Johan Raeder and Ulrich J. Spreng
INTRODUCTION
Infiltration or instillation of local anesthetics around and into the joint as an analgesic adjunct for postoperative joint surgery pain has been used for decades. However, there has been a renewed interest in local infiltration analgesia (LIA), partly due to the work in 2008 of Kerr and Kohan, who demonstrated superior analgesia after total knee or hip arthroplasty with extended, diluted infiltration of local anesthesia with epinephrine and ketorolac added and repeated injections through intraarticular catheters. The interest in using LIA in knee and hip surgery may be also due to the lack of the simpler regional anesthesia alternatives that exist for other joints. For instance, analgesia after shoulder and upper extremity surgery can be accomplished with a simple, single injection block of the brachial plexus, whereas analgesia for hip and knee joints requires multiple and more technically challenging nerve blocks. Also, while motor weakness is common with nerve blocks, infiltration analgesia typically spares the motor function.
THE CONCEPT OF LOCAL INFILTRATION
ANALGESIA
There are three basic components of the LIA concept: high volume of diluted, long-acting local anesthetic; nonlocal anesthetic adjuvants; and catheter bolus injections (top-ups) for 1–3 days.
High Volume of Diluted Long-Acting
Anesthetic Drug
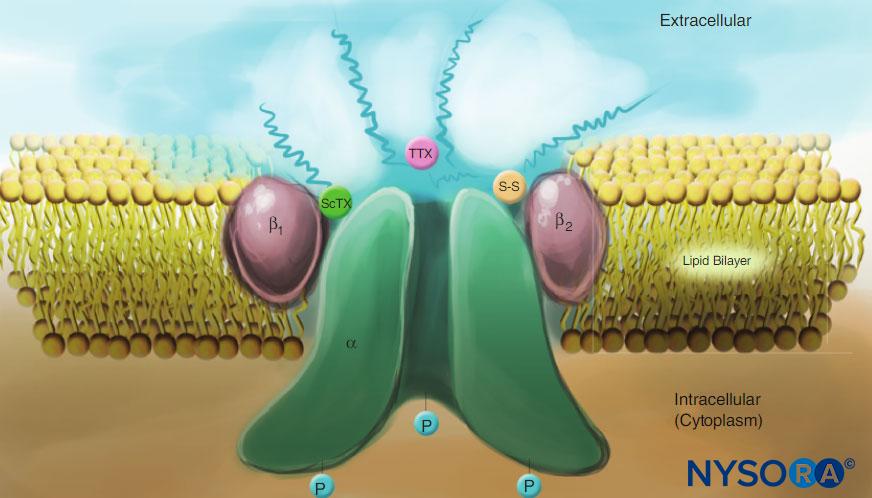
A problem with local anesthetic infiltration for major surgery is that many different structures and layers must be infiltrated. In doing so, a certain minimum volume of local anesthetic is required for an effective local infiltration to cover all relevant structures. With conventional concentrations of local anesthetic solutions, such high volumes carry an unacceptable risk of systemic toxicity (see Local Anesthetic Systemic Toxicity). However, anesthesia of the small nerve endings in and around joints does not require high-concentration local anesthetic. Thus, the concentration of local anesthetic may be lowered and the volume increased, keeping the total dose within safe limits. Further, as the major joints are devoid of major blood vessels, the risk of inadvertent injection of a large bolus directly into circulation is small.
Nonlocal Anesthetic Adjuvants
As careful injections of local anesthetic are made close to the site of surgical injury, there is a potential for targeting the source of pain caused by local inflammation and pain to supply effective treatment close to the origin of pain. This is an alternative to the systemic approach to analgesia by which a potentially higher total dose of drug is needed and carries a higher potential of general side effects. Nonlocal anesthetic adjuvants such as anti-inflammatory agents, nonsteroidal anti-inflammatory drugs (NSAIDs—traditional or cyclooxygenase [COX] 2 inhibitors) and steroids, as well as opioids and ketamine have all been used. The role of epinephrine or clonidine in the LIA mixture, however, has not been well studied. While both drugs have an analgesic effect on the spinal α2 receptors when given epidurally or spinally, there is no documentation on any specific analgesic effect or target mechanism of these drugs when used peripherally. Epinephrine is often empirically included “just in case” due to the potential to prolong effect of other locally active drugs as their clearance from the local site is delayed due to the epinephrine-induced vasoconstriction.
Catheter Top-ups for 1 to 3 Days
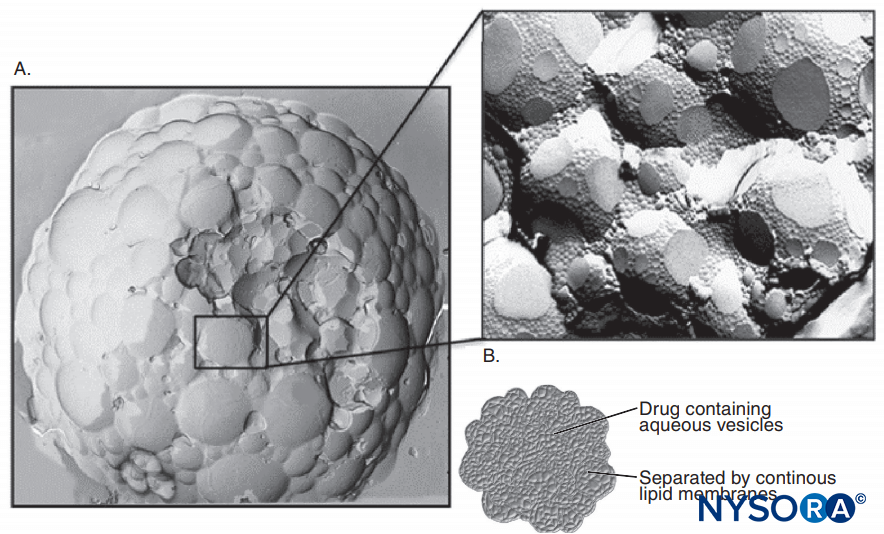
Long-acting local anesthetics used for infiltration, perioperative injections, and infiltration all have a limited duration and wear off within a few hours after injection. Because repeated injection of the local anesthetic is painful or inconvenient, one approach is to leave one or more catheters in the wound or joint to provide the vehicle for boluses or continuous infusion of local anesthetics. The use of catheters in a setting of major joint replacement, however, is controversial because of the potential for infection. The routine use of catheter is also challenged in the United States by the recent development and FDA approval of long-acting depot bupivacaine, (liposomal bupivacaine) although the role and potential of this drug in the LIA concept requires more scrutiny.
