Jerry D. Vloka, Tony Tsai, and Admir Hadzic
INTRODUCTION
Lumbar plexus is an advanced regional anesthesia technique, practiced by relatively few, experienced regional anesthesiologists. This is because these techniques have been challenging to master and resulted in frequent failure. Dogliotti pointed out, “the nerve trunks of the lumbar plexus which run into the inferior extremity are at a great distance from each other, so much so that in order to produce anesthesia, multiple procedures are necessary with separate injections, for each nerve trunk.” Hence, anesthesiologists preferred the more time-efficient, simpler and reliable techniques of spinal or epidural anesthesia. Several variations of the original technique have been proposed, the main differences in these various approaches being in the level of block and the distance from the midline for the needle insertion. However, given the deep location of the lumbar plexus, various approaches often represent minuscule technical variations rather than clinically relevant modifications. For instance, Chayen’s approach is thought to result in too high incidence of an epidural block, but another proposed technique also resulted in a 15% incidence of epidural block. Although ultrasound guidance may allow visualization of the lumbar plexus, the ultrasound-guided technique still requires expertise and is technically challenging; Sonography and Considerations for Ultrasound-Guided Lumbar Plexus Block. Regardless of which technique is followed, certain safety precautions must be used for the successful and safe use of this technique.
INDICATIONS
Lumbar plexus block has been used for a number of lower extremity procedures. It has been shown to be particularly useful for femoral shaft and neck fractures, knee procedures, and procedures involving the anterior thigh. However, lumbar plexus block alone cannot provide adequate anesthesia for major surgery of the lower extremity because of the contributing innervation by the sciatic nerve. In one report, even when combined lumbar plexus-sciatic blocks are used for anesthesia in patients undergoing total knee arthroplasty, 22% of patients still required general anesthesia.
REGIONAL ANESTHESIA ANATOMY AND MANAGEMENT
The lumbar plexus consists of five nerves on each side, the first of which emerges between the first and second lumbar vertebrae and the last between the last lumbar vertebra and the base of the sacrum. As the L2, L3, and L4 roots of the lumbar plexus split off their spinal nerves and emerge from the intervertebral foramina, they enter the psoas major muscle (Figure 1). Within the muscle, these roots then split into anterior and posterior divisions, which reunite to form the individual branches (nerves) of the plexus. The major branches of the lumbar plexus are the genitofemoral nerve, lateral femoral cutaneous nerve, femoral nerve, and obturator nerve (Figure 2). Within the psoas major muscle, the lateral femoral cutaneous and femoral nerves are separated from the obturator nerve by a muscular fold in more than 50% of patients; anatomic variations are also common. The femoral nerve is formed by the posterior divisions of L2–L4 and descends from the plexus lateral to the psoas muscle. The anterior divisions of the same roots unite to form the other major branch of the lumbar plexus, the obturator nerve. The reader is referred to Functional Regional Anesthesia for more in-depth discussions of anatomy.
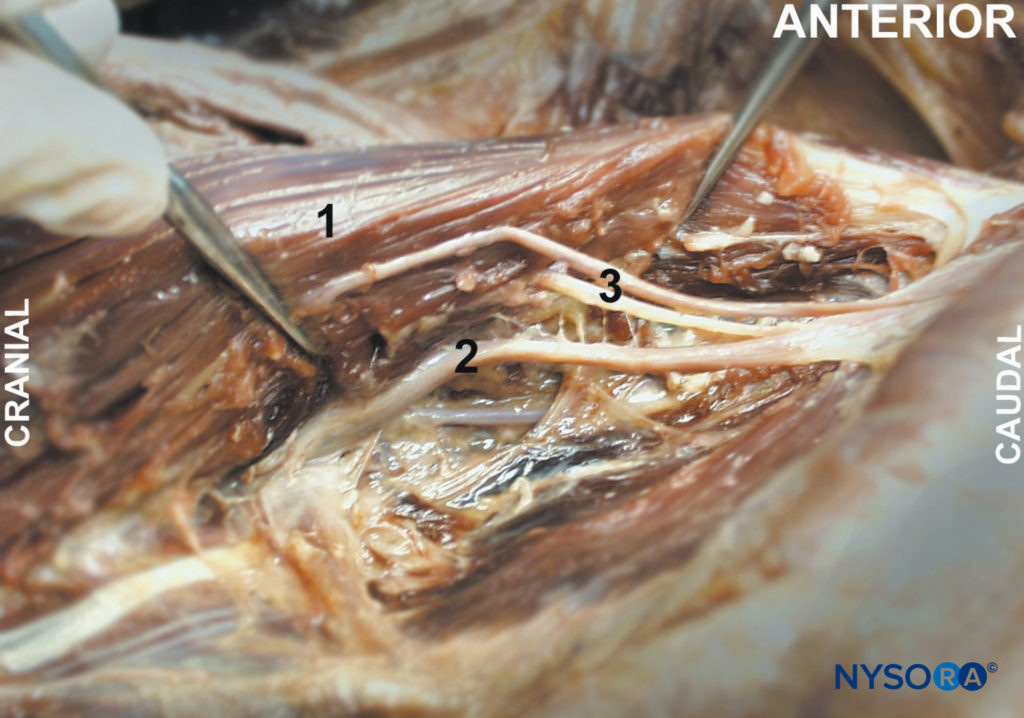
FIGURE 1. Psoas muscle (1) is shown exposed from within the abdominal cavity with lumbar plexus branches (2, 3).
