Diabetes mellitus, particularly type 2 diabetes (T2DM), presents a complex challenge in perioperative and critical care settings. With a growing number of patients on non-insulin diabetes medications, it is crucial that anesthetists, intensivists, and perioperative teams understand how these agents work and how they should be managed during surgical interventions.
This news post offers a comprehensive summary of the British Journal of Anaesthesia 2025 review by Tinsley et al., focusing on the pharmacology and perioperative management of non-insulin diabetes medicines.
Why non-insulin diabetes drugs matter perioperatively
- T2DM affects up to 25% of surgical patients, with even higher prevalence in cardiac surgery.
- Non-insulin agents are often preferred due to lower hypoglycemia risks and easier administration.
- These medicines act via diverse mechanisms, including insulin secretion, gut glucose absorption, insulin sensitivity, and renal glucose handling.
- Optimising perioperative management reduces complications, hospital stays, and surgical delays.
Common classes of non-insulin diabetes medications
1. Sulfonylureas (e.g., gliclazide, glipizide)
- Mechanism: Stimulate pancreatic beta-cells to secrete insulin.
- Risks: High risk of hypoglycemia, especially when fasting.
- Perioperative plan:
- Omit on the day of surgery.
- Restart only once normal eating resumes.
2. Meglitinides (e.g., repaglinide)
- Mechanism: Similar to sulfonylureas but shorter acting.
- Risks: Hypoglycemia, especially during fasting.
- Perioperative plan:
- Omit morning dose for early surgeries.
- Can continue if eating before afternoon surgery.
3. Biguanides (e.g., metformin)
- Mechanism: Reduces hepatic glucose production and increases insulin sensitivity.
- Risks: Potential (though rare) for lactic acidosis, particularly with renal dysfunction.
- Perioperative plan:
- Withhold on surgery day; restart after 48 hours if renal function is normal.
- May continue pre-bariatric surgery with monitoring.
4. Alpha-glucosidase inhibitors (e.g., acarbose)
- Mechanism: Delays intestinal carbohydrate absorption.
- Risks: Minimal; GI side effects like diarrhea, flatulence.
- Perioperative plan:
- Withhold if not eating.
- Restart once normal diet resumes.
5. Thiazolidinediones (e.g., pioglitazone)
- Mechanism: Improve insulin sensitivity via PPAR-γ activation.
- Risks: Fluid retention, potential heart failure.
