General anesthesia is a cornerstone of modern surgery, ensuring patients undergo procedures without pain or awareness. However, accurately measuring the depth of anesthesia remains a significant challenge. A 2024 review by Jiang et al. in Anesthesiology explores the complexities of consciousness under anesthesia, current assessment methods, and potential future advancements.
Why is measuring anesthetic depth so difficult?
- Consciousness is subjective: It involves first-person experiences, while science relies on objective, third-person observations.
- No standard monitor: Unlike heart rate or blood pressure, there is no universally accepted tool to measure consciousness during surgery.
- Risks of mismanagement:
- Too-light anesthesia: Risk of intraoperative awareness, causing psychological trauma.
- Too-deep anesthesia: Potential harm, especially for high-risk populations, though evidence is still debated.
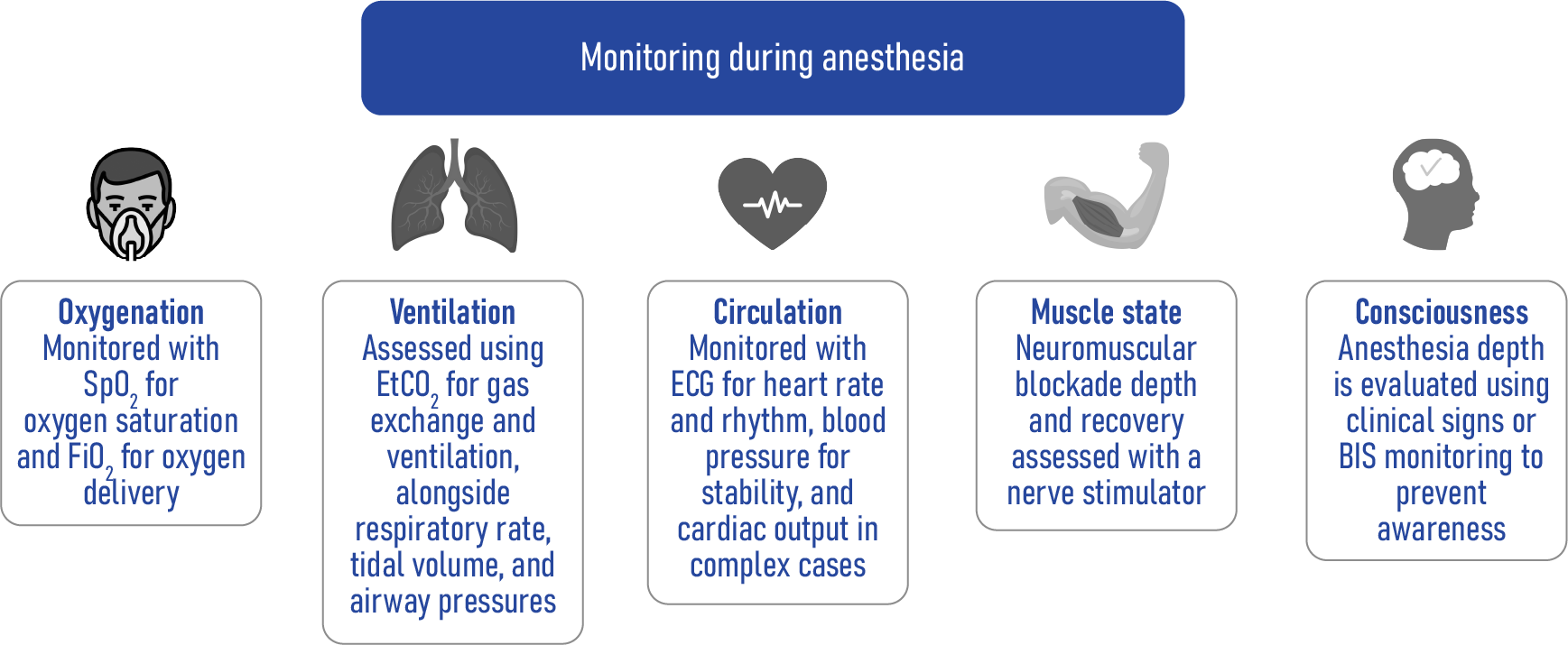
Monitoring during anesthesia: What’s measured?
The depth of anesthesia is just one component of patient monitoring during surgery. The following infographic highlights the critical aspects monitored during anesthesia:
- Oxygenation: Measured using oxygen saturation (SpO₂) and oxygen delivery (FiO₂).
- Ventilation: Assessed via end-tidal CO₂ (EtCO₂), respiratory rate, tidal volume, and airway pressures.
- Circulation: Monitored with ECG for heart rate, blood pressure, and cardiac output.
- Muscle State: Evaluated through neuromuscular blockade and recovery with nerve stimulators.
- Consciousness: Assessed through clinical signs or BIS monitoring to prevent awareness.
While these metrics are essential, the accurate monitoring of consciousness remains the most complex and debated area in anesthesia.
What is consciousness under anesthesia?
Consciousness comprises several dimensions, including:
- Wakefulness: Observable behavior and responsiveness.
- Internal awareness: Subjective self-experience.
- Connectedness: Interaction with the environment.
Anesthetic drugs can selectively impair these dimensions, creating varying states like:
- Disconnected consciousness: Awareness without environmental interaction.
