiologists. Anesth Analg 1996;83:904–912
- Flandin-Blety C, Barrier G: Accidents following extradural analgesia in children. The results of a retrospective study. Paediatr Anaesth 1995;5:41–46.
- Fischer HB: Performing epidural insertion under general anaesthesia. Anaesthesia 2000;55:288–289.
- Kasai T, Yaegashi K, Hirose M, et al: Spinal cord injury in a child caused by an accidental dural puncture with a single-shot thoracic epidural needle. Anesth Analg 2003;96:65–67.
- Horlocker T, Wedel DJ, Rowlingson JC, et al: Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy. American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition). Reg Anesth Pain Med 2010;35:64–101.
- Kost-Byerly S, Tobin JR, Greenberg RS, et al: Bacterial colonization and infection rate of continuous epidural catheters in children. Anesth Analg 1998;86:712–716.
- Wittum S, Hofer CK, Rolli U, et al: Sacral osteomyelitis after single-shot epidural anesthesia via the caudal approach in a child. Anesthesiology 2003;99:503–505.
- Bubeck J, Boos K, Krause H, Thies KC: Subcutaneous tunneling of caudal catheters reduces the rate of bacterial colonization to that of lumbar epidural catheters. Anesth Analg 2004;99:689–693.
- Oliver A: Dural punctures in children: what should we do? Paediatr Anaesth 2002;12:473–477.
- Liley A, Manoharan M, Upadhyay V: The management of a post-dural puncture headache in a child. Paediatr Anaesth 2003;13:534–537.
- Janssens E, Aerssens P, Alliet P, et al: Post-dural puncture headaches in children. A literature review. Eur J Pediatr 2003;162:117–121.
- Tsuji MH, Horigome H, Yamashita M: Left ventricular functions are not impaired after lumbar epidural anaesthesia in young children. Paediatr Anaesth 1996;6:405–409.
- Tsui BC, Malherbe S, Koller J, et al: Reversal of an unintentional spinal anesthetic by cerebrospinal lavage. Anesth Analg 2004;98:434–436.
- Tobias JD: Caudal epidural block: a review of test dosing and recognition of systemic injection in children. Anesth Analg 2001;93:1156–1161.
- Neal JM, Mulroy MF, Weinberg GF: American Society of Regional Anesthesia and Pain Medicine. Checklist for Managing Local Anesthetic Systemic Toxicity: 2012 Version. Reg Anesth Pain Med 2012;37:16Y18.
- Flandin-Blety C, Barrier G: Accidents following extradural analgesia in children. The results of a retrospective study. Paediatr Anaesth 1995; 5:41–46.
- Valairucha S, Seefelder C, Houck CS: Thoracic epidural catheters placed by the caudal route in infants: the importance of radiographic confirmation. Paediatr Anaesth 2002;12:424–428.
- Tsui BC, Gupta S, Finucane B: Confirmation of epidural catheter placement using nerve stimulation. Can J Anaesth 1998;45:640–644.
- Tsui BC, Seal R, Koller J, et al: Thoracic epidural analgesia via the caudal approach in pediatric patients undergoing fundoplication using nerve stimulation guidance. Anesth Analg 2001;93:1152–1155.
- Tsui BC, Gupta S, Finucane B: Detection of subarachnoid and intravascular epidural catheter placement. Can J Anaesth 1999;46: 675–678.
- Tsui BC, Gupta S, Emery D, Finucane B: Detection of subdural placement of epidural catheter using nerve stimulation. Can J Anaesth 2000;47:471–473.
- Tsui BC: Thoracic epidural catheter placement in infants via the caudal approach under electrocardiographic guidance: simplification of the original technique. Anesth Analg 2004;98:273.
- Chen CP, Tang SF, Hsu TC, et al: Ultrasound guidance in caudal epidural needle placement. Anesthesiology 2004;101:181–184.
- Chawathe MS, Jones RM, Gildersleve CD, et al: Detection of epidural catheters with ultrasound in children. Paediatr Anaesth 2003;13: 681–684.
- Baris S, Guldogus F, Baris YS, et al: Is tissue coring a real problem after caudal injection in children? Paediatr Anaesth 2004;14:755–758.
- Lam DK, Corry GN, Tsui BC: Evidence for the use of ultrasound imaging in pediatric regional anesthesia: a systematic review. Reg Anesth Pain Med 2016;41:229–241.
- Rubin K, Sullivan D, Sadhasivam S: Are peripheral and neuraxial blocks with ultrasound guidance more effective and safe in children? Paediatr Anaesth 2009;19:92–96.
- Perlas A: Evidence for the use of ultrasound in neuraxial blocks. Reg Anesth Pain Med 2010;35(2 Suppl):S43–46.
- Triffterer L, Machata AM, Latzke D, et al: Ultrasound assessment of cranial spread during caudal block in children: effect of the speed of injection of local anaesthetics. Br J Anaesth 2012;108:670–674.
- Brenner L, Marhofer P, Kettner SC, et al: Ultrasound assessment of cranial spread during caudal block in children: the effect of different volumes of local anaesthetics. Br J Anaesth 2011;107:229–235.
- Lundblad M, Lönnqvist PA, Eksborg S, et al: Segmental distribution of high-volume caudal anesthesia in neonates, infants, and toddlers as assessed by ultrasonography. Paediatr Anaesth 2010;21:121–127.
- Lundblad M, Eksborg S, Lönnqvist PA: Secondary spread of caudal block as assessed by ultrasonography. Br J Anaesth 2012;108:675–681.
- Tamai H, Sawamura S, Kanamori Y, et al: Thoracic epidural catheter insertion using the caudal approach assisted with an electrical nerve stimulator in young children. Reg Anesth Pain Med 2004;29:92–95.
- Tsui BC, Wagner A, Cave D, et al: Thoracic and lumbar epidural analgesia via the caudal approach using electrical stimulation guidance in pediatric patients: a review of 289 patients. Anesthesiology 2004;100:683–689.
- Tsui BC, Entwistle L: Thoracic epidural analgesia via the lumbar approach using nerve stimulation in a pediatric patient with Down syndrome. Acta Anaesthesiol Scand 2005;49:712–714.
- Fischer HB: Performing epidural insertion under general anaesthesia. Anaesthesia 2000;55:288–289.
- Kasai T, Yaegashi K, Hirose M, et al: Spinal cord injury in a child caused by an accidental dural puncture with a single-shot thoracic epidural needle. Anesth Analg 2003;96:65–67.
- Bromage PR, Benumof JL: Paraplegia following intracord injection during attempted epidural anesthesia under general anesthesia. Reg Anesth Pain Med 1998;23:104–107.
- Chawathe MS, Jones RM, Gildersleve CD, et al: Detection of epidural catheters with ultrasound in children. Paediatr Anaesth 2003;13: 681–684.
- Corning JL: Spinal anesthesia and local medication of the cord. NY J Med 1885;42:483–485.
- Gray H: A study of spinal anaesthesia in children and infants: from a series of 200 cases. Lancet 1909;2:913–917.
- Bainbridge W: Analgesia in children by spinal injection with a report of a new method of sterilization of the injection fluid. Med Rec 1900;58:937–940.
- Melman E, Penuelas JA, Marrufo J: Regional anesthesia in children. Anesth Analg 1975;54:387–390.
- Gregory GA, Steward DJ: Life-threatening perioperative apnea in the ex-”premie.” Anesthesiology 1983;59:495–498.
- Steward DJ: Postoperative apnea syndrome in premature infants. West J Med 1992;157:567.
- Steward DJ: Preterm infants are more prone to complications following minor surgery than are term infants. Anesthesiology 1982;56:304–306.
- Cote CJ, Zaslavsky A, Downes JJ, et al: Postoperative apnea in former preterm infants after inguinal herniorrhaphy. A combined analysis [see comments]. Anesthesiology 1995;82:809–822.
- Liu LM, Cote CJ, Goudsouzian NG, et al: Life-threatening apnea in infants recovering from anesthesia. Anesthesiology 1983;59:506–510.
- Abajian JC, Mellish RW, Browne AF, et al: Spinal anesthesia for surgery in the high-risk infant. Anesth Analg 1984;63:359–362.
- Frumiento C, Abajian JC, Vane DW: Spinal anesthesia for preterm infants undergoing inguinal hernia repair. Arch Surg 2000;135:445–451.