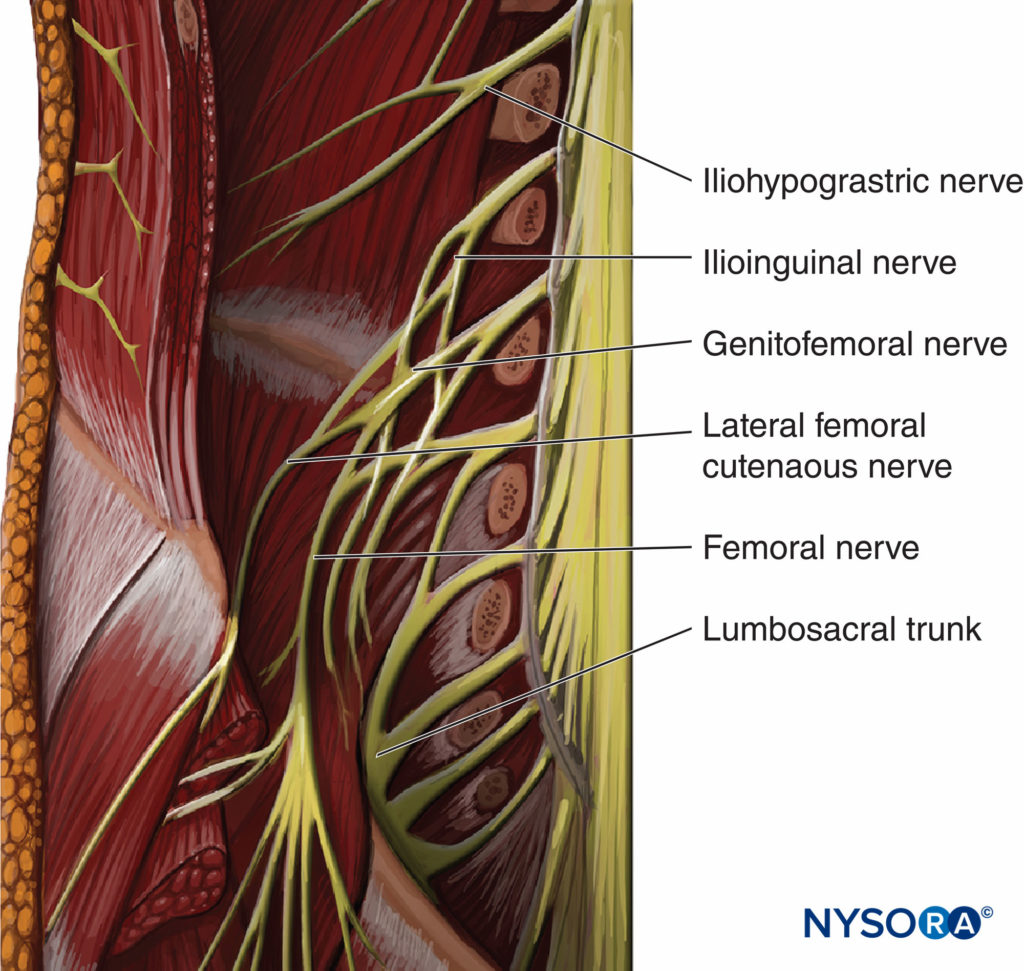
FIGURE 2.Psoas muscle (1) is shown exposed from within the abdominal cavity with lumbar plexus branches (2, 3).
Distribution of Anesthesia
Injection of local anesthetic during lumbar plexus block most commonly results in a spread of the injectate within the body of the psoas muscle around the lumbar branches (L2–L4), with cephalad spread to the lumbar nerve roots.
The femoral nerve supplies motor fibers to the quadriceps muscle (knee extension), the skin of the anteromedial thigh, and the medial aspect of the leg below the knee and foot. The obturator nerve sends motor branches to the adductors of the hip and a highly variable cutaneous area on the medial thigh or knee joint. The lateral femoral cutaneous and genitofemoral nerves are purely cutaneous nerves. Figure 3 illustrates the cutaneous innervation of the lumbar plexus.