EVIDENCE-BASED INFORMATION ON EFFICACY AND SAFETY OF LOCAL INFILTRATION ANALGESIA
As often is the case with new methods and techniques, the initial enthusiasm for LIA expressed in clinical practices, professional gatherings, and case reports,1 awaits evidence-based scrutiny before recommendations for everyday clinical use can be made. The following are important questions that need scrutiny:
1.Is the method sufficiently efficacious?
2.What components of the new method are efficient?
3.How does LIA compare to other common methods in terms of safety, quality, and cost?
If a new method is tested as a component of a multimodal regimen and shows superiority versus controls, we may have the answer to the first question, but questions 2 and 3 remain unanswered. The logical next steps are to put to test each component individually (keeping all the rest unchanged and standardized) in controlled and standardized conditions to elucidate which components of the multimodal protocol are actually beneficial. The LIA should be compared with the best potential alternatives used under optimal conditions: intrathecal opioid, epidural analgesia, femoral nerve block, other nerve blocks, or just optimal multimodal analgesia, including local anesthesia wound infiltration. We do know that infiltration of local anesthetics confers analgesia after knee replacement surgery, assuming that local anesthetic is skillfully infiltrated in all relevant tissues. In a study of hernia repair with bupivacaine infiltration analgesia, Aasboe et al showed improved pain relief for as much as 1 week after the procedure. Still, such results are to some extent procedure specific and not reproduced with LIA by others. In the study of Andersen et al on knee arthroplasty, the preoperative ropivacaine infiltration was superior to placebo at 6 hours but not at 24 hours. The success of LIA may be dependent on how extensive the local infiltration technique is performed in terms of including all relevant structures, not only the superficial wound layers. With all new concepts, one must find a balance between rapidly incorporating the benefits into everyday practice while waiting for objective documentation from quality studies. The studies done so far on the efficacy of LIA do not have the power, standardization, or quality to provide a clear answer or even provide quality pooled data for meta-analyses.
One reason for the paucity of the evidence is that randomized, blinded studies incorporating LIA are somewhat difficult to design because all injections, catheters, and refilling, need to be done in the placebo group as well. Even then, such a placebo group would not be relevant because in clinical practice saline injections in wound structures and catheters would not occur, and yet, saline injections alone may have analgesic benefits. This is because infiltration of saline into the knee joint has analgesic effect, possibly by cooling and dilution of inflammatory local proteins, or placebo. As there are many confounders, ideal studies on the efficacy of LIA should address only one or a few specific items at a time, controlling or standardizing the others. Such specific items include one specific type of surgery, systemic controls for all active drugs in the LIA mixture, and sham or placebo infusions or top-ups when testing postoperative LIA. Analgesic effects of ketorolac and ropivacaine when given systemically are well known. Likewise, intra-articular administration will also result in systemic absorption and systemic effects. It should be remembered that LIA may never be well standardized as a defined dose of a single intravenous drug or a specific nerve block for a few reasons.
First, different types of surgery and joints vary in anatomical composition, acceptability for and spread of LIA, and degree of postoperative pain. Second, differences in infiltration techniques may influence the analgesic benefits. Clinical impression suggests that the morning injection the day after surgery seems to have an analgesic effect on patients in pain, although this was not demonstrated convincingly in controlled studies. This may be because control patients in studies usually receive a placebo injection and often have low-to-moderate pain and thus not much potential or statistical power for showing improvements for the whole group. Two further aspects of clinical interpretation of studies are important: If the control group receives an effective multimodal analgesic regimen resulting in low pain scores, it makes it difficult to demonstrate additional benefits of a new method. However, if a new method is equally effective but not better, it does not mean that the new method is of no value. In contrast, this simply provides a choice of two different methods with differences in side-effect profile, risks, and practical and economic aspects. The benefits of LIA may be in various aspects of nursing care, less need for patient compliance, lower total dose of NSAID, lower need for opioids, lower need for gabapentinoids and their potential side effects, and so on. Still, the number of patients in many studies is too low to address the questions of safety and less-frequent side effects. Studies must carefully examine serious, but rare, side effects, as well as how to use LIA as a tool to improve rehabilitation, shorten hospital stay, and achieve a better functional outcome.
What are the alternatives to LIA for knee or hip arthroplasty? In terms of “most effective” pain relief, it is hard to better epidural analgesia.However, epidural analgesia does not provide any analgesic benefits beyond the period of active use. In addition, during the analgesic treatment, the technique is resource demanding and impairs mobilization and physiotherapy. There are also risks of urinary retention, hypotension, and epidural hematoma. The femoral nerve block for knee arthroplasty provides more specific treatment but does not cover all nerves involved in knee innervation and results in quadriceps muscle weakness.