- Blaise GA, Roy WL: Spinal anaesthesia for minor paediatric surgery. Can Anaesth Soc J 1986;33:227–230.
- Kokki H, Tuovinen K, Hendolin H: Spinal anaesthesia for paediatric day-case surgery: a double-blind, randomized, parallel group, prospective comparison of isobaric and hyperbaric bupivacaine. Br J Anaesth 1998;81:502–506.
- Busoni P, Messeri A: Spinal anesthesia in children: surface anatomy. Anesth Analg 1989;68:418–419.
- Busoni P, Messeri A: Spinal anesthesia in infants: could a L5-S1 approach be safer? Anesthesiology 1991;75:168–169.
- Gray H: Anatomy of the Human Body: Gray’s Anatomy, 30th ed. Philadelphia: Lippincott Williams & Wilkins, 1985.
- Puncuh F, Lampugnani E, Kokki H: Use of spinal anaesthesia in paediatric patients: a single centre experience with 1132 cases. Paediatr Anaesth 2004;14:564–567.
- Kokki H, Ylonen P, Laisalmi M, et al: Isobaric ropivacaine 5 mg/mL for spinal anesthesia in children. Anesth Analg 2005;100:66–70.
- Kokki H, Hendolin H: Hyperbaric bupivacaine for spinal anaesthesia in 7–18 yr old children: comparison of bupivacaine 5 mg mL-1 in 0.9% and 8% glucose solutions. Br J Anaesth 2000;84:59–62.
- Rochette A, Raux O, Troncin R, et al: Clonidine prolongs spinal anesthesia in newborns: a prospective dose-ranging study. Anesth Analg 2004;98:56–59.
- Welborn LG, de Soto H, Hannallah RS, et al: The use of caffeine in the control of post-anesthetic apnea in former premature infants. Anesthesiology 1988;68:796–798.
- Oberlander TF, Berde CB, Lam KH, et al: Infants tolerate spinal anesthesia with minimal overall autonomic changes: analysis of heart rate variability in former premature infants undergoing hernia repair. Anesth Analg 1995;80:20–27.
- Ramamoorthy C, Geiduschek JM, Bratton SL, et al: Postdural puncture headache in pediatric oncology patients. Clin Pediatr 1998;37:247–251.
- Kokki H, Salonvaara M, Herrgard E, Onen P: Postdural puncture headache is not an age-related symptom in children: s prospective, open-randomized, parallel group study comparing a 22-gauge Quincke with a 22-gauge Whitacre needle. Paediatr Anaesth 1999;9:429–434.
- Salmela L, Aromaa U: Transient radicular irritation after spinal anesthesia induced with hyperbaric solutions of cerebrospinal fluiddiluted lidocaine 50 mg/mL or mepivacaine 40 mg/mL or bupivacaine 5 mg/mL. Acta Anaesthesiol Scand 1998;42:765–769.
- Welborn LG, Rice LJ, Hannallah RS, et al: Postoperative apnea in former preterm infants: prospective comparison of spinal and general anesthesia. Anesthesiology 1990;72:838–842.
- Gleason CA, Martin RJ, Anderson JV, et al: Optimal position for a spinal tap in preterm infants. Pediatrics 1983;71:31–35.
- Krane EJ, Haberkern CM, Jacobson LE: Postoperative apnea, bradycardia, and oxygen desaturation in formerly premature infants: prospective comparison of spinal and general anesthesia. Anesth Analg 1995;80:7–13.
- Craven PD, Badawi M, Henderson-Smart DJ, O’Brien M: Regional (spinal, epidural, caudal) versus general anaesthesia in preterm infants undergoing inguinal herniorrhaphy in early infancy. Cochrane Database Syst Rev 2003;(3):CD003669.
- Viscomi CM, Abajian JC, Wald SL, et al: Spinal anesthesia for repair of meningomyelocele in neonates. Anesth Analg 1995;81:492–495.
- Kokki H, Hendolin H. Comparison of spinal anaesthesia with epidural anaesthesia in paediatric surgery. Acta Anaesthesiol Scand 1995;39: 896–900.
- Hammer GB, Ramamoorthy C, Cao H, et al: Postoperative analgesia after spinal block in infants and children undergoing cardiac surgery. Anesth Analg 2005;100:1283–1288.