- Complete unconsciousness: Absence of all conscious experiences.
What is the ideal anesthesia level for surgery?
According to the review:
- Optimal level: Disconnected consciousness – patients may dream but are not aware of surgery or pain.
- Challenges:
- Intraoperative awareness: Even with deep anesthesia, patients might recall surgery.
- Emotional Impact: Undetected stress or fear during anesthesia can have lasting effects.
Current methods to assess anesthetic depth
- Minimum Alveolar Concentration (MAC):
- Measures anesthetic input rather than consciousness.
- Population-based, not individualized.
- Limited use in multimodal anesthesia and intravenous anesthesia.
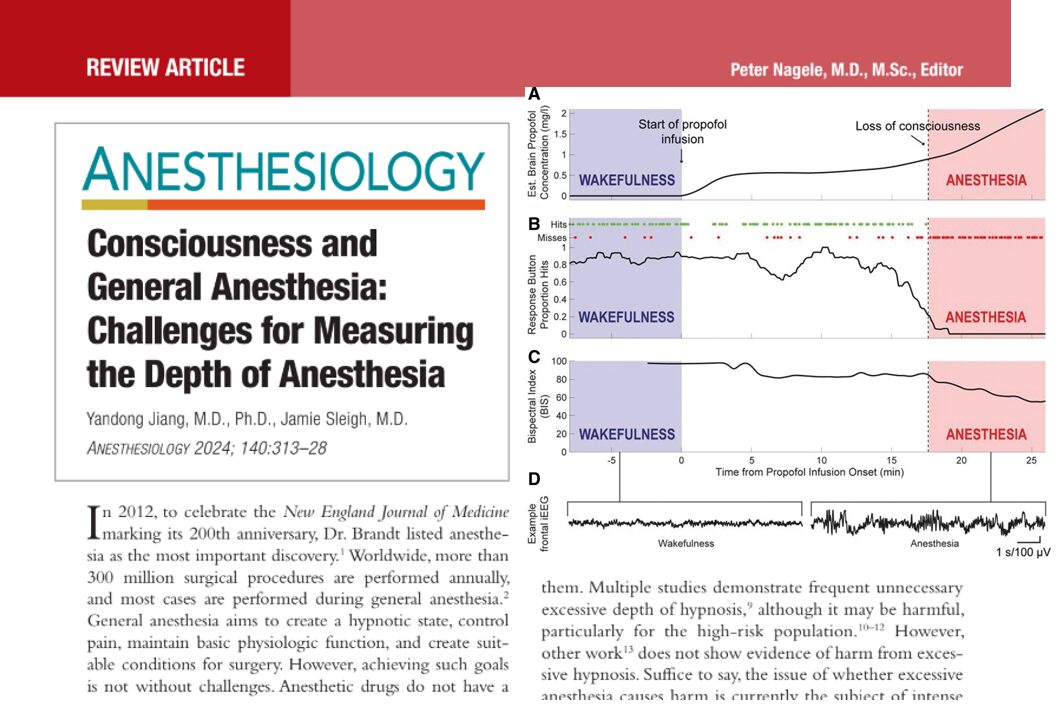
- Electroencephalogram (EEG):
- Measures brain electrical activity.
- Current devices (e.g., BIS) are based on population data and may not reliably indicate consciousness levels.
- Isolated Forearm Test (IFT):
- Detects responsiveness during paralysis.
- Reveals “partial anesthesia” states but is challenging to use routinely.
Emerging technologies for better monitoring
- Transcranial Magnetic Stimulation (TMS):
- Measures brain connectivity and complexity.
- Research tool with potential for clinical use.
- Functional Imaging (PET and fMRI):
- Provides detailed brain activity maps.
- High cost and lack of portability limit routine use.
- Functional Near-Infrared Spectroscopy (fNIRS):
- Portable and cost-effective.
- Measures blood flow changes in the brain.
- Promising but requires further validation for anesthesia use.
Artificial intelligence: The future of anesthesia monitoring
- Machine Learning (ML): Can process vast data, identify patterns, and improve accuracy.
- Deep learning models: Show high accuracy (up to 95.9%) in distinguishing consciousness from unconsciousness.
- Advantages:
- Near real-time assessment.
- Potential to detect subtle consciousness states, including sensory disconnection.
- Challenges:
- Training data often based on responsiveness, not true consciousness.
- Need for optimization and large-scale validation.
Steps toward better anesthesia monitoring
- Define the target state: Aim for disconnected consciousness without pain or fear.
- Develop reliable tools: Invest in technologies like EEG, TMS, and fNIRS.
- Incorporate AI: Use deep learning for real-time, accurate assessments.
- Individualize anesthesia: Move from population-based metrics to patient-specific monitoring.
- Focus on emotional well-being: Assess not just consciousness but also emotional states during surgery.
Conclusion
The review by Jiang et al. highlights the urgent need for improved anesthesia monitoring tools. With advances in AI and neuroimaging, the future of anesthesia promises more precise, individualized care, ensuring patients remain safe, unaware, and comfortable during surgery.
For detailed insights, refer to the full article in Anesthesiology (2024), available here.
Read about this topic and more in NYSORA’s Anesthesia Updates 2025. Don’t miss out—get your copy on Amazon or Google Books.