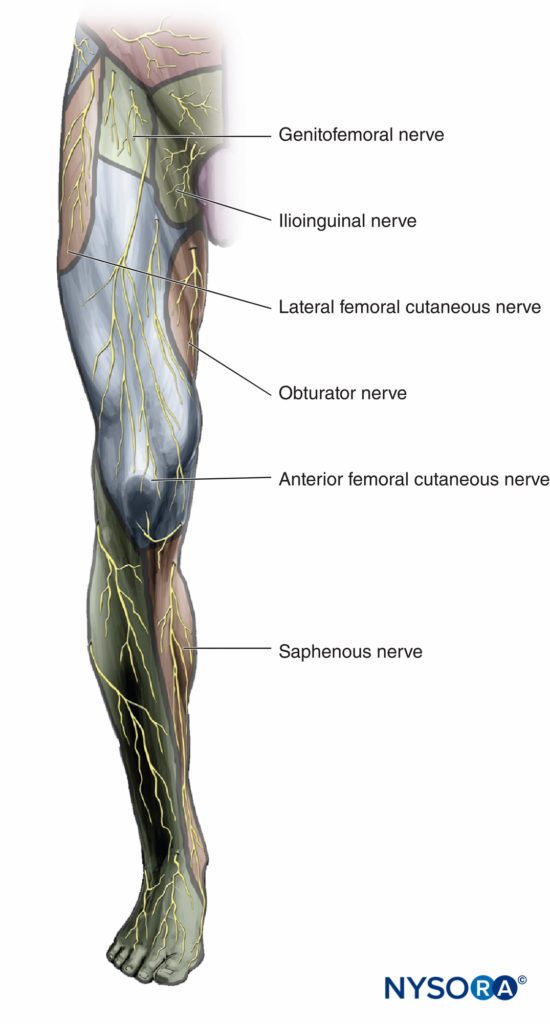
FIGURE 3. Distribution of anesthesia and analgesia after a successful lumbar plexus block.
Choice of Local Anesthetic
Lumbar plexus block requires a relatively large volume of local anesthetic. The choice of the type and concentration of local anesthetic should be based on whether the block is planned for surgical anesthesia or pain management. Because of the vascular nature of the area and the potential for inadvertent intravascular injection, rapid absorption from the deep muscle beds, and epidural spread, then rapid, forceful injections should be avoided. Epinephrine is almost routinely used as a vascular marker. The most commonly used local anesthetic for this block in our institution for short procedures is alkalinized 2-chloroprocaine 3% with 1:300,000 epinephrine in patients having knee arthroscopy. Some common choices of local anesthetics for this block are listed in Table 1.
TABLE 1. Local anesthetic choices for lumbar plexus block.
| Onset (min) | Anesthesia (h) | Analgesia (h) |
|
|---|---|---|---|
| 3% 2-Chloroprocaine (+ HCO3; + epinephrine) | 10–15 | 1.5 | 2.0 |
| 1.5% Mepivacaine (+ HCO3) | 10-15 | 2 | 2-4 |
| 1.5% Mepivacaine (+ HCO3; + epinephrine) | 10-15 | 2.5–3 | 2-5 |
| 2% Lidocaine (+ HCO3) | 10-20 | 2.5–3 | 2-5 |
| 2% Lidocaine (+ HCO3 + epinephrine) | 10-20 | 5–6 | 5-8 |
| 0.5% Ropivacaine | 15-20 | 4-6 | 6-10 |
Technique
The patient is in the lateral decubitus position with a slight forward tilt (Figure 4). The foot on the side to be blocked should be positioned over the dependent leg so that twitches of the quadriceps muscle and/or patella can be seen easily.

FIGURE 4. Patient position for lumbar plexus block.
A standard regional anesthesia tray is prepared with the following equipment:
- Sterile towels and 4-in. × 4-in. gauze packs
- 20-mL syringes with local anesthetic
- Sterile gloves, marking pen, and surface electrode
- One 1.5-in., 25-gauge needle for skin infiltration
- A 10-cm long, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Injection pressure monitor
More information on Equipment for Peripheral Nerve Blocks.