As with epidural block, this technique may be associated with very rare but serious nerve damage. In a recent study comparing LIA and femoral block for knee arthroplasty, Affas et al showed less pain with activity with LIA at 24 hours and an advantage in terms of ease of performance and lower costs. Other nerve blocks may provide more focused single-knee pain relief without motor block, such as an adductor canal block of the saphenous and obturator nerves. Intrathecal opioid, as used in the study of Essving et al may be beneficial as well. Morphine appears to be the best drug in terms of prolonged effect after a single shot. However, a dose higher than 0.1 mg may in some cases prolong the effect, but with a higher risk of side effects. The expert, evidence-based, procedure-specific recommendation for knee arthroplasty (see http://www.postoppain.org/image.aspx?imgid=654) is the combination of either spinal anesthesia without opioid or general anesthesia with femoral block as the first choice for anesthesia. Either should be supplemented with acetaminophen plus NSAID plus an opioid for breakthrough pain. The recommendation for avoiding intrathecal morphine was based on nausea in a study with a morphine dose of 0.25 mg and may not be relevant with the 0.1-mg dose used by Essving et al. Although used by some, there are no convincing data that steroids or gabapentinoid confer additional analgesic benefits.
POTENTIAL AND DOCUMENTED PROS AND CONS OF LOCAL INFILTRATION ANALGESIA AND ALTERNATIVES
Pros
A major benefit of LIA is the lack of motor impairment often seen with alternative techniques of nerve blocks, such as femoral or sciatic nerve blocks, or epidural analgesia. With LIA, there is also a minor risk of hematoma formation, which is a feared complication of deep blocks, such as lumbar block or epidural analgesia. Also, LIA is not contraindicated in cases of increased bleeding risk from other causes, such as therapeutic anticoagulation, platelet inhibition, or even use of traditional NSAIDs or low-dose acetylsalicylic acid. Another argument for LIA is its simplicity; the infiltration is can be done by the surgeon intraoperatively or anesthesia providers using ultrasound. Postoperative top-ups of one or more catheters may be done easily by a nurse on the ward.
Cons
Some of the specific cons of LIA have to do with the potential dangers of supplying a potent drug close to delicate joint structures. The local anesthetic may be neurotoxic to small nerves when supplied repeatedly, although diluted ropivacaine has proven to be safe for 2–3 days of continuous infusion. A more serious concern may be the chondrotoxic effect, especially with bupivacaine. Because in most hip and knee replacement surgeries the cartilage is removed as a part of the procedure, this consideration may not be of practical concern. Adding NSAIDs, COX-2 inhibitors, or glucocorticoids may slow or impair tissue healing or growth, although practical impact has not yet been shown in human clinical studies in patients having hip or knee replacement. A concern has been voiced regarding a potential for increased risk of infection with LIA. This concern arises mainly from the postoperative use of a catheter with the risk of contamination from multiple injections as well as bacteria migration along the indwelling catheter, rather than from the sterile infiltration done during surgery. It is also theorized that epinephrine may impede circulation, oxygenation, and macrophage function. To minimize the risk of infection, it is important to use strict aseptic procedures for all top-ups and refills of infusions.
LOCAL INFILTRATION ANALGESIA FOR HIP ARTHROPLASTY
Kehlet et al reviewed six available studies in 2011, whereas McCarthy and Iohom extended the review by including additional additional studies. Since then, the two studies of Rikalainen-Salimi and Murphy et al have also been published. The early studies of Kerr and Kohan et al and Otte et al reported favorable analgesia and rapid mobilization with LIA; however, there were no control groups. In the Parvataneni et al and Busch et al studies, LIA was compared to intravenous opioid analgesia. Both studies reported lower pain scores with LIA; the Parvataneni et al study reduced hospital stay by 1 day with LIA. Four studies have compared LIA versus placebo.
The first placebo-controlled trial of Bianconi et al from 2003 used only 40 mL of ropivacaine 5 mg/mL were used for infiltration, but infusion of 10 mg/h continued for 35 hours. The LIA group had lower pain scores at rest and during mobilization up to 72 hours postoperatively and a lower need for opioids. The study of Andersson et al used infiltration, followed by bolus the next day, and demonstrated less pain and opioid consumption from 4 hours postoperatively up to 2 weeks, whereas joint function was improved at 1 week. Murphy et al compared infiltration with 60 mL levobupivacaine 2.5 mg/mL versus placebo. The morphine consumption was reduced by 4% in the LIA group during the first 12 hours, but quality of analgesia and sideeffects were similar. In the placebo-controlled study of Lunn et al, the placebo group received an optimal multimodal analgesic regimen of acetaminophen, elecoxib, and gabapentin with equal results as in the LIA group. Andersen et al compared LIA with top-up injections to epidural analgesia and found less opioid consumption, better mobilization, and shorter hospital stay with LIA. Specht et al found that a top-up bolus at 10 and 22 hours was no better than placebo in patients who received perioperative LIA. Rikalainen-Salmi et al compared LIA with a top-up morning after surgery to morphine 0.1 mg given as a part of the spinal anesthetic. The LIA technique resulted in less opioid consumption on the day of surgery and better early mobilization, without any difference in pain scores and patient satisfaction; the LIA top-up, however, did not confer any benefit. Taken together, LIA appears to be better than placebo for hip replacement surgery, whereas in comparison with other optimized methods, the results are mixed. Whether the adjuncts in the LIA solutions have a specific local effect compared with systemic administration has not been studied properly in hip surgery.
