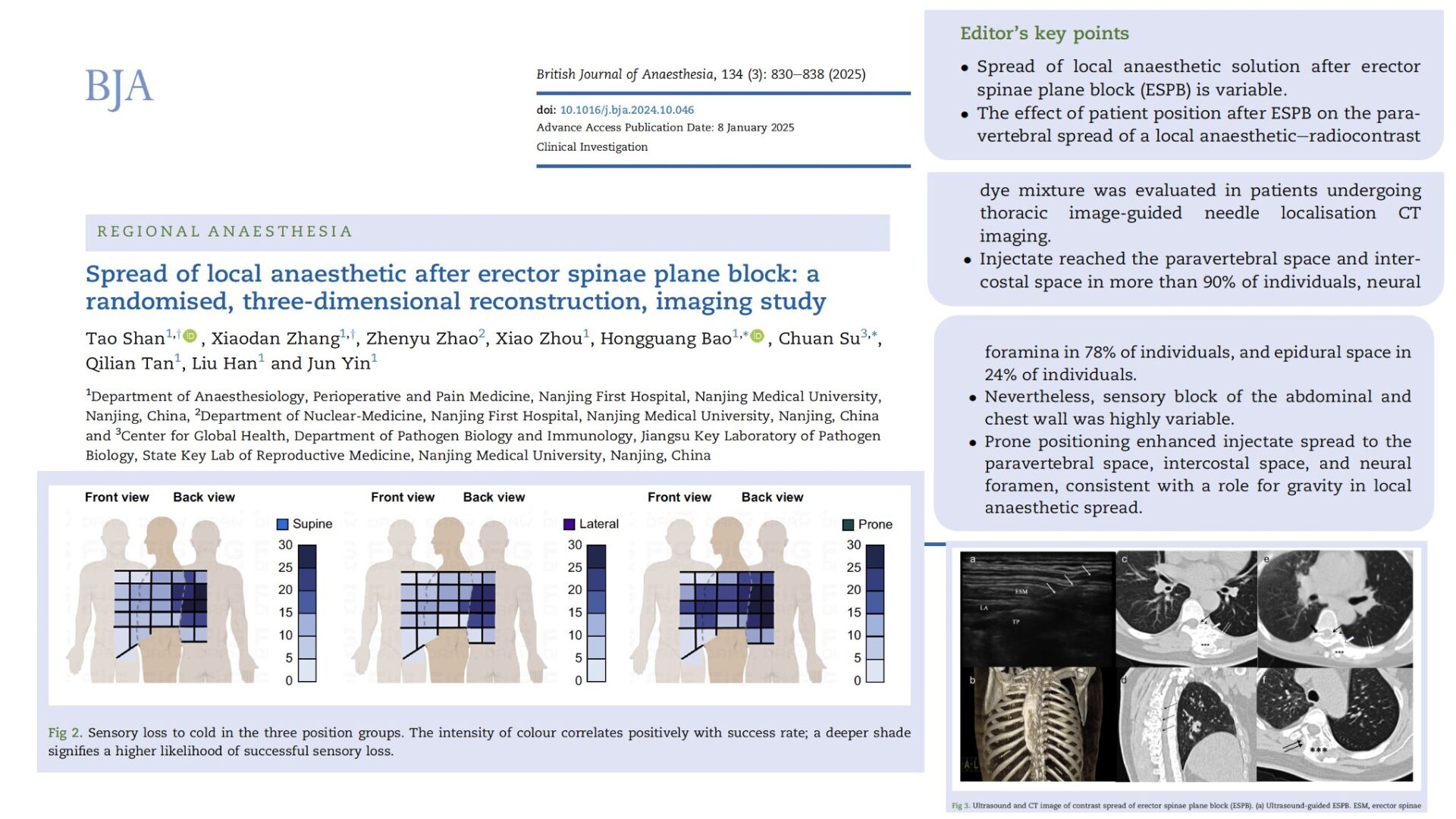
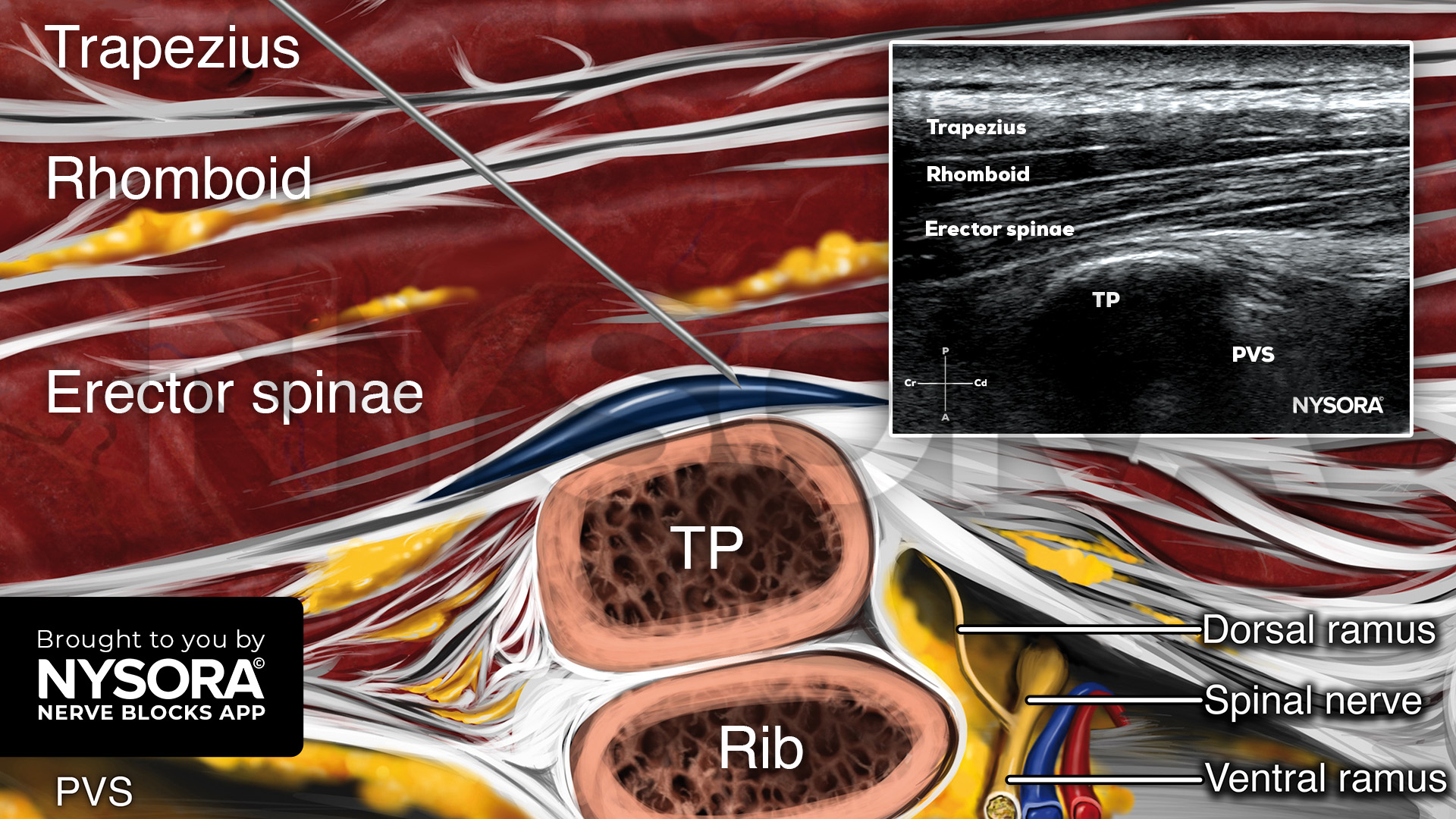
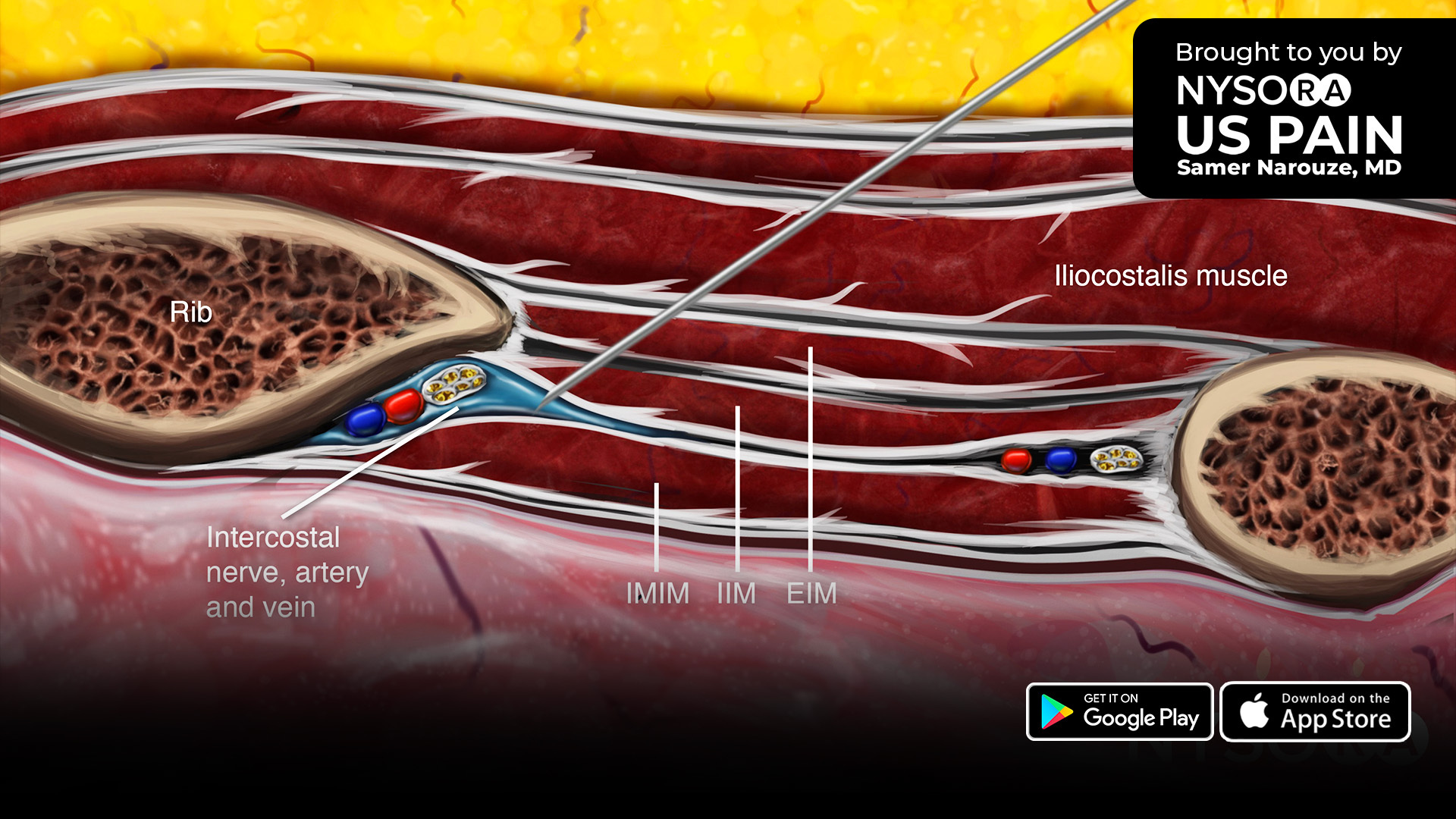
The erector spinae plane block (ESPB) has gained significant attention as a regional anesthesia technique since its introduction in 2016. Initially described as an alternative to thoracic epidural and paravertebral blocks, ESPB offers a relatively simple, ultrasound-guided approach with a favorable safety profile. It is now frequently used in thoracic and abdominal surgeries to manage postoperative pain while minimizing systemic opioid use.