Landmarks for the lumbar plexus block include Figure 5:
1. Midline (spinous processes)
2. Iliac crest
3. Needle insertion labeled 4-cm lateral to the intersection of landmarks 1 and 2
After cleaning with an antiseptic solution, the skin is anesthetized by infiltrating local anesthetic subcutaneously. The fingers of the palpating hand are pressed against the paravertebral muscles to stabilize the landmark and decrease the skin–nerve distance. The needle is inserted at a perpendicular angle to the skin (Figure 6 A and B). The nerve stimulator should be initially set to deliver a current intensity of 1.5 mA. As the needle is advanced, local twitches of the paravertebral muscles are obtained first at a depth of a few centimeters. The needle is then advanced further until twitches of the quadriceps muscle are obtained (usually at the depth of 6–8 cm). After the twitches are obtained, the current should be lowered to obtain stimulation between 0.5 and 1.0 mA. At this point, 25–35 mL of local anesthetic is slowly injected with frequent aspiration to rule out inadvertent intravascular placement of the needle. Of note, while ultrasound guidance allowed for a reduction of the volume and dose of local anesthetics for most nerve block procedures, this is not the case in the lumbar plexus block.
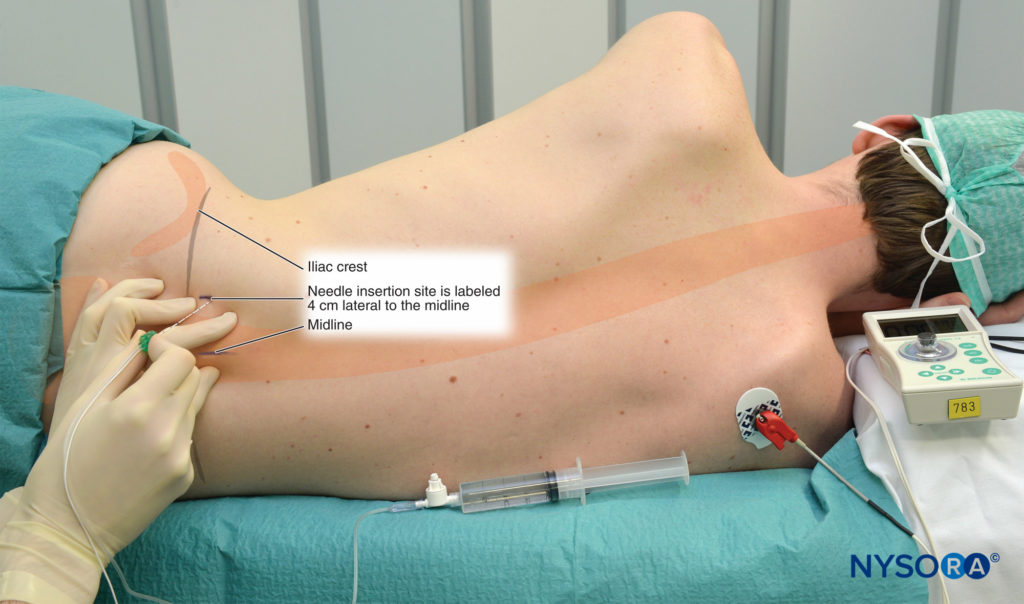
FIGURE 5. Landmarks for lumbar plexus block.
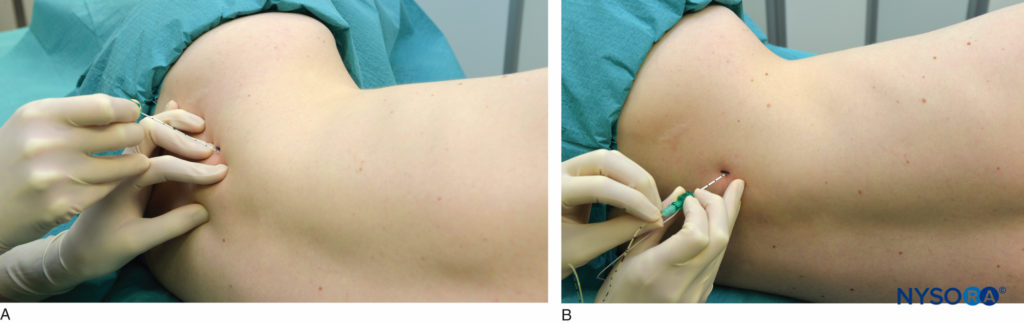
FIGURE 6. A and B. Needle insertion for the lumbar plexus block. The needle is inserted perpendicular to the body plane or with a slight medial orientation (shown) (A). Catheter placement technique is preceded by a similar needle technique (B).
NYSORA Tips
- Successful lumbar plexus block depends on the disposition of the local anesthetic in the fascial plane (psoas muscle) where the roots of the plexus are situated. Nerve stimulation is used to identify this plane by eliciting stimulation of one of the roots.
TABLE 2. Troubleshooting procedures during lumbar plexus blocks.
| Response Obtained | Interpretation | Problem | Action |
|---|---|---|---|
| Local twitch of the paraspinal muscles | Direct stimulation of the paraspinal muscles | Too shallow placement of the needle | Continue advancing the needle |
| Needle contacts bone at 4–6 cm depth; no twitches are seen | The needle advancement is stopped by the transverse process | Indicates proper needle placement, but requires redirection of the needle | Withdraw the needle to the skin level, and redirect 5 degrees cranially or caudally |
| Twitches of hamstrings muscles are seen; needle inserted 6–8 cm | Result of stimulation of the roots of the sciatic plexus (sciatic nerve) | Needle inserted too caudally | Withdraw the needle and reinsert 3–5 cm cranially |
| Flexion of thigh at the depth of > 6–8 cm | This subtle and often missed response is caused by direct stimulation of the psoas muscle | Needle inserted too deep (missed the lumbar plexus roots); further advancement may place the needle intraperitoneally | Stop advancing the needle; withdraw the needle and reinsert using the protocol outlined in the technique description |
| Needle is placed deep (10 cm), but twitches were not elicited and bone is not contacted | Needle missed the transverse process and roots of the lumbar plexus | Needle placement too lateral | Withdraw the needle and reinsert with a slight medial angulation (5–10 degrees) |
- Stimulation at currents less than 0.5 mA should not be sought because stimulation with a low current may indicate the placement of the needle inside a dural sleeve. An injection inside this sheath can result in a spread of the local anesthetic toward the epidural or subarachnoid space.
When insertion of the needle does not result in quadriceps muscle stimulation, the maneuvers outlined in Table 2 should be followed.
Block Dynamics and Perioperative Management
A lumbar plexus block is uncomfortable for patients owing to the needle passage through multiple muscle planes and adequate premedication is necessary. Typically, we use midazolam 2-4 mg after the patient is positioned and alfentanil 500–750 mcg just before needle insertion. Typical onset time for this block is 15–25 minutes, depending on the type, concentration, and volume of local anesthetic and the level at which the needle is placed. For example, although an almost immediate onset of anesthesia in the anterior thigh and knee can be achieved with an injection at the L3 level, additional time is required for the local anesthetic to block the lateral thigh (L1) or obturator nerve (L5). The first sign of the onset of a block is usually the loss of sensation in the saphenous nerve territory (medial skin below the knee).
CONTINUOUS LUMBAR PLEXUS BLOCK
Continuous lumbar plexus block is an advanced regional anesthesia technique, and adequate experience with the single-shot technique is a prerequisite to ensure its efficacy and safety. Otherwise, the technique is similar to the single-shot injection except that the Tuohy-style tip needle is preferable. The needle opening should be directed cephalad to facilitate threading of the catheter. This technique can be used for postoperative pain management in patients undergoing hip, femur, and knee surgery. However, because a large volume of local anesthetic is required to accomplish analgesia, continuous infusion requires intermittent boluses for success. Consequently, some feel that its advantages over the femoral block for postoperative analgesia are questionable at best and that continuous lumbar plexus block should not be in routine use for postoperative analgesia. More information on Continuous Peripheral Nerve Blocks: Local Anesthetic Solutions and Infusion Strategies.
Equipment
A standard regional anesthesia tray is prepared with the following equipment:
- Sterile towels and 4-in. × 4-in. gauze packs
- 20-mL syringe with local anesthetic
- Sterile gloves, marking pen, and surface electrode
- One 1.5-in. 25-gauge needle for skin infiltration
- A 10-cm long, insulated stimulating needle (preferably Tuohy-style tip)
- Catheter
- Peripheral nerve stimulator
Learn more about Equipment for Continuous Peripheral Nerve Blocks.
Technique
The skin and subcutaneous tissues are anesthetized with local anesthetic. The needle is attached to the nerve stimulator (1.5 mA, 2 Hz, 100 μsec) and to a syringe with the local anesthetic. The palpating hand should be firmly pressed and anchored against the paraspinal muscles to facilitate the needle insertion and redirection of the needle when necessary. A 10-cm, Tuohy-style tip, continuous block needle is inserted at a perpendicular angle and advanced until the quadriceps twitch response is obtained at 0.5–1.0 mA current. At this point, the initial volume of local anesthetic is injected (e.g., 15–25 mL), and the catheter is inserted approximately 8–10 cm beyond the needle tip. The needle is then withdrawn back to the skin level, while the catheter is simultaneously advanced. This method prevents inadvertent removal of the catheter and intravascular and intrathecal placement by negative aspiration test.
NYSORA Tips
- The skin in the lumbar area can be mobile; thus insertion of the catheter to a depth of 5–6 cm is necessary to help prevent its removal during patient repositioning.