LOCAL INFILTRATION ANALGESIA FOR KNEE ARTHROPLASTY
A wide range of LIA techniques for total knee arthroplasty have been described in recent literature. In earlier studies, the volume of the mixture of local anesthetics and adjuvants used was lower than 50 mL. In the study of Kerr and Kohan, a mixture of ropivacaine (2 mg/mL, maximum 300 mg), ketorolac (30 mg), and epinephrine (10 μg/mL) was diluted with saline to a volume of 150–170 mL. The mixture was injected into the different knee structures during the knee arthroplasty in three stages: after preparation of bone surfaces (30–50 mL), after insertion of the prosthesis components (35–50 mL), and into subcutaneous tissue (25–50 mL). At the end of surgery, an 18-gauge epidural catheter was inserted with the catheter tip placed anterior to the posterior capsule, and 10–15 mL of the mixture were injected. This catheter was used for a further injection 15–20 hours postoperatively, when another 50 mL of the mixture were injected through the catheter.
To our knowledge, the first randomized studies regarding high-volume intra- or periarticular multimodal drug injection in total knee arthroplasty were published by Busch et al and Vendittoli el al. Several reviews regarding LIA following total knee arthroplasty have been published recently. The most recent review by Gibbs et al included a total of 29 randomized studies. However, this number in Gibbs and colleagues’ review also included some local infiltration studies in which low volumes of LIA (<100 mL) were used. Most of the individual studies lacked adequate blinding. However, when comparing different treatment modalities (eg, LIA vs. epidural analgesia), a proper trial would require invasive procedures in the placebo group, which may be unethical and therefore difficult to execute. Andersen and colleagues conducted a double-blind, placebo-controlled study in patients undergoing bilateral total knee arthroplasty and demonstrated the effectiveness of the LIA technique. However, based on the current information, effectiveness of a postoperative top-up dose is questionable and may carry a risk of infection.Regardless, several authors reported that postoperative top-up injections are associated with less opioid consumption and lower pain scores. To date, no study reported an increased incidence of postoperative infections with LIA catheters.
NYSORA Tips
Is LIA of sufficient clinical benefit to warrant routine clinical use?
A. Hip replacement surgery
LIA is not better than preoperative spinal anesthesia followed by multimodal analgesia with acetaminophen + NSAID/COX-2 inhibitor + either glucocorticoid or gabapentinoid.
In patients in whom multimodal therapy is contraindicated LIA may be a valuable analgesic method, reducing the need for rescue opioids.
B. Knee replacement surgery
Yes, even with an optimal preoperative spinal (or other nerve blocks) and three-component systemic multimodal analgesia, preoperative LIA still provides additional analgesia for 24–48 hours.
Compared to no injections or saline injections, all studies showed LIA had a beneficial analgesic effect. The two studies comparing LIA to femoral nerve block, however, showed conflicting results. While Toftdahl and colleagues concluded that LIA was superior to a continuous femoral nerve block regarding opioid consumption and pain scores during the first postoperative day, Carli et al suggested that the femoral nerve is better. Of note, patients in the Carli et al study received an infiltration with ropivacaine, ketorolac, and epinephrine into the posterior capsule of the knee joint during surgery (in addition to LIA or femoral nerve block). Both studies comparing LIA with epidural analgesia (Table 1) demonstrated that LIA can reduce both postoperative opioid consumption and postoperative pain scores.
TABLE 1. Comparison of local infiltration analgesia with other techniques.
| Author (Reference Number) | Patients (n) | Groups Intraoperative | Treatment Intraoperative | Groups Postoperative | Treatment Postoperative | Findings of LIA |
|---|---|---|---|---|---|---|
| 1. Studies Comparing LIA With No Injections or Saline Injections | ||||||
| Busch et al (2006)37 | 64 | LIA (100 mL) No injection | 400 mg ropivacaine 30 mg ketorolac 5 mg epimorphine 0.6 mg epinephrine | All patients | No injections into the knee Morphine PCA | Opioid consumption ↓ (0–24 h) Pain ↓ (0–4 h) |
| Vendittoli et al (2006)38 | 42 | LIA (160 mL) No injection | 275 mg ropivacaine 30 mg ketorolac 0.5 mg epinephrine | LIA (15 mL) No injection | 150 mg ropivacaine after 16–24 h | Opioid consumption ↓ (0–48 h) Pain ↓ (0–48 h) |
| Andersen et al (2008)8 | 12 (24 knees) | LIA (170 mL) Control | 340 mg ropivacaine 1.7 mg epinephrine Saline (170 mL) | LIA Control | 8 h: 40 mg ropivacaine + 0.2 mg epinephrine (20 mL) 24 h: 100 mg ropivacaine + 0.5 mg epinephrine (50 mL) 8 h + 24 h: saline (20 + 50 mL) | Pain ↓ (0–24 h) |
| Kazak et al (2010)45 | 60 | LIA (150 mL) LIA (150 mL) Control | 200 mg bupivacaine 0.5 mg epinephrine 200 mg levobupivacaine 0.5 mg epinephrine Saline (150 mL) | LIA (25 mL) LIA (25 mL) Control | 10 h + 22 h: 120 mg bupivacaine 10 h + 22 h: 120 mg levobupivacaine + 0.5 mg epinephrine 10 h + 22 h: saline (25 mL + 25 mL) | Opioid consumption ↓ (0–48 h) Pain ↓ (0–48 h) |
