A Silent Threat During Surgery
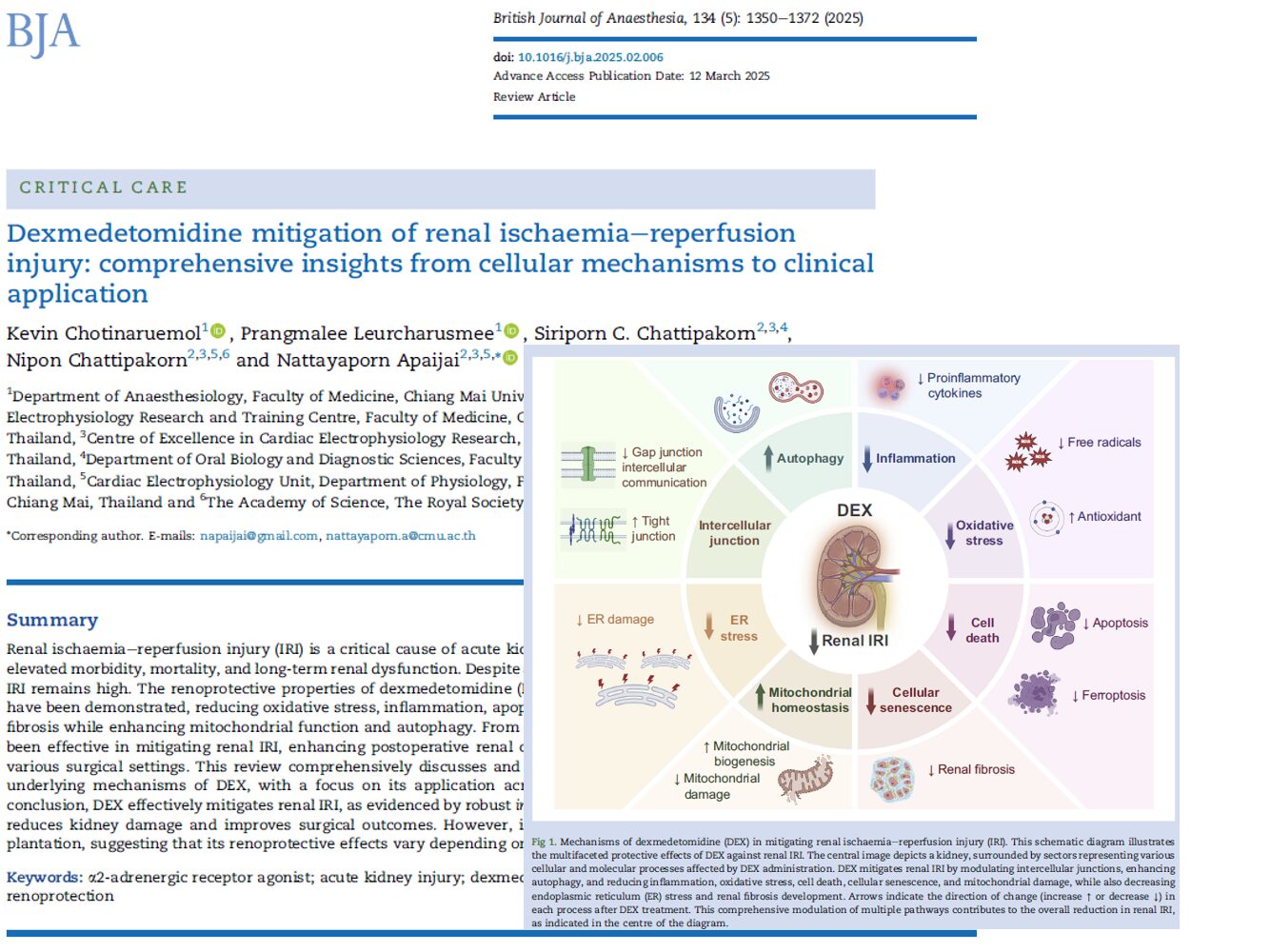
Renal ischaemia-reperfusion injury (IRI) is a critical concern in perioperative medicine. It occurs when blood supply to the kidneys is temporarily cut off and then restored, a necessary process that paradoxically causes further damage. IRI plays a major role in the development of acute kidney injury (AKI), which affects 20–40% of high-risk surgical patients. AKI is not only associated with short-term complications like fluid overload and metabolic imbalance but also contributes to long-term kidney dysfunction and increased mortality.
