As populations age, the demand for neuraxial procedures in older adults continues to rise. Yet, the anatomical changes that occur with aging present unique challenges for clinicians performing these procedures. A recent study by Hagenaars et al. (2024) sheds light on the evolving morphology of the spine across age groups and its impact on the feasibility of midline neuraxial punctures.
Key findings
The research utilized mid-sagittal computed tomography (CT) scans to evaluate changes in the interspinous space and their effect on the success of virtual needle trajectories. Here are the major takeaways:
- Decreased maneuver space with age:
- The Spinal Accessibility Index (SAI), a measure of available needle maneuver space, significantly decreases with age.
- Older adults (≥80 years) displayed notably smaller and more irregular interspinous spaces compared to younger individuals (21–30 years).
- Optimal puncture points and angles:
- Despite age-related changes, the optimal generic puncture points and angles for neuraxial procedures remained consistent across age groups.
- This indicates that similar techniques may be applied, though anatomical variability should be considered.
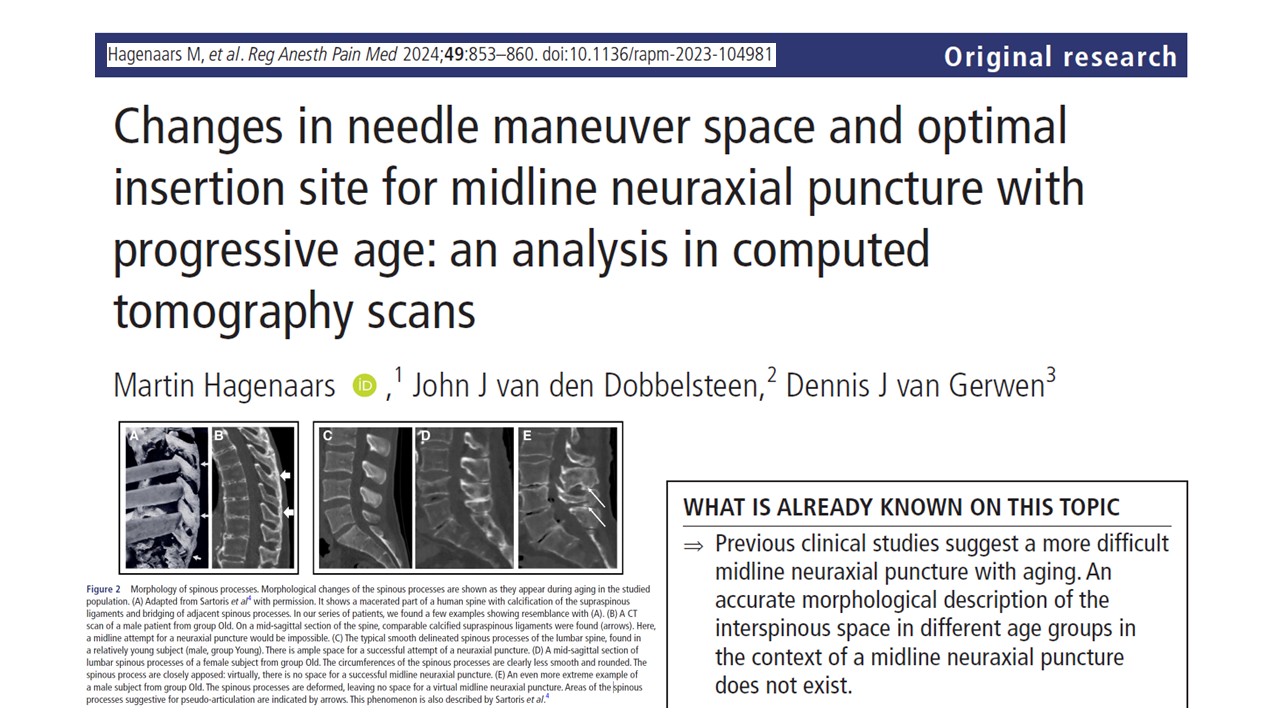
- Morphological changes:
- In older adults, calcification of ligaments, ossification, and pseudo-articulation formations were common.
- These changes can render certain interspaces inaccessible via midline approaches, particularly in the lumbar region.
Implications for clinical practice
- Challenges for older adults:
- Reduced SAI highlights the need for precise technique, particularly in patients over 80.
- The lumbar spine, carrying more weight and exposed to mechanical stress, shows the most significant anatomical deterioration.
- Need for adaptations:
- Alternative approaches like the paramedian technique may be preferable for challenging cases.
- Pre-procedural ultrasound guidance could enhance accuracy, especially in patients with distorted spinal anatomy.
- Training and awareness:
- Detailed anatomical knowledge is essential, particularly for novice practitioners.
- Understanding the expected changes in interspinous space morphology can aid in anticipating difficulties and improving success rates.
Future research
The study underscores the importance of tailored approaches to neuraxial procedures, especially in older populations. To advance clinical outcomes:
- Explore the efficacy of paramedian approaches or combined techniques for aged patients.
- Investigate the role of ultrasound-assisted techniques in reducing failure rates and complications.
- Conduct further research on intermediate age groups (60–80 years), often underrepresented in existing studies.
Conclusion
Hagenaars et al.’s findings provide valuable insights into the anatomical transformations of the spine with aging and their implications for neuraxial punctures. While the optimal techniques remain largely consistent, clinicians must adapt their approaches to navigate the challenges posed by these changes. Enhanced training and the integration of advanced imaging technologies hold promise for improving procedural outcomes, particularly in older adults.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Hagenaars M, van den Dobbelsteen JJ, van Gerwen DJ. Changes in needle maneuver space and optimal insertion site for midline neuraxial puncture with progressive age: an analysis in computed tomography scans. Reg Anesth Pain Med. 2024 Dec 2;49(12):853-860.
Learn more about spinal anesthesia with the Regional Anesthesia Manual e-Course on the NYSORA LMS website!