| Essving et al (2010)43 | 48 | LIA (166 mL) No injection | 400 mg ropivacaine 30 mg ketorolac 0.5 mg epinephrine | LIA (22 mL) Control | 21 h: 200 mg ropivacaine + 30 mg ketorolac + 0.1 mg epinephrine 21 h: saline (22 mL) | Opioid consumption ↓ (0–48 h) Pain ↓ (0–27 h) |
| 2. Studies Comparing LIA With Femoral Nerve Block | ||||||
| Carli et al (2010)46 | 40 | LIA (102 mL) → peri- and intra-articularly FNB (8mL) All patients: → Infiltration postoperative capsule (51 mL) | 200 mg ropivacaine 30 mg ketorolac 0.5 mg epinephrine + 8 mL saline in femoral catheter 16 mg ropivacaine + 100 mL saline into periarticular catheter 100 mg ropivacaine 15 mg ketorolac 0.25 mg epinephrine | LIA (50) mL FNB | 24 h: 250 mg ropivacaine + 30 mg ketorolac + 0.25 mg epinephrine + 8 mL/h saline through femoral catheter for 48 h Ropivacaine 2 mg/mL 8mL/h for 48 h + 50 mL saline into periarticular catheter 24 h after surgery | Opioid consumption ↑ (0–48 h) for LIA group (peri- and intra-articular infiltrations) |
| Toftdahl et al (2007)44 | 77 | LIA (152 mL) FNB (20 mL) | 300 mg ropivacaine 30 mg ketorolac 0.5 mg epinephrine 200 mg ropivacaine 4 mg morphine + 50 mg bupivacaine through drain (intra-articular) | LIA (22 mL) FNB | 12 h + 24 h: 200 mg ropivacaine + 30 mg ketorolac + 0.5 mg epinephrine Ropivacaine 2 mg/mL at 10 mL/h for 48 h | Opioid consumption ↓ (0–24 h) Pain ↓ (0–24 h) |
| 3. Studies Comparing LIA With Epidural Analgesia | ||||||
| Andersen et al (2010)47 | 40 | LIA (152 mL) EDA | 300 mg ropivacaine 30 mg ketorolac 0.5 mg epinephrine Test dose 3 mL: lidocaine + epinephrine | LIA EDA | Continuous infusion at 4 mL/h for 48 h (380 mg ropivacaine, 60 mg ketorolac) Continuous infusion at 4 mL/h for 48 h (ropivacaine 2 mg/mL) Ketorolac 15 mg IV × 6 | Opioid consumption ↓ (0–48 h) Pain ↓ (0–72 h) |
| Spreng et al (2010)14 | 99 | LIA (150 mL) LIA IV (150mL) EDA | 150 mg ropivacaine 30 mg ketorolac 5 mg morphine 0.5 mg epinephrine 6 mL saline IV 150 mg ropivacaine 0.5 mg epinephrine 6 mL saline (LIA) 30 mg ketorolac IV 5 mg morphine IV Test dose 3 mL: lidocaine + epinephrine | LIA (20 mL) LIA IV (20 mL) EDA | 22–24 h: 142.5 mg ropivacaine + 30 mg ketorolac 1 mL saline IV 22–24 h: 142.5 mg ropivacaine + 1 mL saline (LIA) 1 mL ketorolac IV 6–10 mL/h for 48h : fentanyl 2 μg/mL + bupivacaine 1 mg/mL + epinephrine 1 μg/mL | Opioid consumption ↓ (0–72 h) Pain ↓ (24–72 h) |
| 4. Studies Comparing Different LIA Techniques | ||||||
| Andersen et al (2008)49 | 48 | LIA ± compression bandage | 340 mg ropivacaine 1 mg epinephrine (170 mL) | LIA ± compression bandage | 6 h + 12 h: 40 mg ropivacaine + 0.2 mg epinephrine (20 mL) 24 h: 100 mg epinephrine (50 mL) | Pain ↓ (0–8h) with compression bandage |
| Andersen et al (2010;p984) | 43 | All patients: LIA (150 mL) | 300 mg ropivacaine 1 mg epinephrine | LIA (20 mL) LIA (10 mL) | 6 h + 24 h: ropivacaine 5 mg/mL 6 h + 24 h: ropivacaine 10 mg/mL | No differences between the groups |
| Andersen et al (2010;p543)42 | 16 (32 knees) | LIA (150 mL) LIA (100 mL) | 200 mg ropivacaine 1 mg epinephrine 100 mg ropivacaine to superficial layers 200 mg ropivacaine 1 mg epinephrine 50 mL saline to superficial layers | LIA (20 mL) Control (20 mL) | 24 h: 100 mg ropivacaine subcutaneously 24 h: saline subcutaneously | Pain ↓ (0–6 h) with infiltration of superficial layers, but no difference after 24 h |
| Andersen et al (2010;p904) | 60 | All patients: LIA (150 mL) | 300 mg ropivacaine 1 mg epinephrine | LIA (20 mL) intracapsular LIA (20 mL) intra-articular | 6 h + 24 h: 100 mg ropivacaine | No differences between the groups |
| Andersen et al (2008;p800)49 | 32 | All patients: LIA (170 mL) | 340 mg ropivacaine 1.2 mg epinephrine | LIA LIA | 6 h + 12 h + 24 h: 40 mg ropivacaine + 0.2 mg epinephrine (20 mL). Additional 60 mg ropivacaine + 0.3 mg epinephrine (30 mL) during catheter retraction 6 h + 12 h + 24 h: 40 mg ropivacaine + 0.2 mg epinephrine (20 mL). Additional 30 mL saline during catheter retraction | No differences between the groups |
| Spreng et al (2010)14 | 99 | LIA (150 mL) LIA IV (150 mL) EDA | 150 mg ropivacaine 30 mg ketorolac 5 mg morphine 0.5 mg epinephrine 6 mL saline IV 150 mg ropivacaine 0.5 mg epinephrine 6 mL saline (LIA) 30 mg ketorolac IV 5 mg morphine IV Test dose 3 mL: lidocaine + epinephrine | LIA (20 mL) LIA IV (20 mL) EDA | 22–24 h: 142.5 mg ropivacaine + 30 mg ketorolac 1 mL saline IV 22–24 h: 142.5 mg ropivacaine + 1 mL saline (LIA) 1 mL ketorolac IV 6–10 mL/h for 48 h (fentanyl 2 μg/mL + bupivacaine 1 mg/mL + epinephrine 1 μg/mL) | Opioid consumption ↓ (0–72 h) when ketorolac and morphine were infiltrated into the knee Pain ↓ (0–72 h) when ketorolac and morphine were infiltrated into the knee |
| Andersen et al (2013)48 | 60 | LIA (151 mL) LIA (151 mL) | 300 mg ropivacaine 30 mg ketorolac 300 mg ropivacaine 1 mL saline | LIA (10 mL) LIA (10 mL) | Every 6 h for 48 h: 100 mg ropivacaine + 15 mg ketorolac Every 6 h for 48 h: 100 mg ropivacaine + 1 mL | Opioid consumption ↓ (0–48 h) in the ketorolac group Pain ↓ (0–48 h) in the ketorolac group |
EDA = epidural analgesia; IV = intravenous; LIA = local infiltration analgesia; FNB = femoral nerve block; PCA = patient-controlled analgesia.
Moreover, LIA was associated with faster mobilization and earlier readiness for hospital discharge. The LIA recipe (ie, volume, content, as well as the use of adjuvants) is not well defined. Two recently published studies have shown that ketorolac is an important factor in the LIA mixture. Moreover, Spreng and colleagues showed that local administration of ketorolac and morphine may also have a local effect. Application of a compression bandage for 24 hours postoperatively and infiltration of superficial layers in the knee joint with local anesthetics are also important for the effectiveness of the LIA. Several recent studies have been published regarding continuous infusion of local anesthetics with or without adjuvants. Gomez-Cardero and Rodriguez-Merchán50 compared continuous LIA for 60 hours (ropivacaine) with placebo and found reduced opioid consumption and pain scores for the first 3 days after surgery. Ong and colleagues examined the use of continuous intra-articular infusion or bolus dose and demonstrated reduced opioid consumption and lower pain scores compared to intravenous pain treatment only.
LOCAL INFILTRATION ANALGESIA RECIPES
LIA in Total Knee Arthroplasty
The LIA Recipe
The solution, which is infiltrated into the knee, should be prepared under aseptic conditions (Figure 1). The total volume of the solution is 150 mL and contains the following:
•200 mg ropivacaine (2 mg/mL) (amount of infiltrated ropivacaine in published studies varied: 150 mg, 200 mg, 300 mg,1 400 mg)
•30 mg ketorolac (30 mg/mL)
•0.5 mg epinephrine (1 mg/mL)
•Isotonic saline (dilution to 150 mL total)

FIGURE 1. In the operating room, a sterile bag with ropivacaine from the pharmacy receives the addition of 30 mg (1 mL) ketorolac and 0.5 mg (0.5 mL) epinephrine.
NYSORA Tips
Although there are numerous recipes, the following formula is efficacious for both knee and hip replacement surgery:
• Total volume 150 mL (add normal saline according to the number of milliliters used by the other drugs)
• 200 mg ropivacaine (use any practical preparation: 2, 5, 7.7 mg/mL, dilute)
• 30 mg ketorolac
The addition of epinephrine (eg, 0.5 mg in 150 mL) may have a beneficial effect on hemostasis.
The solution, which is infiltrated into the knee catheter postoperatively (top-up dose), should also be prepared under aseptic conditions. The total volume of the solution should be 15–20 mL for each injection and contains the following:
•150 mg ropivacaine (5–7.5 mg/mL)
•30 mg ketorolac (30 mg/mL)
•Isotonic saline (dilution to 15–20 mL total)
Injection Technique
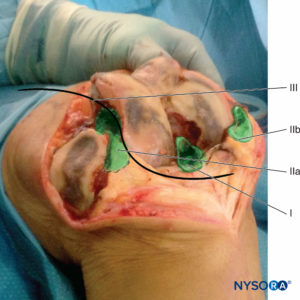
• After surgical preparation of the knee joint, 40 mL of the LIA solution are infiltrated into posterior capsule structures by the orthopedic surgeon. A “moving needle technique” is preferable (Figure 2, area marked I).
• After the joint replacement, 50–60 mL of the solution are infiltrated circularly around the prosthesis (Figure 2, area marked IIa and IIb).
• An 18-gauge epidural catheter with a bacterial filter can be placed from the lateral side into the knee joint (optional) (Figure 2, sinusoidal line, marked III;Figure 3).
• After closure of the capsule, another 50 mL of the solution are infiltrated into the fascia and subcutis (Figure 4).
• If a catheter is used, 10 mL of the solution are injected through the knee catheter at the end of surgery to verify fluid flow (Figure 5).
• Aseptic top-up injections into the knee catheter (15–20 mL, according to the actual knee size) after 8, 16, and 24 hours (Figure 6).
• The knee catheter is removed during the last injection with subsequent spread into the fascia and subcutis.

FIGURE 5. The last injection through the catheter: 10 mL for analgesia and for testing the catheter.
