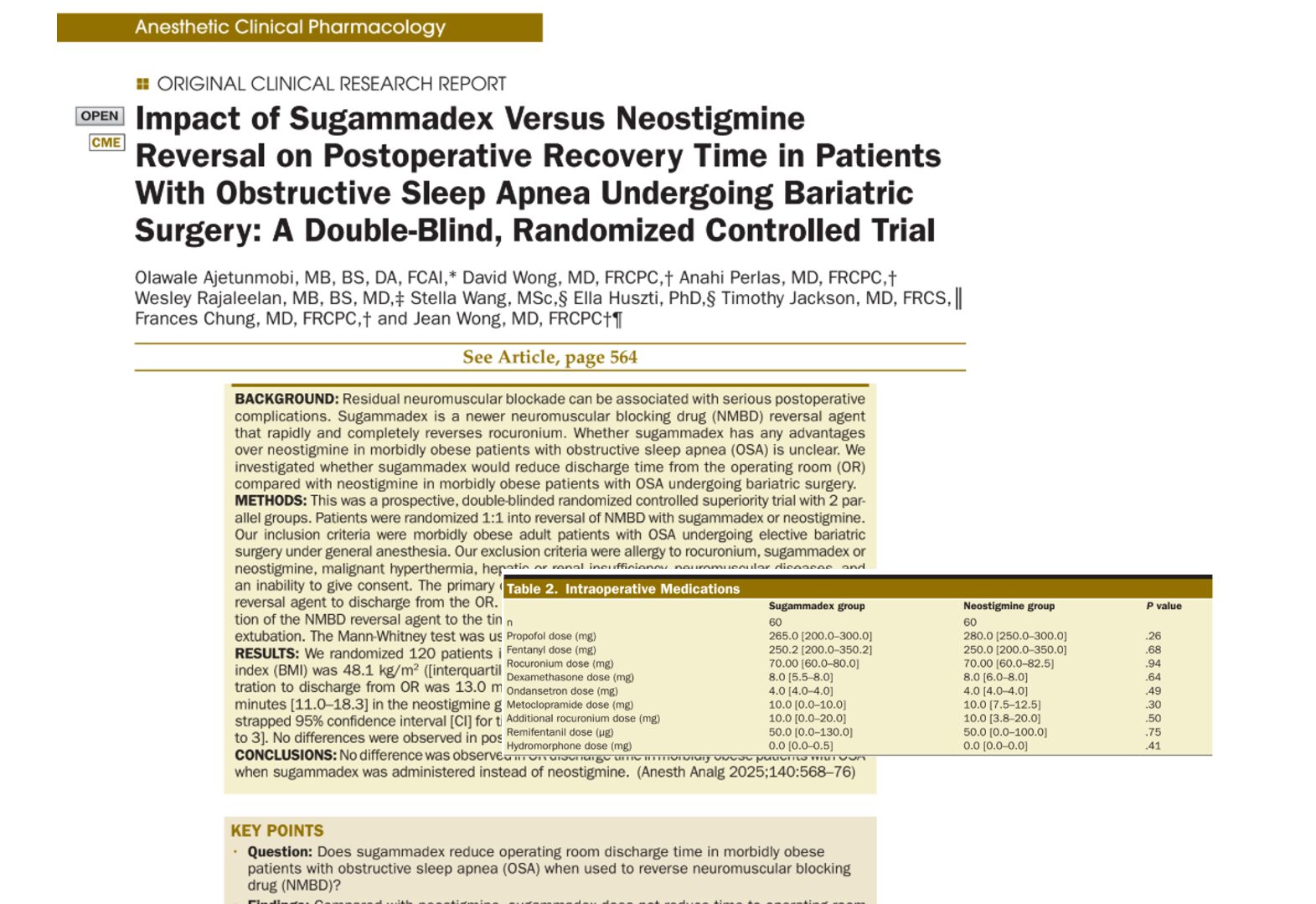
A double-blind, randomized controlled trial led by Dr. Ajetunmobi and colleagues (A&A, 2025) has revealed that sugammadex, a newer neuromuscular blockade reversal agent, does not offer a faster recovery from anesthesia compared to neostigmine in morbidly obese patients with obstructive sleep apnea (OSA) undergoing bariatric surgery.
Background
Neuromuscular blocking drugs (NMBDs) are essential in bariatric procedures to facilitate intubation and muscle relaxation. However, reversing their effects postoperatively is critical to avoid complications such as residual neuromuscular blockade (NMB), which can occur in up to 64% of cases when using neostigmine.
OSA, prevalent in 71–86% of bariatric surgery patients, significantly increases the risk of postoperative pulmonary complications. Given these risks, a more effective and faster NMBD reversal could be beneficial in improving outcomes.
Study design
- Type: Double-blind, randomized controlled trial
- Participants: 120 morbidly obese adults diagnosed with OSA
- Interventions: Patients were randomized 1:1 to receive either:
- Sugammadex (2 mg/kg)
- Neostigmine (2.5 mg) + glycopyrrolate (0.4 mg)
- Sugammadex (2 mg/kg)
- Monitoring: Train-of-four (TOF) count was used to assess neuromuscular function
- Primary outcome: Time from drug administration to discharge from the operating room (OR)
Key findings
No significant difference in the primary outcome
- Sugammadex group: Median OR discharge time of 13.0 minutes
- Neostigmine group: Median OR discharge time of 13.5 minutes
Secondary outcomes
No significant differences were observed in:
- Time to extubation
- Time to eye-opening
- Time to strong hand grip
- Time to move from the OR table to the bed
PACU (Postanesthesia Care Unit) differences
- PACU stay was longer in the sugammadex group: 150 vs. 127 minutes (This result is confounded by a mandatory 2-hour PACU stay policy for OSA patients.)
Safety outcomes
- No significant differences in intraoperative or postoperative complications.
- Incidence of desaturation in PACU: 5 patients (sugammadex) vs. 3 (neostigmine)
- No cases of severe postoperative pulmonary complications
Important considerations
Cost difference
- Sugammadex: ~$95 per vial
- Neostigmine: ~$4 per dose
Due to its high cost, sugammadex is typically reserved for rescue scenarios at many institutions.
Methodological limitations
- The neostigmine dose (2.5 mg) was lower than current dosing recommendations based on patient weight.
- The study lacked quantitative neuromuscular monitoring, which may affect the ability to detect residual NMB.
- PACU discharge was not assessed; all patients were kept a minimum of 2 hours due to institutional policy.
Clinical implications
- This study supports continued use of neostigmine as a cost-effective, clinically equivalent alternative to sugammadex in routine bariatric cases.
- The low rate of complications underscores the importance of high-volume, experienced centers in managing patients with OSA who are at high risk.
Summary in bullet points
- Sugammadex and neostigmine provided similar OR discharge times in OSA patients.
- No significant differences in recovery milestones or complication rates.
- Sugammadex did not reduce postoperative pulmonary risks compared to neostigmine.
- Study supports neostigmine as an effective and economical choice for NMBD reversal.
- More robust, quantitatively monitored, and cost-focused trials are warranted.
Reference: Ajetunmobi O et al. Anesth Analg. 2025;140:568-576.
For more information on sugammadex and its impact on perioperative care, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Here’s what Anesthesia Assistant recommends:
Which one is more effective? Neostigmine or suggamadex in obese patients with OSA undergoing bariatric surgery?