Continuous Infusion
Continuous infusion is initiated after an initial bolus of dilute local anesthetic through the catheter. For this purpose, we routinely use ropivacaine 0.2% (15–20 mL). The infusion is maintained at 10 mL/h or 5 mL/h when a patient-controlled analgesia (PCA) dose is planned (5 mL/q60min). Figures 7 and 8 show the dispersion of 20 mL of a contrast solution within the psoas sheath.
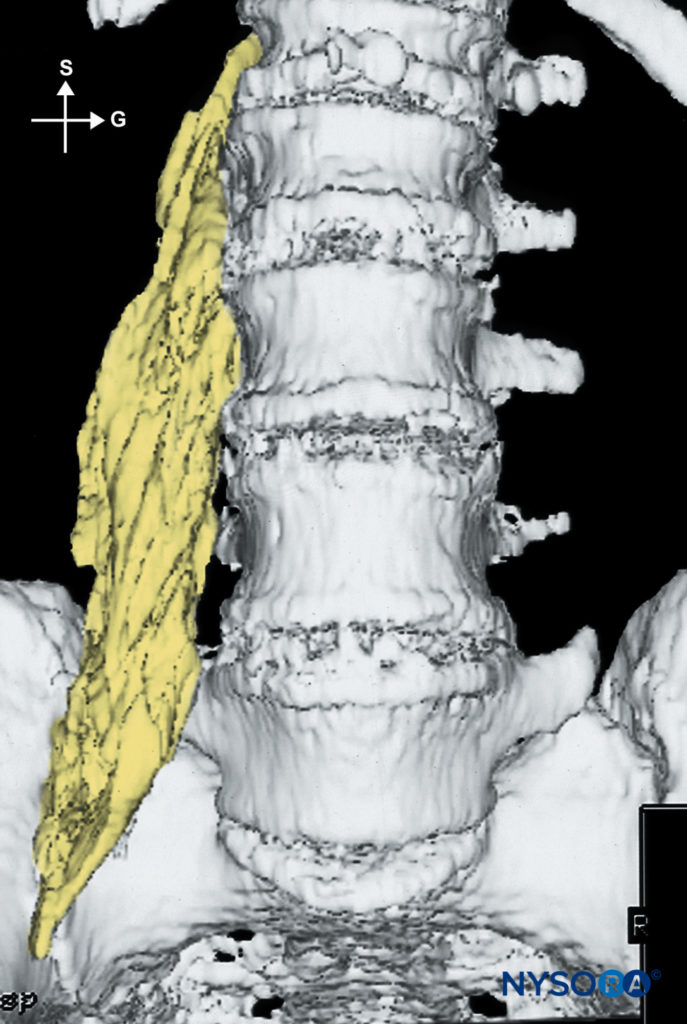
FIGURE 7. Distribution of 20 mL of injectate after lumbar plexus block. A typical fusiform distribution within the psoas muscle is seen.
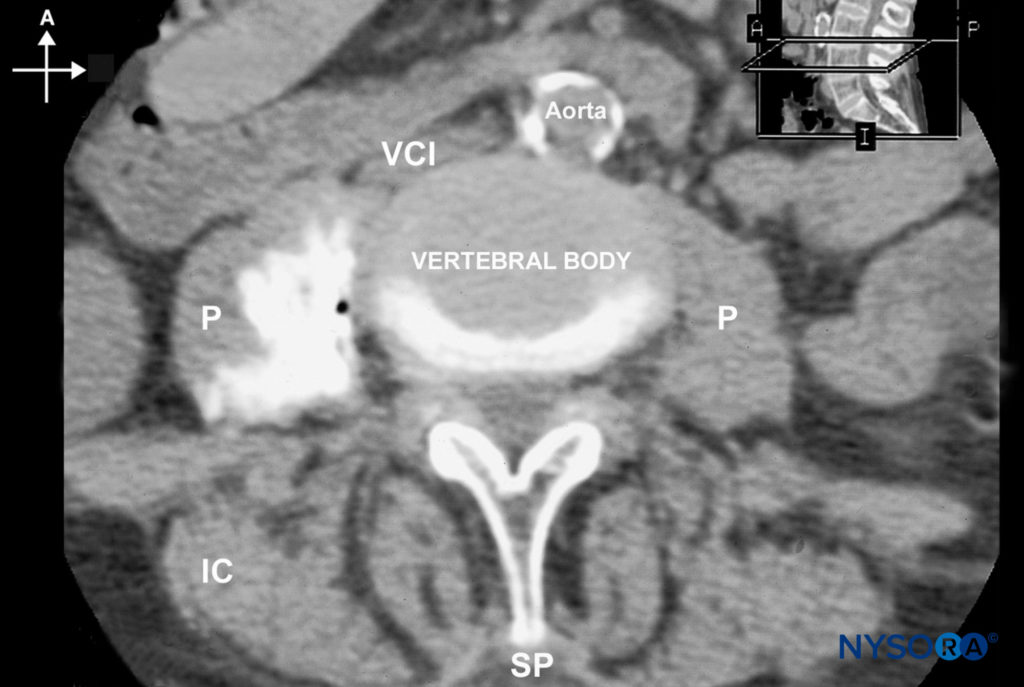
FIGURE 8. An MRI image demonstrating the distribution of local anesthetic after lumbar plexus block. (A, anterior; I, inferior; IC, iliac crest; P, psoas muscle; SP, spinous process; VCI, vena cava inferior.)
