Introduction
Total knee and hip arthroplasty (TKA and THA) are among the most commonly performed surgical procedures worldwide. As populations age and demand for joint replacements rises, ensuring optimal recovery and minimizing complications has become a clinical priority. A recent multicenter study led by Garcia-Casanovas and published in Anesthesiology (2025) delivers robust evidence that higher adherence to patient blood management (PBM) guidelines leads to significantly better patient outcomes.
What is patient blood management?
PBM is a proactive, multidisciplinary approach that:
- Optimizes the patient’s own blood resources
- Reduces the need for allogeneic blood transfusions
- Minimizes surgical blood loss
- Enhances recovery and reduces complications
PBM follows a “three-pillar” strategy:
- Optimize red blood cell mass (e.g., detect and treat preoperative anemia)
- Minimize blood loss and bleeding (e.g., use antifibrinolytics and regional anesthesia)
- Enhance patient tolerance to anemia (e.g., set restrictive transfusion thresholds)
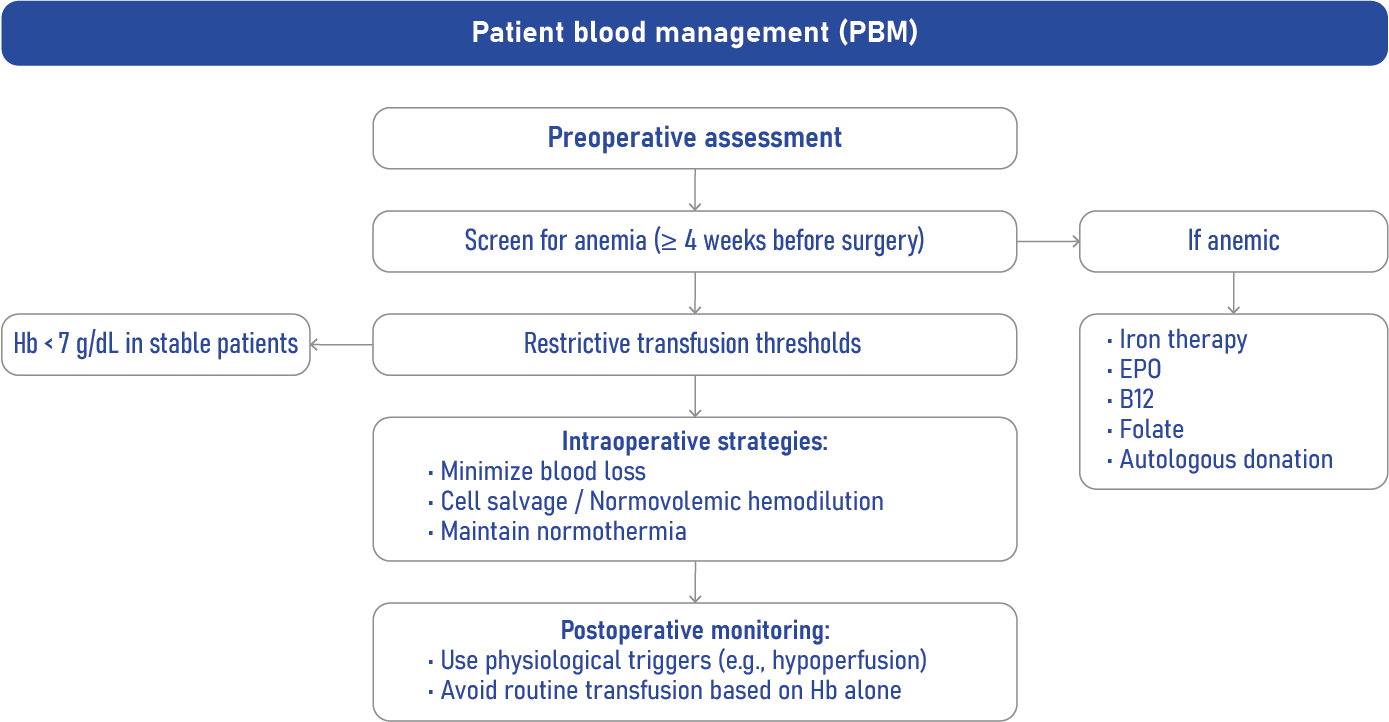
PBM is globally endorsed, including by the World Health Organization, for its clinical and economic benefits.
Study overview
- Study design: Retrospective multicenter cohort
- Period: 2016–2022
- Sample size: 30,926 patients
- Settings: 43 hospitals in Spain and Andorra
- Procedures: Elective primary TKA and THA
- Analysis: Composite Quality Indicator (CQI) across 9 guideline-based PBM interventions
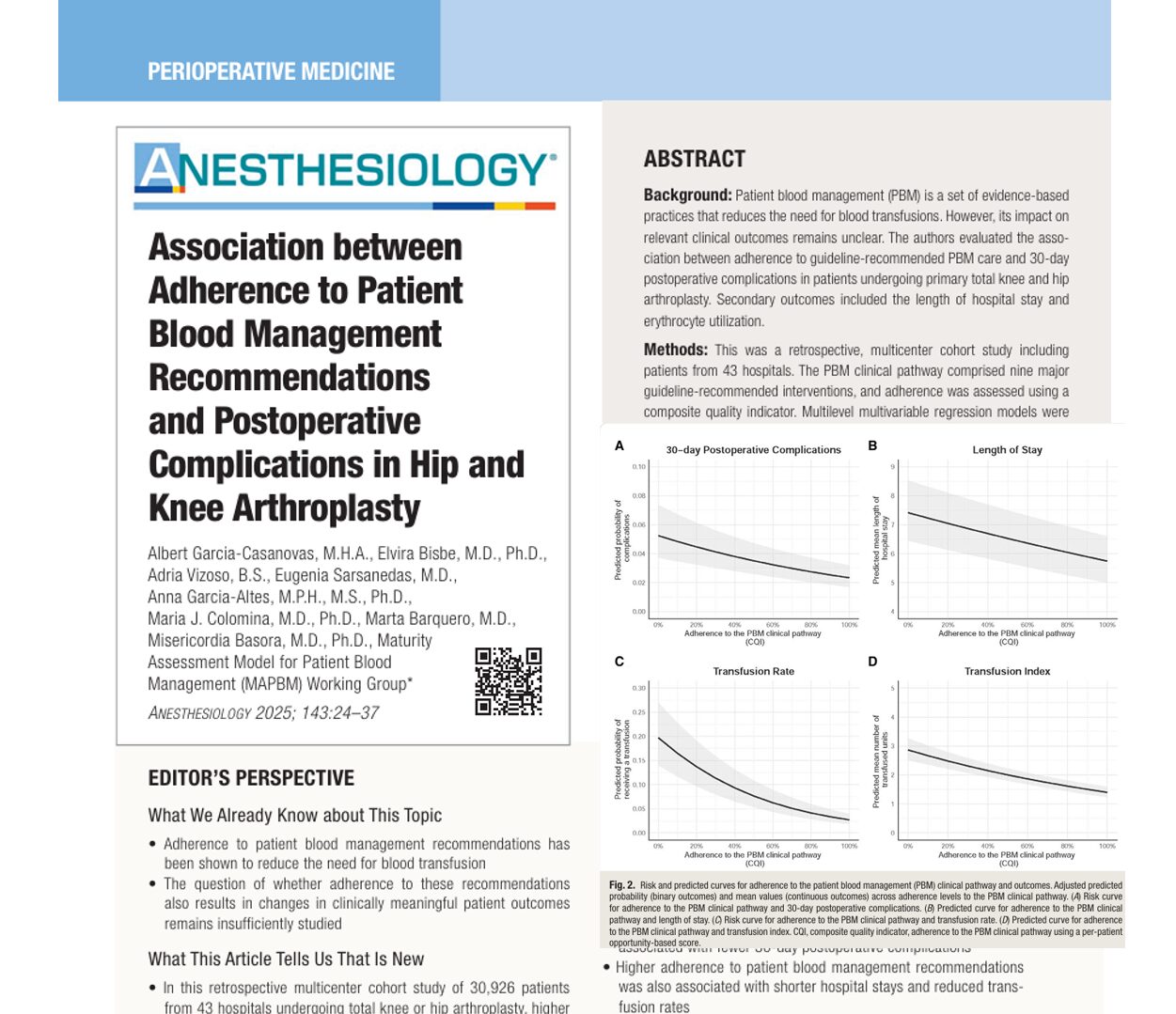
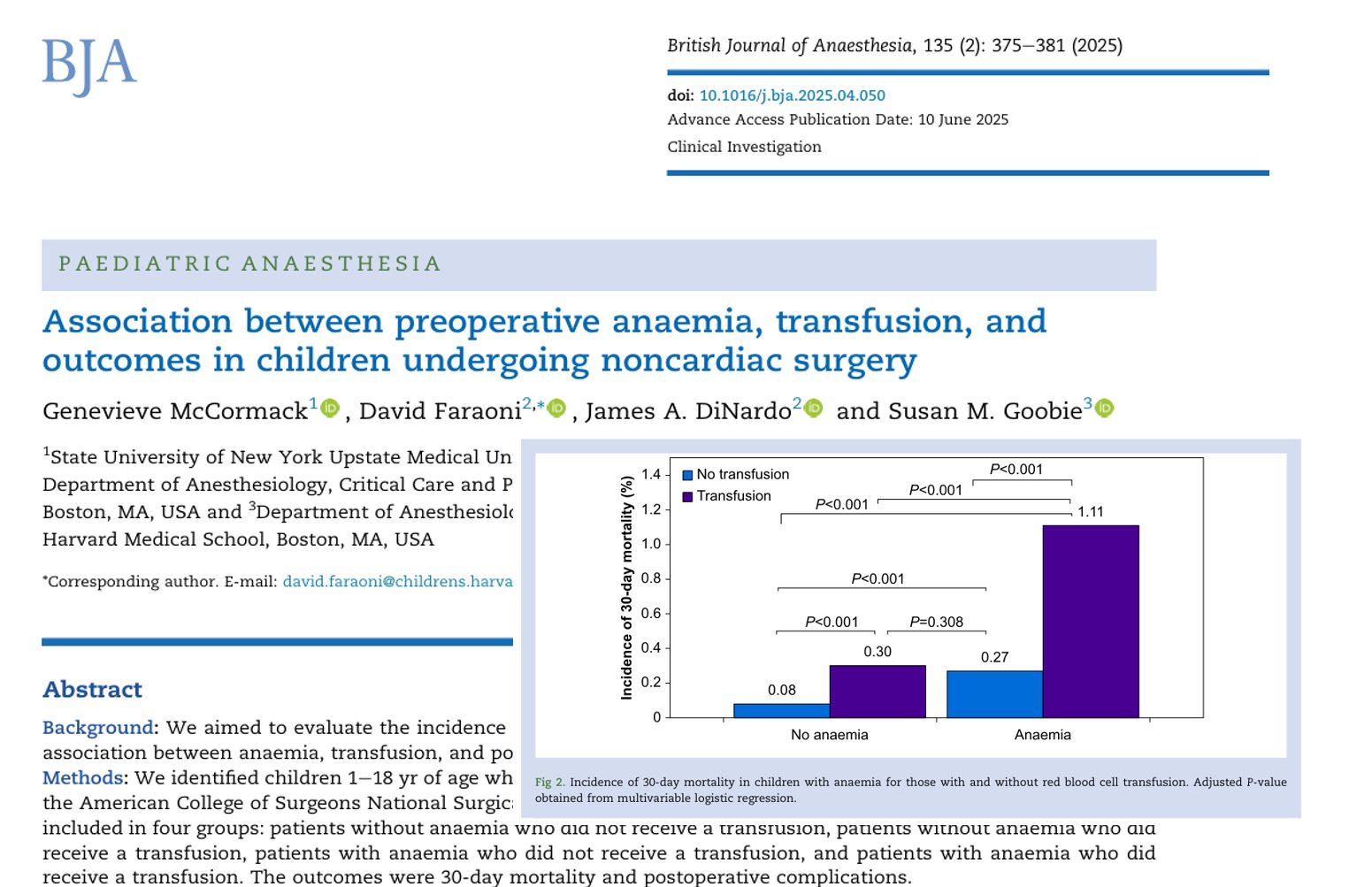
Core findings
Patients with higher adherence to PBM experienced:
- 57% fewer 30-day postoperative complications
- 65% lower odds of major adverse cardiac events (MACE)
- 45% lower odds of infection
- 23% shorter hospital stays
- 89% lower transfusion rates
- 51% lower transfusion index (units per patient)
Key interventions tracked
The study assessed compliance with nine critical interventions, each contributing to the CQI:
- Timely screening for preoperative anemia
- Assessment of iron metabolism
- Timely treatment of preoperative anemia
- Undergoing surgery without anemia
- Treatment of postoperative anemia
- Use of regional anesthesia
- Use of antifibrinolytics
- Use of restrictive transfusion thresholds
- Single-unit transfusions
Notable trends:
- Underutilized interventions: Pre- and postoperative anemia treatments had the lowest adherence rates (23.4% and 8.6%, respectively).
- Strongest impact: Surgery without anemia, antifibrinolytic use, and restrictive transfusion thresholds were most strongly linked to improved outcomes.
Conclusion
This extensive research affirms that strict adherence to a patient blood management pathway significantly reduces complications and resource use in joint replacement surgeries. It supports calls for broader adoption of PBM as standard perioperative care.
By focusing not only on reducing transfusions but also on improving patient-centered outcomes, PBM offers a win-win for patients and health systems alike.
Reference: Garcia-Casanovas A et al. Association between Adherence to Patient Blood Management Recommendations and Postoperative Complications in Hip and Knee Arthroplasty. Anesthesiology. 2025;143:24-37.
For more information on patient blood management guidelines, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Here is a test for the Medical AI Assistant (MAIA) in the Anesthesia Manual app:
A 74-year-old woman is scheduled for elective total hip arthroplasty.
She has mild chronic kidney disease and her preoperative hemoglobin is 11.1 g/dL.
What measures can be taken to reduce her risk of postoperative complications?