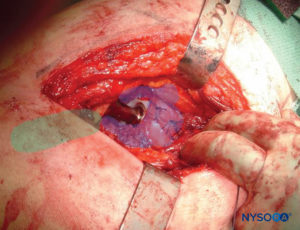
FIGURE 6. Sites for infiltration of LIA in hip arthroplasty: transparent blue area for first injection (see text) and transparent green area for the second injection.
LIA in Total Hip Arthroplasty
The LIA Cocktail
The LIA cocktail solution, which is infiltrated into the hip, should be prepared under aseptic conditions (Figure 1). The total volume of the solution is 100 mL and contains the following:
• 200 mg ropivacaine (2 mg/mL)
• 30 mg ketorolac (30 mg/mL)
• 0.5 mg epinephrine (1 mg/mL)
• Isotonic saline (dilution to 100 mL total)
Injection Technique
Depending on the size of the surgical incision and choice of surgical approach, 100 mL of the LIA solution are injected in two stages:
• After surgical preperation of the acetabulum, 50 mL of the solution are infiltrated into capsule structures (if remaining), into adductor muscles and into the gluteus medius muscle.
NYSORA Tips
Should we include catheters for peri- or intra-articular infusion/top-ups when using LIA?
• No, there is strong evidence for no benefit of catheter after hip prosthesis.
• After knee prosthesis, the evidence is more conflicting, mostly indicating no extra effect when compared with optimal multimodal systemic analgesia, but some effect if not all components of the multimodal regimes are used.
• A recent report of an increased rate of infections with catheters, added to anecdotal reports of similar results, added to the evidence in disfavor of catheter use.
• After insertion of the femoral component, another 50 mL are infiltrated into the external rotators (quadratus femoris muscle, obturator muscle, and the tendon of the gluteus maximus muscle) (Figure 6).
REFERENCES
- Kerr DR, Kohan L: Local infiltration analgesia: A technique for the control of acute postoperative pain following knee and hip surgery: A case study of 325 patients. Acta Orthop 2008;79:174–183.
- Goodwin RC, Amjadi F, Parker RD: Short-term analgesic effects of intra-articular injections after knee arthroscopy. Arthroscopy 2005;21: 307–312.
- Brummett CM, Williams BA: Additives to local anesthetics for peripheral nerve block. Int Anesthesiol Clin 2011;49:104–116.
- Ilfeld BM: Continuous peripheral nerve blocks: A review of the published evidence. Anesth Analg 2011;113:904–925.
- Smoot JD, Bergese SD, Onel E, et al: The efficacy and safety of DepoFoam bupivacaine in patients undergoing bilateral, cosmetic, submuscular augmentation mammaplasty: A randomized, double-blind, active-control study. Aesthet Surg J 2012;32:69–76.
- Kehlet H, Andersen LO: Local infiltration analgesia in joint replacement: The evidence and recommendations for clinical practice. Acta Anaesthesiol Scand 2011;55:778–784.
- Raeder J, Spreng UJ: Local-infiltration anaesthesia (LIA): Post-operative pain management revisited and appraised by the surgeons? Acta Anaesthesiol Scand 2011;55:772–774.
- Andersen LO, Husted H, Otte KS, et al: High-volume infiltration analgesia in total knee arthroplasty: A randomized, double-blind, placebo-controlled trial. Acta Anaesthesiol Scand 2008;52:1331–1335.
- Aasbo V, Thuen A, Raeder J: Improved long-lasting postoperative analgesia, recovery function and patient satisfaction after inguinal hernia repair with inguinal field block compared with general anesthesia. Acta Anaesthesiol Scand 2002;46:674–678.
- Parker RD, Streem K, Schmitz L, Martineau PA: Efficacy of continuous intra-articular bupivacaine infusion for postoperative analgesia after anterior cruciate ligament reconstruction: A double-blinded, placebo-controlled, prospective, and randomized study. Am J Sports Med 2007; 35:531–536.
- Rosseland LA, Helgesen KG, Breivik H, Stubhaug A: Moderate-to-severe pain after knee arthroscopy is relieved by intraarticular saline: a randomized controlled trial. Anesth Analg 2004;98:1546–1551, table.
- Lenz H, Raeder, Heyerdahl F, et al: Modulation of remifentanil-induced postinfusion hyperalgesia by parecoxib or ketorolac in humans. Pain 2011;100–110.
- Dye SF: The pathophysiology of patellofemoral pain: A tissue homeostasis perspective. Clin Orthop Relat Res 2005;100–110.
- Spreng UJ, Dahl V, Hjall A, et al: High-volume local infiltration analgesia combined with intravenous or local ketorolac + morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth 2010;105: 675–682.
- Affas F, Nygards EB, Stiller CO, et al: Pain control after total knee arthroplasty: A randomized trial comparing local infiltration anesthesia and continuous femoral block. Acta Orthop 2011;82(4):441–447.
- Lund J, Jenstrup MT, Jaeger P, et al: Continuous adductor-canal-block for adjuvant post-operative analgesia after major knee surgery: Preliminary results. Acta Anaesthesiol Scand 2011;55:14–19.
- Essving P, Axelsson K, Åberg E, et al: Local infiltration analgesia (LIA) vs. intrathecal morphine for postoperative pain management following total knee arthroplasty. A randomized, controlled trial. Anesth Analg 2011;113: 926–933.
- Sites BD, Beach M, Gallagher JD, et al: A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg 2004;99:1539–1543.
- Hval K, Thagaard KS, Schlichting E, Raeder J: The prolonged postoperative analgesic effect when dexamethasone is added to a nonsteroidal antiinflammatory drug (rofecoxib) before breast surgery. Anesth Analg 2007;105:481–486.
- Zhang J, Ho KY, Wang Y: Efficacy of pregabalin in acute postoperative pain: A meta-analysis. Br J Anaesth 2011;106:454–462.