COMPLICATIONS AND HOW TO AVOID THEM
The lumbar plexus block is an advanced technique with a potential for serious complications. The most common complications reported with lumbar plexus block are epidural spread with a risk of high neuraxial anesthesia, hypotension, local anesthetic toxicity, spinal anesthesia or iliopsoas or renal hematoma. Although the plasma concentrations of local anesthetics are not significantly higher after lumbar plexus block compared with other peripheral nerve blocks, there is the potential for rapid absorption and intravascular channeling owing to the large volumes required for this block and intramuscular location of the needle. In addition, this block is best avoided in anticoagulated patients due to the risk of haematoma. Table 3 provides some general and specific instructions on possible complications and methods to avoid.
TABLE 3. Strategies to decrease the risk of complications.
| Complication | Instruction |
|---|---|
| Infection | • A strict aseptic technique is used |
| Hematoma | • Avoid multiple needle insertions, particularly in anticoagulated patients • Avoid continuous lumbar plexus blocks in anticoagulated patients • Antiplatelet therapy is not a contraindication for lumbar plexus block in the absence of spontaneous bleeding |
| Vascular puncture | • Deep needle insertion should be avoided (vena cava, aorta) |
| Local anesthetic toxicity | • Large volumes of long-acting anesthetic should be reconsidered in older and frail patients • Careful and frequent aspiration should be performed during the injection • Avoid forceful, fast injection of local anesthetic |
| Nerve injury | • Risk after lumbar plexus block is low • Local anesthetic should never be injected when the patient complains of pain or when abnormally high pressure on injection is noted • When stimulation is obtained with current intensity of <0.5 mA, the needle should be pulled back to obtain the same response with a current of 0.5 mA before injecting local anesthetic to avoid injection into the dural sleeves and the consequent epidural or spinal spread |
| Hemodynamic consequences | • Lumbar plexus block results in unilateral sympathectomy • Spread of the local anesthetic to the epidural space may result in significant hypotension and occurs in up to 15% of patients • Patients receiving a lumbar plexus block should be monitored to the same extent as patients receiving epidural anesthesia |
REFERENCES
- de Takats G: Local Anesthesia. Philadelphia, PA: Saunders, 1928.
- Labat G: Regional Anesthesia. In Its technic and Clinical Application, 2nd ed. Philadelphia, PA: Saunders, 1924.
- Sherwood-Dunn B: Regional Anesthesia. Philadelphia, PA: Davis, 1920.
- Dogliotti A: Narcosis—Local-Regional-Spinal. Chicago, IL: Debour, 1939.
- Mannion S, O’Callaghan S, Walsh M, et al: In with the new, out with the old? Comparison of two approaches for psoas compartment block. Anesth Analg 2005;101:259–264.
- Awad IT, Duggan EM: Posterior lumbar plexus block: anatomy, approaches, and techniques. Reg Anesth Pain Med 2005;30:143–149.
- Chayen D, Nathan H, Chayen M: The psoas compartment block. Anesthesiology 1976;45:95–99.
- Molina Monleon I, Asensio Romero I, Barrio Mataix J, et al: [Epidural anesthesia after posterior lumbar plexus block.] Rev Esp Anestesiol Reanim 2005;52:55–56.
- Kirchmair L, Entner T, Wissel J, et al: A study of the paravertebral
anatomy for ultrasound guided posterior lumbar plexus block. Anesth Analg 2001;93:477–478. - Sauter AR, Ullensvang K, Niemi G, et al: The Shamrock lumbar plexus block: A dose finding study. Eur J Anaesthesiol 2015; 32:764–770.
- Karmakar MK, Li JW, Kwok WH, et al: Sonoanatomy relevant for lumbar plexus block in volunteers correlated with cross-sectional anatomic and magnetic resonance images. Reg Anesth Pain Med 2013;391–397.
