Goal-directed hemodynamic therapy (GDHT) is a tailored approach to managing blood flow and oxygen delivery during surgery. Despite its strong physiological rationale, recent evidence has challenged its broad application, prompting the need for updated clinical guidance.
The 11th Perioperative Quality Initiative (POQI-11) meeting in London, UK, convened experts to review and update consensus on GDHT based on evolving evidence, including findings from the large OPTIMISE II trial.
What is goal-directed hemodynamic therapy?
GDHT is a protocolised strategy used to optimise cardiovascular performance during the perioperative period. It involves continuous monitoring and targeted use of:
- Intravenous fluids
- Vasopressors (to increase vascular tone and blood pressure)
- Inotropes (to enhance cardiac contractility)
Key goals:
- Improve tissue oxygen delivery (DO₂)
- Maintain adequate mean arterial pressure (MAP)
- Reduce postoperative complications
Components of GDHT protocols
A GDHT protocol must clearly define:
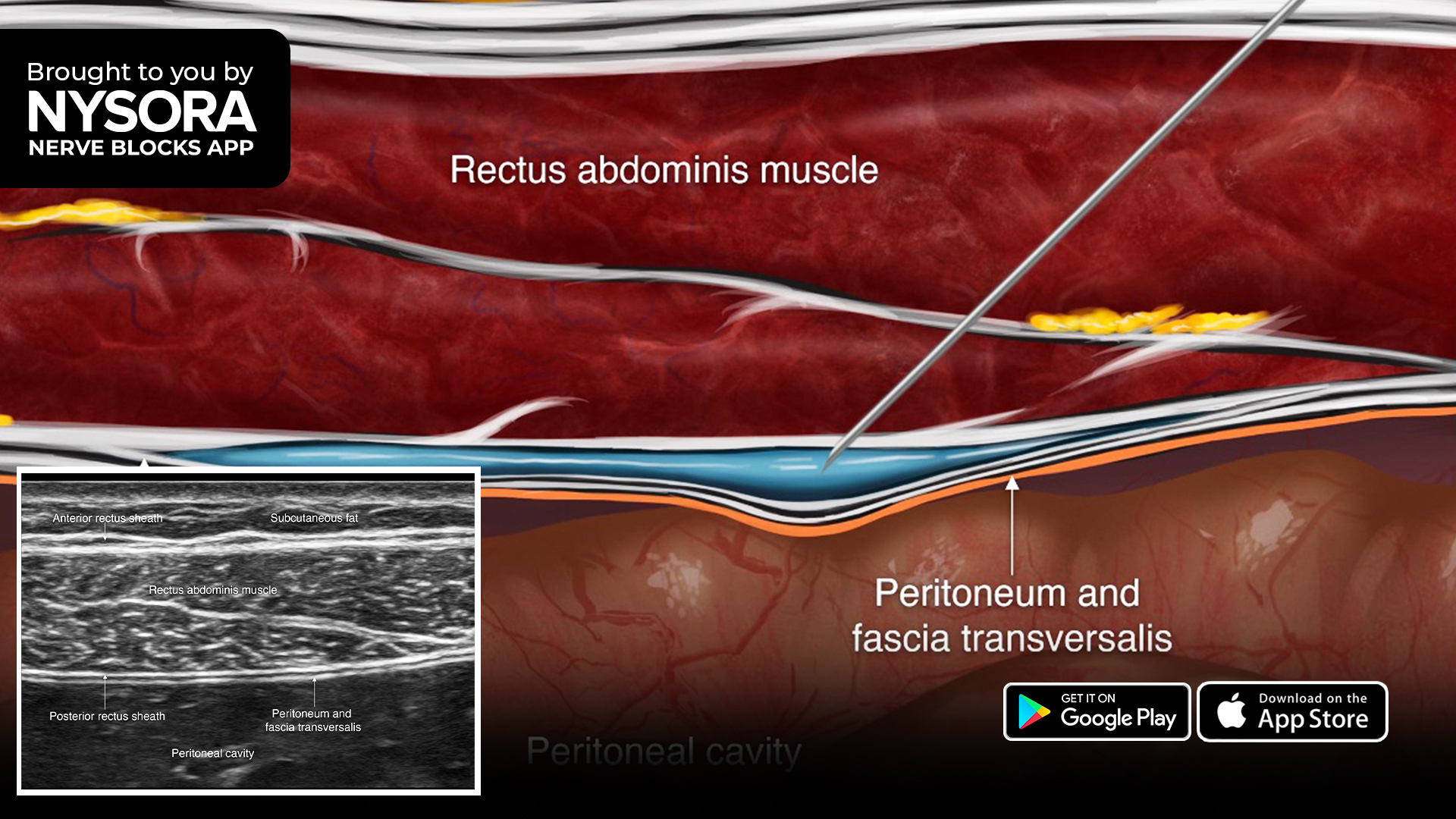
- Monitoring tools: e.g., oesophageal Doppler, pulse contour analysis, pulmonary artery catheters
- Physiological targets: e.g., stroke volume (SV), cardiac output (CO), MAP
- Treatment interventions: e.g., fluid boluses, vasopressors, inotropes
- Timing: intraoperative, postoperative, or both
Commonly monitored variables
- Stroke volume (SV)
- Cardiac output (CO)
- Systemic vascular resistance
- Central venous oxygen saturation
- Urine output
- Serum lactate
Key recommendations from POQI-11
- Avoid routine GDHT in elective major abdominal surgery
- Strong recommendation, high-quality evidence
- Strong recommendation, high-quality evidence
- Consider GDHT for high-risk noncardiac surgeries
- Weak recommendation, moderate evidence
- Weak recommendation, moderate evidence
- Avoid fixed-dose inotrope infusions in GDHT protocols
- Strong recommendation, high-quality evidence
- Strong recommendation, high-quality evidence
- Use dynamic tests to assess fluid responsiveness
- e.g., stroke volume variation (SVV), passive leg raise (PLR)
- e.g., stroke volume variation (SVV), passive leg raise (PLR)
- Use DO₂ and MAP as targets, not just fluid loading
When to consider GDHT
POQI-11 suggests considering GDHT in these clinical contexts:
- Cardiac surgery: postoperatively to reduce complications
- During cardiopulmonary bypass (CPB): to prevent acute kidney injury (AKI)
- Hip fracture surgery: particularly in elderly patients
- Select noncardiac surgeries: when the patient is high-risk or unstable
Step-by-step: implementing GDHT
- Assess baseline risk
Evaluate patient’s surgical risk (ASA status, comorbidities).
- Choose appropriate monitoring
Select minimally invasive tools when possible (e.g., Doppler, pulse analysis).
- Set target values
- MAP > 65 mm Hg
- SVV < 13%
- DO₂ > 600 mL/min/m²
- Start fluid optimisation
Administer a 250 mL bolus. Measure SV response.
- Determine responsiveness
- If SV increases >10%, the patient is fluid responsive
- If not, reassess or consider vasopressors/inotropes
- Add pharmacologic support if needed
Only titrate vasopressors/inotropes to meet hemodynamic goals
- Monitor and reassess frequently
Continue trend monitoring intra- and post-operatively
New directions for GDHT
POQI-11 outlines future research priorities:
- Individualised protocols
Explore patient-specific endotypes and hemodynamic patterns.
- AI and predictive algorithms
Investigate machine learning to predict instability and optimise therapy. - Closed-loop systems
Evaluate automated, responsive GDHT systems for improved target compliance.
Clinical scenarios and evidence strength

Challenges in GDHT implementation
- Heterogeneity in protocols, monitoring tools, and outcomes
- Variability in clinician adherence to physiological targets
- Lack of direct measures of tissue perfusion
- Risk of harm from inappropriate inotrope use
Summary
The updated 2025 POQI consensus reflects a more nuanced and individualised approach to GDHT. While the theoretical benefits remain compelling, recent high-quality trials challenge its routine use in broad populations. Selective implementation in high-risk patients, particularly in cardiac contexts or emergency settings, may yield the most benefit.
Reference: Edwards MR et al. PeriOperative Quality Initiative 11 (POQI-11) Group Members. Perioperative Quality Initiative consensus statement on goal-directed haemodynamic therapy. Br J Anaesth. 2025;135:547-560.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!
Q: Should goal-directed hemodynamic therapy (GDHT) be reserved only for the sickest patients?