Despite its growing popularity, ESPB has shown variable results in clinical practice. The inconsistency in its analgesic efficacy is often attributed to the unpredictable spread of local anesthetic. In particular, it remains unclear how reliably the anesthetic reaches the paravertebral space, which is believed to be a crucial site for achieving effective multi-dermatomal analgesia.
One possible factor influencing local anesthetic spread is patient positioning after the block is performed. Gravity could play a role in directing the flow of the local anesthetic, especially given the large volumes often used for ESPB. However, to date, few studies have explored this variable in a controlled clinical setting.
This study aimed to determine whether maintaining different patient positions after ESPB affects the local anesthetic spread to key anatomical spaces, including the paravertebral, intercostal, and epidural spaces.
Study objective and methods
The primary goal of this study was to assess the influence of patient position on the local anesthetic spread after ESPB.
- Design: Single-center, prospective, randomized trial.
- Participants: 84 patients undergoing ESPB for CT-guided percutaneous pulmonary nodule localization were enrolled.
- Randomization: Patients were assigned to one of three post-ESPB positions: Supine, lateral (operation side up), or prone group.
- Procedure: ESPB was performed at the T7 level using ultrasound guidance. A mixture of 0.375% ropivacaine (15 mL) and radiocontrast dye (15 mL) was injected for a total volume of 30 mL. Patients maintained their assigned position for 30 minutes before undergoing CT imaging.
- Primary outcome: The proportion of patients with local anesthetic spread to the paravertebral space.
Secondary outcomes: Spread to neural foramina, epidural space, and intercostal space, craniocaudal spread (measured in thoracic vertebral levels), sensory block distribution assessed with cold testing.
Key findings
- Paravertebral space spread: The local anesthetic reached the paravertebral space in 96.5% of all cases. Spread was observed in 100% of prone-positioned patients, compared to 93.1% in supine and 96.3% in lateral positioning.
- Neural foramina and epidural spread: Spread to the neural foramina occurred in 77.9% of patients. The prone position significantly increased spread to the neural foramina (90% vs. 70% in supine, P = 0.005). Epidural spread was noted in 24% of patients, with higher incidence in prone positioning (36.7%) compared to supine (13.8%).
- Intercostal space and craniocaudal spread: Intercostal spread occurred in 94.2% of patients, with the highest distribution in the prone group (100% vs. 96.6% in supine, 85.2% in lateral, P < 0.001). The prone position allowed the local anesthetic to spread across 4.3 thoracic levels, compared to 3.2 in supine (P = 0.019).
- Sensory block variability: Despite widespread local anesthetic spread, sensory block in the ventral dermatomes was highly inconsistent, highlighting the unpredictable nature of ESPB’s clinical effects.
Conclusion
This study demonstrates that patient positioning significantly influences local anesthetic spread after ESPB. The prone position resulted in the greatest spread to the paravertebral space, intercostal space, and neural foramina. These findings suggest that gravity plays a role in directing anesthetic distribution, potentially enhancing ESPB’s effectiveness. However, despite increased anesthetic spread, sensory block patterns remained highly variable, raising questions about ESPB’s clinical reliability.
Future research
Further studies should focus on correlating anesthetic spread with clinical analgesic outcomes to determine whether prone positioning leads to improved pain control. Investigating the optimal injection volume and speed may also refine ESPB’s effectiveness. Future research should explore the long-term impact of different post-ESPB positions and whether positioning strategies can improve pain relief consistency.
For more detailed information, refer to the full article in BJA.
Shan T et al. Spread of local anaesthetic after erector spinae plane block: a randomised, three-dimensional reconstruction, imaging study. Br J Anaesth. 2025;134:830-838.
Download the Nerve Blocks App HERE for in-depth insights on the erector spinae plane block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Blocks Manual Course on NYSORA’s LMS!