- Capdevilla X, Macaire P, Dadure C, et al: Continuous psoas compartment blocks for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines, and clinical evaluation. Anesth Analg 2002;94:1606–1613.
- Indelli PF, Grant SA, Nielsen K, et al: Regional anesthesia in hip surgery. Clin Orthop Relat Res 2005;441:250–205.
- Watson MW, Mitra D, McLintock TC, Grant SA: Continuous versus single-injection lumbar plexus blocks: comparison of the effects on morphine use and early recovery after total knee arthroplasty. Reg Anesth Pain Med 2005;30:541–547.
- Luber MJ, Greengrass R, Vail TP: Patient satisfaction and effectiveness of lumbar plexus and sciatic nerve block for total knee arthroplasty. J Arthroplasty 2001;16:17–21.
- Di Benedetto P, Pinto G, Arcioni R, De Blasi RA, et al: Anatomy and imaging of lumbar plexus. Minerva Anestesiol 2005;71:549–554.
- Sim IW, Webb T: Anatomy and anaesthesia of the lumbar somatic plexus. Anaesth Intensive Care 2004;32:178–187.
- Farny J, Drolet P, Girard M: Anatomy of the posterior approach to the lumbar plexus block. Can J Anaesth 1994;41:480–485.
- Mannion S, Barrett J, Kelly D, et al: A description of the spread of injectate after psoas compartment block using magnetic resonance imaging. Reg Anesth Pain Med 2005;30:567–571.
- Gadsden JC, Lindenmuth DM, Hadzic A, et al: Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology 2008;683–688.
- Khy V, Girard M: [The use of 2-chloroprocaine for a combined lumbar plexus and sciatic nerve block.] Can J Anaesth 1994;41:919–924.
- Hadzic A, Karaca PE, Hobeika P, et al: Peripheral nerve blocks result in superior recovery profile compared with general anesthesia in outpatient knee arthroscopy. Anesth Analg 2005;100:976–981.
- Chelly JE, Casati A, Al-Samsam T, et al: Continuous lumbar plexus block for acute postoperative pain management after open reduction and internal fixation of acetabular fractures. J Orthop Trauma 2003;17:362–367.
- Bogoch ER, Henke M, Mackenzie T, et al: Lumbar paravertebral nerve block in the management of pain after total hip and knee arthroplasty: a randomized controlled clinical trial. J Arthroplasty 2002;17:398–401.
- Litz RJ, Vicent O, Wiessner D, Heller AR: Misplacement of a psoas compartment catheter in the subarachnoid space. Reg Anesth Pain Med 2004;29:60–64.
- Auroy Y, Benhamou D, Bargues L, et al: Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology 2002;97:1274–1280.
- Gentili M, Aveline C, Bonnet F: [Total spinal anesthesia after posterior lumbar plexus block.] Ann Fr Anesth Reanim 1998;17:740–742.
- Farny J, Girard M, Drolet P: Posterior approach to the lumbar plexus combined with a sciatic nerve block using lidocaine. Can J Anaesth 1994;41:486–491.
- Huet O, Eyrolle LJ, Mazoit JX, Ozier YM: Cardiac arrest after injection of ropivacaine for posterior lumbar plexus block. Anesthesiology 2003;99:1451–1453.
- Mullanu CH, Gaillat F, Scemama F, et al: Acute toxicity of local anesthetic ropivacaine and mepivacaine during a combined lumbar plexus and sciatic block for hip surgery. Acta Anaesthesiol Belg 2002;53: 221–223.
- Pham-Dang C, Beaumont S, Floch H, et al: [Acute toxic accident following lumbar plexus block with bupivacaine.] Ann Fr Anesth Reanim 2000;19:356–359.
- Capdevila X, Coimbra C, Choquet O: Approaches to the lumbar plexus: success, risks, and outcome. Reg Anesth Pain Med. 2005; 150–162.
- Hsu DT: Delayed retroperitoneal haematoma after failed lumbar plexus block. Br J Anaesth 2005;394–395.
- Aveline C, Bonnet F: Delayed retroperitoneal haematoma after failed lumbar plexus block. Br J Anaesth 2004;93:589–591.
- Klein SM, D’Ercole F, Greengrass RA, Warner DS: Enoxaparin associated with psoas hematoma and lumbar plexopathy after lumbar plexus block. Anesthesiology 1997;87:1576–1579.
- Aida S, Takahashi H, Shimoji K: Renal subcapsular hematoma after lumbar plexus block. Anesthesiology 1996;84:452–455.
- Blumenthal S, Ekatodramis G, Borgeat A: Ropivacaine plasma concentrations are similar during continuous lumbar plexus block using two techniques: Pharmacokinetics or pharmacodynamics? Can J Anaesth 2004;51–851.