A new role for dexmedetomidine
Dexmedetomidine (DEX), widely used as a sedative and analgesic in intensive care and anesthesia, has gained attention for its renal protective effects. It selectively targets α2-adrenergic receptors (α2-AR), which are richly expressed in renal tissues, particularly in the proximal and distal tubules and peritubular vasculature.
Core renoprotective mechanisms of DEX:
- Reduction of oxidative stress: Enhances antioxidant defenses and reduces reactive oxygen species (ROS)
- Inflammation suppression: Inhibits cytokines like IL-6, IL-1β, and TNF-α
- Anti-apoptotic action: Prevents programmed cell death by modulating proteins like Bcl-2 and caspases
- Prevention of ferroptosis and pyroptosis: Blocks less-known forms of cell death linked to iron metabolism and inflammatory caspases
- Mitochondrial preservation: Stabilizes membrane potential and promotes biogenesis
- Stimulation of autophagy: Clears damaged cellular components
- Anti-fibrotic activity: Limits extracellular matrix accumulation and epithelial-mesenchymal transition (EMT)
- Tight junction integrity: Maintains epithelial barriers via proteins like ZO-1
Cellular studies: the lab evidence
Researchers used two main experimental models, oxygen-glucose deprivation/reoxygenation (OGD/R) and hypoxia/reoxygenation (H/R), to mimic IRI in human and animal kidney cells.
Key findings:
- DEX increases cell viability and reduces LDH release, a marker of cellular damage.
- It restores mitochondrial function by enhancing SIRT3 and PGC-1α activity.
- Inhibits the pro-apoptotic proteins like Bax and activates anti-apoptotic Bcl-2.
- Reduces inflammatory cytokines and improves gap junction integrity.
Animal models: what in vivo studies reveal
Animal experiments have consistently shown that DEX reduces serum creatinine, BUN, and histological damage after induced IRI. These benefits are linked to:
- Timing: Pre-treatment, 30 minutes before IRI, is more effective than post-treatment.
- Dose-dependent effects: Higher doses (50–100 μg/kg) offer better outcomes.
- Signaling pathways: DEX modulates SIRT3, JAK/STAT, and AMPK/mTOR pathways, all vital in kidney repair and survival.
Molecular highlights:
- SIRT3 maintains mitochondrial homeostasis.
- PGC-1α supports mitochondrial biogenesis.
- Autophagy clears cellular debris and damaged mitochondria.
- JAK/STAT inhibition reduces inflammation and fibrosis.
How dexmedetomidine protects the kidneys
- DEX binds to α2-adrenergic receptors.
- Inhibits vasopressin release, enhancing diuresis.
- Reduces oxidative stress, limiting ROS formation.
- Suppresses pro-inflammatory cytokines (IL-6, TNF-α, IL-1β).
- Preserves mitochondrial function via SIRT3 and PGC-1α.
- Inhibits cell death, both apoptosis and ferroptosis.
- Activates autophagy, promoting cellular repair.
- Prevents EMT, reducing fibrosis risk.
- Strengthens tight junctions, preserving epithelial integrity.
Special topic: dexmedetomidine in remote organ IRI
Renal damage isn’t always local. IRI in distant organs, heart, intestines, brain, can lead to secondary kidney injury due to systemic inflammation and oxidative stress.
DEX protects the kidney even in remote IRI models by:
- Reducing ER stress and mitochondrial dysfunction
- Suppressing inflammation
- Restoring antioxidant levels
Clinical implications and limitations
Where DEX excels:
- Perioperative care in high-risk surgeries
- Prevention of AKI in intensive care
- Sepsis-related and drug-induced AKI
Challenges:
- Limited efficacy in renal transplant scenarios
- Optimal dosing protocols need standardization
- Long-term human trial data are limited
Conclusion: from bench to bedside
Dexmedetomidine is redefining its role in perioperative medicine—not just as a sedative, but as a potent kidney protector. By acting on multiple pathways involved in cell injury, inflammation, and repair, DEX offers a multi-targeted approach to reduce renal IRI. While more clinical research is essential, current evidence supports the broader integration of DEX in protocols aimed at reducing surgical AKI and improving long-term renal outcomes.
Reference: Chotinaruemol K et al. Dexmedetomidine mitigation of renal ischaemia-reperfusion injury: comprehensive insights from cellular mechanisms to clinical application. Br J Anaesth. 2025;134:1350-1372.
For more information on dexmedetomidine and its use in perioperative care, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
AI On Call: Case of the Week
A 72-year-old male with hypertension, type 2 diabetes, and stage 3 chronic kidney disease (baseline creatinine 1.8 mg/dL) comes in for an elective open abdominal aortic aneurysm (AAA) repair.
Here’s what the Assistant recommends doing: