Carlo D. Franco, Bram Byloos, and Ilvana Hasanbegovic
INTRODUCTION
The supraclavicular block is one of several techniques used to anesthetize the brachial plexus. The block is performed at the level of the brachial plexus trunks where almost the entire sensory, motor, and sympathetic innervation of the upper extremity is carried in just three nerve structures confined to a very small surface area. Consequently, this technique typically provides a predictable, dense block with rapid onset. In 1911, Georg Hirschel described a surgical approach to the brachial plexus in the axilla. A few months later, Diedrich Kulenkampff, in Germany, performed the first percutaneous supraclavicular approach, reportedly on himself. The technique was published in 1928 by Kulenkampff and Persky. As they described it, the technique was performed with the patient in the sitting position (“a regular chair will suffice”) or in the supine position with a pillow between the shoulders. The operator sat on a stool at the side of the patient. The needle was inserted above the midpoint of the clavicle where the pulse of the subclavian artery could be felt and was directed medially toward the spinous process of T2 or T3. Kulenkampff ‘s familiarity with brachial plexus anatomy allowed him to recognize that “the best way to reach the trunks was in the neighborhood of the subclavian artery over the first rib.” His technique was also simple: “all the branches of the plexus could be anesthetized through one injection.” These two assertions are still valid today. Unfortunately. his advice on needle direction carried an inherently high risk of pneumothorax. The popularity of the supraclavicular block remained unrivaled during the entire first half of the 20th century until well after World War II. During this time the technique underwent several modifications, most of them intended to reduce the risk of pneumothorax. The introduction of axillary techniques by Accardo and Adriani in 1949 and by Burnham10 in 1958 marked the beginning of the decline in enthusiasm for the supraclavicular block.
The axillary block was particularly popularized after a publication in the journal Anesthesiology by Rudolph De Jong in 1961. The paper was based on cadaver dissections and included the now well-known calculation of 42 mL as the volume needed to fill a cylinder 6 cm long (axillary sheath); according to De Jong, this dose “should be sufficient to completely bathe all branches of the brachial plexus.” The article was also critical of the supraclavicular approach. Coincidentally, the same journal published a paper by Brand and Papper, who compared axillary and supraclavicular techniques and warned of the 6.1% rate of pneumothorax frequently quoted for supraclavicular block. More modern modifications of supraclavicular block include Alon Winnie and Vincent Collins’s subclavian perivascular technique and the “plumb-bob” technique of Brown and collaborators. The former is more a concept than a radically different technique, stating that plexus anesthesia is performed around a main vessel (perivascular) and within the confines of a sheath. Otherwise, their technique is similar to Murphey’s, who in 1944, described a single-injection technique performed just lateral to the anterior scalene muscle directing the needle caudad.
The plumb-bob technique, published in 1993, is based on cadaver dissections and magnetic resonance imaging performed on volunteers. In this technique, the needle is introduced above the clavicle, just lateral to the sternocleidomastoid (SCM) muscle and advanced perpendicularly to the plexus in an anteroposterior direction. If the needle misses the plexus, the pleural dome could be penetrated. Many investigators appear to perceive the supraclavicular block as being complex and associated with a significant risk of pneumothorax. However, its rapid onset, dense and predictable anesthesia, and high success rate make it a very useful approach, which, according to Brown and collaborators, is “unrivaled” by other techniques. Indeed, in our practice, the supraclavicular approach is the cornerstone of distal upper extremity regional anesthesia, and we use it extensively with a very low rate of complications.
INDICATIONS
The supraclavicular block provides anesthesia and analgesia to the upper extremity below the shoulder. It is an excellent choice for elbow and hand surgery.
CONTRAINDICATIONS
General contraindications to the use of this technique are those that apply to any regional block, such as local infection, significant coagulation abnormalities, and inability to cooperate during block placement or surgery. Like interscalene block, supraclavicular block is not used bilaterally or in patients with respiratory compromise because of the potential risk of pneumothorax or phrenic nerve block.
ANATOMY OF THE BRACHIAL PLEXUS ABOVE THE CLAVICLE
The brachial plexus is formed by five roots originating from the ventral divisions of C5 through T1. The roots lie between the anterior and middle scalene muscles (Figure 1). The anterior scalene muscle originates from the anterior tubercles of the transverse processes of C3 through C6 and inserts on the scalene tubercle of the upper surface of the first rib. The middle scalene muscle originates in the posterior tubercles of the transverse processes of C2 through C7 and inserts on the upper surface of the first rib behind the subclavian groove. The five roots converge toward one another to form three trunks—upper, middle, and lower—which are stacked one on top of the other as they traverse the triangular interscalene groove, formed between the anterior and middle scalene muscles. This space becomes wider in the anteroposterior plane as the muscles approach their insertion on the first rib. The subclavian artery accompanies the brachial plexus in the interscalene groove anterior to the lower trunk. Although the roots of the plexus are long, the trunks are almost as short as they are wide, soon giving rise to anterior and posterior divisions as they reach the clavicle.
Figure 1 shows the clinical anatomy of the brachial plexus and surrounding structures in the supraclavicular area. The pleura can potentially be injured in two places during a supraclavicular block; the pleural dome and the first intercostal space. The pleural dome is the apex of the parietal pleura, circumscribed by the first rib. The first rib is a short, broad, and flattened bone shaped like the letter C. It’s medial border forms the outer boundary of the pleural dome. The anterior scalene, by inserting in this border of the first rib, comes in contact medially with the pleural dome. There is no pleural dome lateral to the anterior scalene muscle. The first intercostal space on the other hand, is for the most part infraclavicular (see Figure 1) and consequently should not be reached when a supraclavicular block is properly performed.
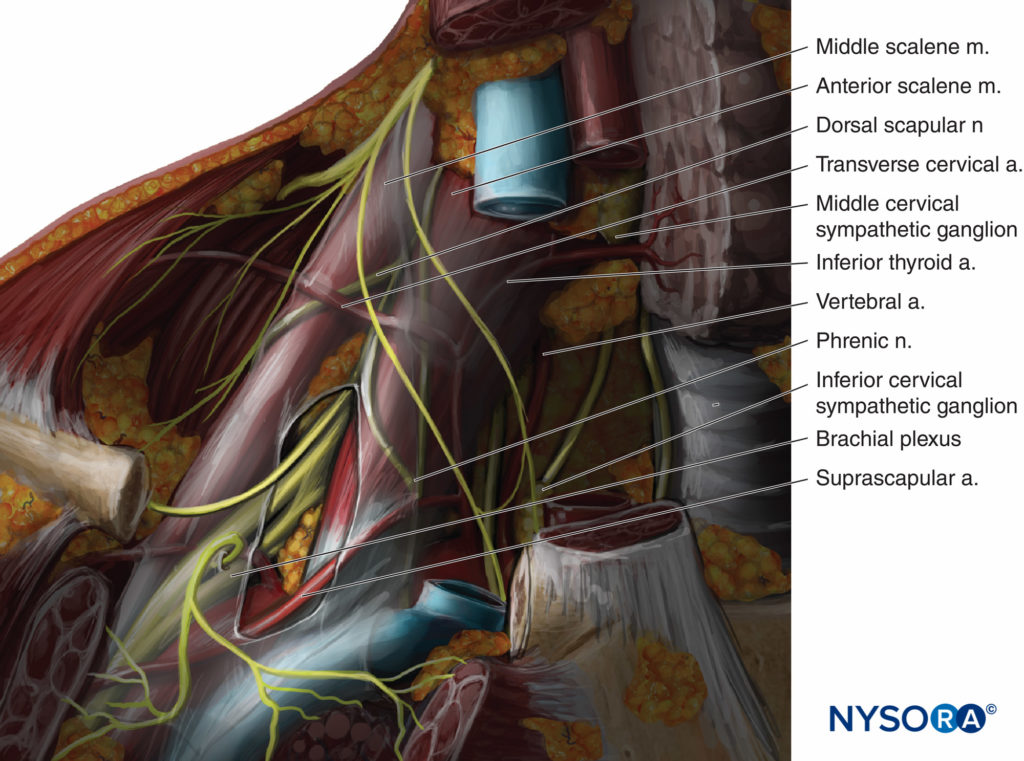
FIGURE 1. Anatomy of the brachial plexus at the low interscalene space and supraclavicular area.
NYSORA Tips
- With the shoulder pulled down, the three trunks of the brachial plexus are located above the clavicle; therefore, the block needle should never need to reach below the clavicle during a supraclavicular block.
- The first intercostal space is located below the clavicle, thus its penetration is unlikely during a properly performed supraclavicular block.
- The needle should never cross the parasagittal plane medial to the anterior scalene muscle because of the risk of pneumothorax.
- The SCM muscle inserts on the medial third of the clavicle, and the trapezius muscle on the lateral third of it, leaving the middle third for the neurovascular bundle. These proportions are maintained regardless of patient’s size.
- Because the brachial plexus moves from medial to lateral as it descends, the higher in the supraclavicular area the more medial (closer to the SCM) the plexus is located.
LANDMARKS
The technique described in this chapter combines the simplicity of the original single-injection Kulenkampff technique with important anatomic principles, which should make the technique safer than the original description. The main landmarks for this block are the lateral insertion of the SCM muscle in the clavicle, the clavicle itself, and the patient’s midline. These three landmarks are easily identifiable in the majority of patients.
EQUIPMENT
- Gloves
- Antiseptic solution for skin disinfection
- Marking pen
- Sterile gauze
- Two 20-mL syringes for local anesthetic solution
- One 1-mL syringe with a 25-gauge needle for skin wheal
- One 5-cm, short-beveled, 22-gauge insulated needle
- Surface electrode
- Nerve stimulator
- Injection pressure monitor
Learn more about Equipment for Regional Anesthesia.
TECHNIQUE
Ideally, the block is performed in a room dedicated to regional anesthesia with American Society of Anesthesiologists (ASA) standard monitors, an oxygen source, suctioning, and resuscitation equipment and drugs including lipid emulsion. A contingency plan for emergencies must be in place to deal safely and expeditiously with any emergency that might arise. If not contraindicated, this block is best performed after premedication (e.g., midazolam 1 mg plus fentanyl 50 mcg IV for the average adult). In young and healthy patients, this dose can be repeated as necessary. The patient is best kept sedated but cooperative and able to relate pain or any undue discomfort. The block is performed with the patient in a semisitting position with the head rotated to the opposite side as shown in Figure 2A. The semisitting position is more comfortable than the supine position both for the patient and the operator. Because patient positioning is very important in regional anesthesia, the operator should not try to recognize any landmarks until the patient has adopted the desired position. The patient is asked to lower the shoulder and flex the elbow, so the forearm rests on the lap. The wrist is supinated so the palm of the hand faces the patient’s face, as shown in Figure 2B. This maneuver allows for detection of any subtle finger movement produced by nerve stimulation. If the patient cannot supinate their wrist, a roll is placed under it so the fingers are free to move. The operator usually stands on the side to be blocked, so for a left-side block, the palpation is done with the left hand and the needle is manipulated with the right (see Figure 2B). For a right-side block, the operator manipulates the needle with the left hand and palpates with the right. However, the operator may choose to manipulate the needle with their preferred hand regardless of the block side.
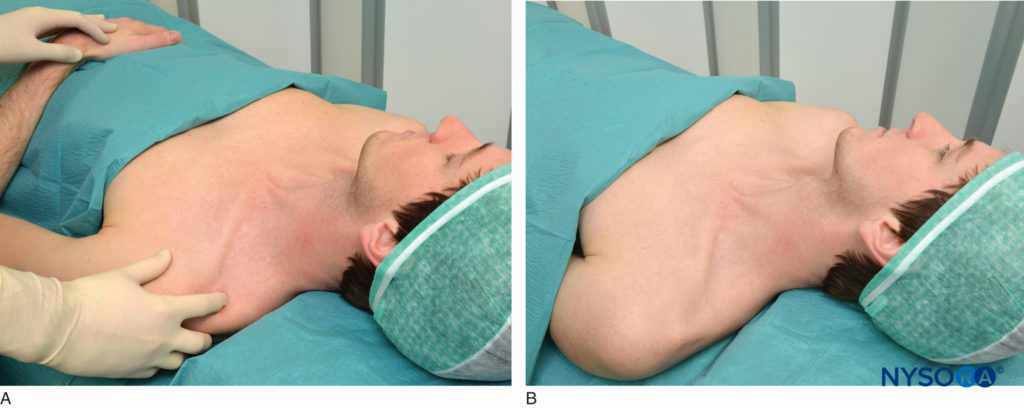
FIGURE 2 A: Patient positioning. The patient lies in a semisitting or supine position with the head turned away from the side to be blocked. B: The shoulder is down, the elbow is flexed, and the palm of the hand rests on the patient’s lap while it is turned toward his face.
Point of Needle Entrance
With the patient in the described semisitting position and the shoulder down, the lateral (posterior) border of the SCM muscle is identified and followed distally to the point where it meets the clavicle. This particular point is marked on the skin over the clavicle, as shown in Figure 3. The lateral border of the SCM is usually clearly visible at the level where the external jugular vein crosses it. From this level, the border can be traced caudally to the point where it meets the clavicle. A parasagittal line (parallel to the midline) is drawn at this level to recognize an area medial to it that is at risk for pneumothorax. The point of needle entrance is found lateral to this parasagittal plane, separated by a distance we call “margin of safety.” This distance is about 1 in. (2.5 cm) lateral to the insertion of the SCM on the clavicle, as shown in Figure 4. The margin of safety can be alternatively established using a distance equal to the width of the clavicular head of the SCM at its insertion on the clavicle. The palpating index finger is placed at this site as shown in Figure 5. We customarily draw two arrows at this location pointing to each other. The proximal arrow, above the finger, is used to localize the needle entrance point, the distal one shows the direction of the needle path. The needle is inserted immediately cephalad to the palpating finger and advanced first perpendicularly to the skin for 2–5 mm (depending on the amount of the patient’s subcutaneous tissue) and then turned caudally under the palpating finger to advance it in a direction that is parallel to the midline, as shown in Figure 5. The block should take place above the clavicle, under the palpating finger. As a goal we like to elicit an isolated muscle twitch in all fingers either in flexion or extension to confirm needle proximity to the lower trunks of the plexus. Any other response carries a significantly lower success rate. If repositioning of the needle is necessary, the needle is withdrawn and the angle is adjusted in the anteroposterior plane, but always parallel to the midline and never directed medially

FIGURE 3. Landmarks. The lateral insertion of the SCM to the clavicle is shown underneath the palpating finger.

FIGURE 4. Margin of safety. A distance of approximately 1 in. (2.5 cm) is measured laterally from the SCM, to assure the needle placement away from the pleural dome.

FIGURE 5. Point of needle entrance and direction. The point of needle entrance is located just cephalad to the palpating finger and one fingerbreadth above the clavicle. The needle is first introduced perpendicular to the skin and is then turned and advanced parallel to the midline.
Nerve Stimulator Settings
The nerve stimulator is initially set to a current intensity of around 0.8 mA and a pulse width of 100 μs. Once the desired response is obtained (i.e., a muscle twitch of the fingers) injection is initiated without reducing the nerve stimulator current. This is a unique characteristic of the supraclavicular block. One study has shown that the onset, duration, and success rate with a supraclavicular block is unaffected by reducing the nerve stimulator to 0.9 mA or less.18 Supraclavicular and lumbar plexus blocks are the only peripheral nerve blocks in which injecting at a higher current than 0.5 mA is recommended.
NYSORA Tips
- The lateral border of the SCM muscle follows a straight line from the mastoid to the clavicle.
- The needle is inserted in a direction that is parallel to the midline.
- Depending on the patient’s weight, the palpating finger needs to exert different amounts of pressure on the deeper tissues. This maneuver helps bring the plexus closer to the skin and makes the trajectory of the needle shorter.
- The needle should never be inserted deeper than 1 in. (2.5 cm) if a twitch from the brachial plexus is not present.
- Because the trunks are contiguous, elicited twitches from one trunk follow the other without interruption. If the twitches instead disappear before reaching the lower trunk, the needle is withdrawn to the point of the previous twitch and advanced with a slight change in the anteroposterior angle of insertion.