- Perioperative plan:
- Generally safe to continue.
- Monitor closely in patients at risk for heart failure.
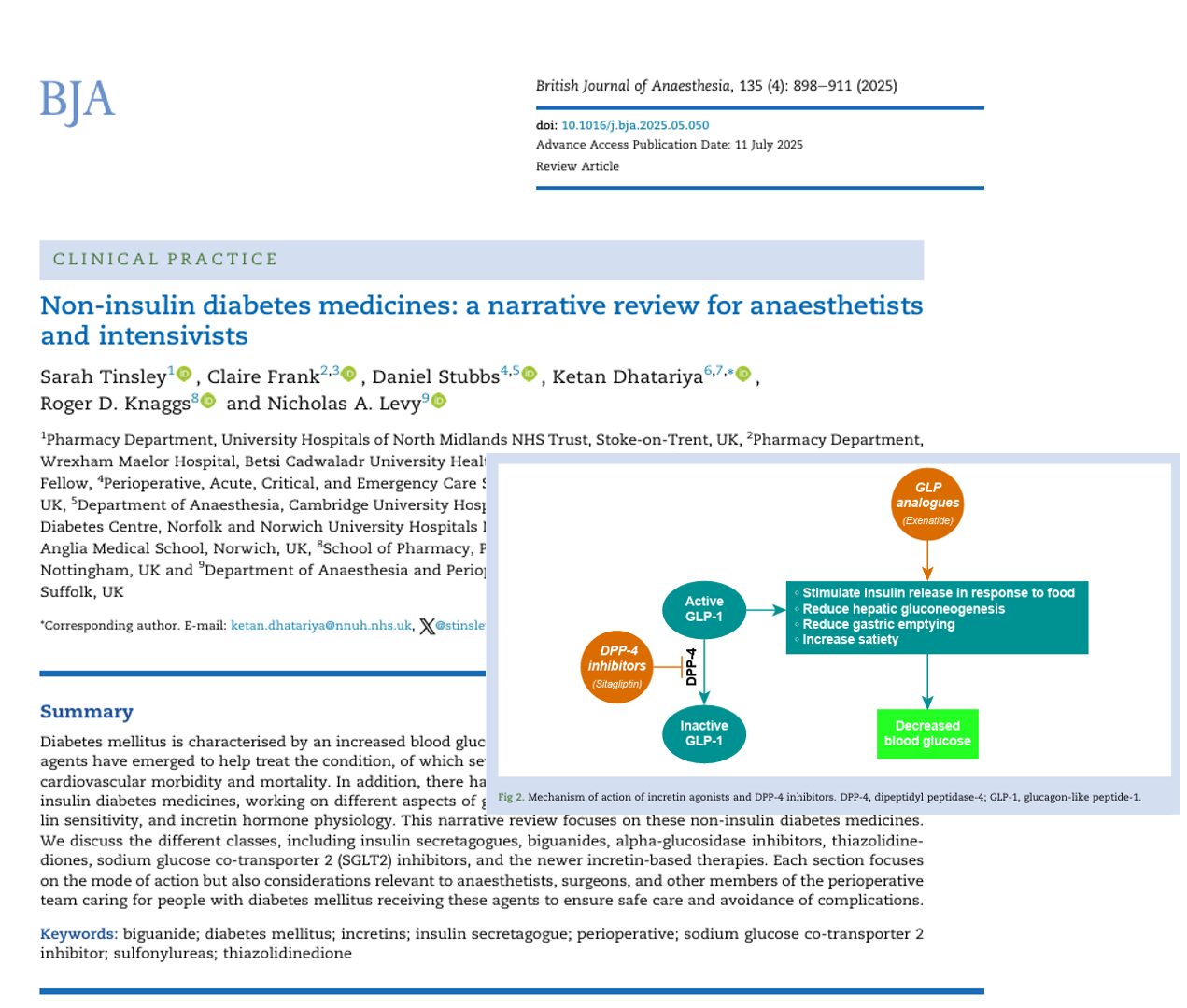
6. DPP-4 inhibitors (e.g., sitagliptin, linagliptin)
- Mechanism: Prolong the action of endogenous incretins.
- Risks: Minimal; rare pancreatitis.
- Perioperative plan:
- Safe to continue, unless in combination with metformin or SGLT2i.
- Restart postoperatively when oral intake resumes.
7. GLP-1 receptor agonists (e.g., semaglutide, liraglutide)
- Mechanism: Enhance insulin secretion, delay gastric emptying.
- Risks: Risk of aspiration from delayed gastric emptying.
- Perioperative plan:
- Individual risk assessment recommended.
- Avoid discontinuation if not necessary.
8. SGLT-2 inhibitors (e.g., dapagliflozin, empagliflozin)
- Mechanism: Promote renal glucose excretion.
- Risks: Euglycemic diabetic ketoacidosis (DKA), especially during fasting or illness.
- Perioperative plan:
- Withhold at least 48 hours before surgery.
- Resume only when eating normally and ketones are normal.
Steps for perioperative management
1. Preoperative assessment
- Identify all diabetes medications and comorbidities.
- Evaluate renal and hepatic function.
- Determine surgical fasting requirements.
2. Medication adjustment
- Refer to drug-specific guidance.
- Withhold agents with high hypoglycemia or DKA risk.
3. Monitoring and support
- Monitor blood glucose and ketones perioperatively.
- Use VRIII or sliding-scale insulin when necessary.
4. Postoperative reintroduction
- Restart oral agents once eating resumes and renal function is stable.
- Individualise therapy based on postoperative glucose levels.
Conclusion
With increasing global use of complex non-insulin therapies for T2DM, perioperative teams must navigate the challenges of balancing glycemic control with medication safety. Each drug class carries unique risks and benefits, and perioperative decisions must be based on patient-specific factors, surgery type, and current evidence. This updated review arms clinicians with the necessary knowledge to make informed decisions that support safe, effective care in both elective and emergency settings.
Reference: Tinsley S et al. Non-insulin diabetes medicines: a narrative review for anaesthetists and intensivists. Br J Anaesth. 2025;135:898-911.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!