- Banks A: Innovations in postoperative pain management: Continuous infusion of local anesthetics. AORN J 2007;85:904–914.
- Piper SL, Kramer JD, Kim HT, Feeley BT: Effects of local anesthetics on articular cartilage. Am J Sports Med 2011;39:2245–2253.
- McCarthy D, Iohom G: Local infiltration analgesia for postoperative pain control following total hip arthroplasty: A systematic review. Anesthesiol Res Pract 2012;2012:709531.
- Rikalainen-Salmi R, Forster JG, Makela K, et al: Local infiltration analgesia with levobupivacaine compared with intrathecal morphine in total hip arthroplasty patients. Acta Anaesthesiol Scand 2012;56: 695–705.
- Murphy TP, Byrne DP, Curtin P, et al: Can a periarticular levobupivacaine injection reduce postoperative opiate consumption during primary hip arthroplasty? Clin Orthop Relat Res 2012;470:1151–1157.
- Otte K, Husted H, Andersen L, et al: Local infiltration analgesia in total knee arthroplasty and hip resurfacing: A methodological study. Acute Pain 2008;10:111–116.
- Parvataneni HK, Shah VP, Howard H, et al: Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: A prospective randomized study. J Arthroplasty 2007;22:33–38.
28. Busch CA, Whitehouse MR, Shore BJ, et al: The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res 2010;468:2152–2159. - Bianconi M, Ferraro L, Traina GC, et al: Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth 2003;91:830–835.
- Andersen LJ, Poulsen T, Krogh B, Nielsen T: Postoperative analgesia in total hip arthroplasty: A randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop 2007;78:187–192.
- Lunn TH, Husted H, Solgaard S, et al: Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: A randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2011;36: 424–429.
- Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Soballe K: Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: A randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop 2007;78:180–186.
- Specht K, Leonhardt JS, Revald P, et al: No evidence of a clinically important effect of adding local infusion analgesia administrated through a catheter in pain treatment after total hip arthroplasty. Acta Orthop 2011;82:315–320.
- Badner NH, Bourne RB, Rorabeck CH, et al: Intra-articular injection of bupivacaine in knee-replacement operations. Results of use for analgesia and for preemptive block. J Bone Joint Surg Am 1996;78:734–738.
- Mauerhan DR, Campbell M, Miller JS, et al: Intra-articular morphine and/or bupivacaine in the management of pain after total knee arthroplasty. J Arthroplasty 1997;12:546–552.
- Ritter MA, Koehler M, Keating EM, et al: Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br 1999; 81:301–303.
- Busch CA, Shore BJ, Bhandari R, et al: Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am 2006;88:959–963.
- Vendittoli PA, Makinen P, Drolet P, et al: A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am 2006;88:282–289.
- Morin AM, Wulf H: High volume local infiltration analgesia (LIA) for total hip and knee arthroplasty: A brief review of the current status [in German]. Anasthesiol Intensivmed Notfallmed Schmerzther 2011;46: 84–86.
40. Ganapathy S, Brookes J, Bourne R: Local infiltration analgesia. Anesthesiol Clin 2011;29:329–342. - Gibbs DM, Green TP, Esler CN: The local infiltration of analgesia following total knee replacement: A review of current literature. J Bone Joint Surg Br 2012;94:1154–1159.
- Andersen LO, Husted H, Kristensen BB, et al: Analgesic efficacy of subcutaneous local anaesthetic wound infiltration in bilateral knee arthroplasty: A randomised, placebo-controlled, double-blind trial. Acta Anaesthesiol Scand 2010;54:543–548.
- Essving P, Axelsson K, Kjellberg J, et al: Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty. Acta Orthop 2010;81:354–360.
- Toftdahl K, Nikolajsen L, Haraldsted V, et al: Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: A randomized clinical trial. Acta Orthop 2007;78: 172–179.
- Kazak BZ, Aysu SE, Darcin K, et al: Intraarticular levobupivacaine or bupivacaine administration decreases pain scores and provides a better recovery after total knee arthroplasty. J Anesth 2010;24:694–699.
- Carli F, Clemente A, Asenjo JF, et al: Analgesia and functional outcome after total knee arthroplasty: Periarticular infiltration vs continuous femoral nerve block. Br J Anaesth 2010;105:185–195.
- Andersen KV, Bak M, Christensen BV, et al: A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop 2010;81:606–610.
- Andersen KV, Nikolajsen L, Haraldsted V, et al: Local infiltration
analgesia for total knee arthroplasty: Should ketorolac be added? Br J Anaesth 2013;111:242–248. - Andersen LO, Husted H, Otte KS, et al: A compression bandage improves
local infiltration analgesia in total knee arthroplasty. Acta Orthop 2008;79:806–811. - Gomez-Cardero P, Rodriguez-Merchan EC: Postoperative analgesia in
TKA: Ropivacaine continuous intraarticular infusion. Clin Orthop Relat Res 2010;468:1242–1247. - Ong JC, Chin PL, Fook-Chong SM, et al: Continuous infiltration of local anaesthetic following total knee arthroplasty. J Orthop Surg (Hong Kong)
2010;18:203207. - Essving P, Axelsson K, Kjellberg J, et al: Reduced hospital stay, morphine consumption, and pain intensity with local infiltration analgesia after
unicompartmental knee arthroplasty. Acta Orthop 2009;80:213–219. - Ali A, Sundberg M, Hansson U, Malmvik J, Flivik G: Doubtful effect of
continuous intraarticular analgesia after total knee arthroplasty. Acta Orthop 2015;86:373–377.