- The margin of safety of about 1 in. (2.5 cm) lateral to the insertion of the SCM on the clavicle provides a safe distance lateral to the outer boundary of the pleural dome for the needle to travel. Because of the steep downward direction of the trunks, increasing this distance laterally may prevent the needle from contacting the plexus above the clavicle or miss the short trunks altogether.
- In the supraclavicular block, an initial nerve stimulator current of 0.8 mA is high enough to produce guidance into the plexus, but low enough to assure sufficient proximity for successful block.
- The risk of intraneural injection is minimized by using low injection pressures and meticulous technique.
- The injection is performed slowly with frequent aspirations while carefully observing the patient.
- If pain or abnormal pressure is felt at any point during injection, the needle should be withdrawn 1–2 mm, after which a new assessment is made.
CONTINUOUS TECHNIQUE
Traditionally, the supraclavicular technique has not been considered to be an optimal choice for placement of catheters. The great mobility of the neck at this location carries a risk for catheter dislodgement. Tunneling the catheter to the infraclavicular level could help to make the catheter more stable; however; little data are currently available on this topic.
LOCAL ANESTHETIC CHOICES FOR SINGLE-SHOT AND CATHETER TECHNIQUES
Most of upper extremity surgeries performed under regional anesthesia last 1–3 hours. Consequently, we most commonly use 30 mL of 1.5% mepivacaine with 1:200,000 epinephrine, which provides about 3–4 hours of anesthesia. The same anesthetic solution without epinephrine provides about 2–3 hours of anesthesia. To speed block onset, 2 mL of 8.4% sodium bicarbonate may be added to every 20 mL of mepivacaine solution. Solutions of levobupivacaine, ropivacaine, or bupivacaine provide longer acting anesthesia (5–7 hours) when required. Recent studies have suggested that the use of ultrasound guidance may reduce the volume needed for a successful block. For continuous techniques, a bolus dose of about 10–15 mL of local anesthetic solution can be given, followed by an infusion rate of 8–10 mL/h. A solution of 0.2% ropivacaine can be used for this purpose. A patient-controlled bolus of 3–5 Ll every 30–60 minutes can be added, with the basal infusion decreased to around 5 mL/h. Breakthrough pain must be treated with a bolus of local anesthetic because simply increasing the rate of infusion could take several hours to have an effect.
PERIOPERATIVE MANAGEMENT
The patient that receives single-shot blocks can undergo surgery under intravenous sedation titrated to the patient’s comfort. The sedation requirements vary from patient to patient and range from small intermittent boluses of midazolam or fentanyl, to a propofol infusion at 25–50 mcg/kg/min, to light general anesthesia.
COMPLICATIONS
Common side effects associated with this technique include phrenic nerve block with diaphragmatic paralysis and sympathetic nerve block with development of Horner syndrome. These are typically self-limiting and do not require intervention. Phrenic nerve block reportedly occurs about 50% of the time, although this may be reduced by the use of ultrasound guidance. Intravascular injection with systemic local anesthetic toxicity and hematoma formation can also occur. To reduce the risk, high level of vigilance is needed due to the risch vascularity of the supraclavicular region. In the case of the supraclavicular block, this can be due to puncture of the subclavian, transverse cervical or dorsal scapular arteries, all of which are located near the plexus at this level. Pneumothorax occurs as often as 6.1%, which was an incidence reported in 1961 that compared 230 consecutive supraclavicular blocks with 246 consecutive axillary blocks. However, the comparison was neither blinded nor randomized, and the study used several different techniques. In contrast, this complication is rare in the modern literature. It is frequently mentioned that the pneumothorax complicating a supraclavicular block has a delayed onset. Although such cases have been published in the literature, most of the pneumothoraces reported have been diagnosed within a few hours of the procedure and before the patient’s discharge. Based on the available literature, the pneumothorax associated with supraclavicular block is uncommon, typically small, and it presents within a few hours following the procedure. In some instances its presentation can be delayed up to 12 hours.
SUMMARY
Supraclavicular block is a reliable, rapid-onset approach to brachial plexus anesthesia. The anatomy of the brachial plexus, with its three trunks confined to a much-reduced surface area, affords a high success rate for achieving anesthesia in the upper extremity below the shoulder. A combination of good anatomic knowledge, simple landmarks, and meticulous technique are paramount for consistent success rate and limiting its potential for complications.
REFERENCES
- Moore D: Supraclavicular approach for block of the brachial plexus. In Moore D (ed): Regional Block. A Handbook for Use in the Clinical Practice of Medicine and Surgery, 4th ed. Thomas, Springfield, IL: 1981, pp 221–242.
- Lanz E, Theiss D, Jankovic D: The extent of block following various techniques of brachial plexus block. Anesth Analg 1983;62:55–58.
- Urmey W: Upper extremity blocks. In Brown D (ed): Regional Anesthesia and Analgesia. Philadelphia, PA: Saunders, 1996; pp 254–278.
- Kulenkampff D, Persky M: Brachial plexus anesthesia. Its indications, technique and dangers. Ann Surg 1928;87:883–891.
- Labat G: Regional Anesthesia. Its Technic and Clinical Application. Philadelphia, PA: Saunders, 1922.
- Patrick J: The technique of brachial plexus block anesthesia. Br J Surg 1940;27:734–739.
- Murphey D: Brachial plexus block anesthesia: an improved technic. Ann Surg 1944;119:935–943.
- Winnie A: Plexus Anesthesia. Perivascular Techniques of Brachial Plexus Block. Philadelphia, PA: Saunders, 1993.
- Accardo N, Adriani J: Brachial plexus block: a simplified technic using the axillary route. South Med J 1949;42:920.
- Burnham P: Regional anesthesia of the great nerves of the upper arm. Anesthesiology 1958;19:281–284.
- De Jong R: Axillary block of the brachial plexus. Anesthesiology 1961;22:215–225.
- Brand L, Papper E: A comparison of supraclavicular and axillary techniques for brachial plexus blocks. Anesthesiology 1961;22:226–229.
- Winnie A, Collins V: The subclavian perivascular technique of brachial plexus anesthesia. Anesthesiology 1964;25:353–363.
- Brown DL, Cahill D, Bridenbaugh D: Supraclavicular nerve block: anatomic analysis of a method to prevent pneumothorax. Anesth Analg 1993;76:530–534.
- Franco C, Vieira Z: 1,001 subclavian perivascular brachial plexus blocks: success with a nerve stimulator. Reg Anesth Pain Med 2000;25:41–46.
- Franco CD: The subclavian perivascular block. Tech Reg Anesth Pain Manage 1999;3:212–216.
- Haleem, Shahla; Siddiqui, Ahsan K.; Mowafi, Hany A. Nerve Stimulator Evoked Motor Response Predicting a Successful Supraclavicular Brachial Plexus Block; More Anesthesia & Analgesia. 110(6):1745-1746, June 2010.
- Franco C, Domashevich V, Voronov G, et al: The supraclavicular block with a nerve stimulator: To decrease or not to decrease, that is the question. Anesth Analg 2004;98:1167–1171.
- Kant A, Gupta PK, Zohar S, et al: Application of the continual reassessment method to dose-finding studies in regional anesthesia: an estimate of the ED95 dose for 0.5% bupivacaine for ultrasound-guided supraclavicular block. Anesthesiology. 2013;119:29–35.
- Neal J, Moore J, Kopacz D, et al: Quantitative analysis of respire tory, motor, and sensory function after supraclavicular block. Anesth Analg 1998;86:1239–1244.
- Renes SH, Spoormans HH, Gielen MJ, et al: Hemidiaphragmatic paresis can be avoided in ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med. 2009;34:595–599
- Murata H, Sakai A, Hadzic A, Sumikawa K.: The presence of transverse cervical and dorsal scapular arteries at three ultrasound probe positions commonly used in supraclavicular brachial plexus block. Anesth Analg. 2012;115:470–473.
- Greengrass R, Steele S, Moretti G, et al: Peripheral nerve blocks. In Raj P (ed): Textbook of Regional Anesthesia. New York, NY: Churchill Livingstone, 2002, pp 325–377
- Neal J, Hebl J, Gerancher J, et al: Brachial plexus anesthesia: Essentials of our current understanding. Reg Anesth Pain Med 2002;27:402–428
- Harley N, Gjessing J: A critical assessment of supraclavicular brachial plexus block. Anesthesia 1969;24:564–570.