Spinal cord stimulation (SCS) has emerged over the past three decades as a transformative therapy for managing chronic, treatment-resistant pain. Yet, new research suggests that who receives this therapy, and under what circumstances, varies dramatically around the world. A newly published systematic review and meta-analysis in Regional Anesthesia & Pain Medicine offers the first comprehensive global snapshot of SCS usage, uncovering major disparities in patient age, diagnosis, geographic access, and funding support.
Led by Dr. Peter Vu and colleagues, this international research team synthesized data from 187 studies, encompassing over 16,000 patients across 28 countries and six continents. Their findings highlight not only how SCS is used globally, but who is being left behind, and why.
What is spinal cord stimulation?
Spinal cord stimulation (SCS) is a type of neuromodulation therapy in which electrical impulses are delivered to the dorsal column of the spinal cord through implanted electrodes. These impulses mask or modify pain signals before they reach the brain. Initially developed for refractory back and leg pain, its indications have expanded to include:
- Post-surgical pain syndrome (PSPS1 and PSPS2)
- Complex regional pain syndrome (CRPS)
- Diabetic peripheral neuropathy (DPN)
- Peripheral vascular disease (PVD)
- Postherpetic neuralgia (PHN)
- Radiculopathy and nerve root compression syndromes
Despite its effectiveness, the therapy remains invasive, costly, and inconsistently funded, making it less accessible in many parts of the world.
Why this study matters
While numerous clinical trials have documented SCS efficacy and safety, no previous review has analyzed global patterns of usage across diverse populations. This study fills that gap by examining:
- Patient demographics (age, gender)
- Pain diagnoses
- Regional trends
- Funding sources
- Study designs and outcomes
By identifying disparities, the authors aim to guide more equitable policy and clinical decision-making in neuromodulation.
Key findings from the meta-analysis
-
Global average age of SCS patients: 55.8 years
- Across all studies, the mean patient age was 55.84 years (95% CI: 54.89–56.79).
- Age ranged widely from 38.6 to 80.7 years, indicating substantial geographic and clinical variability.
-
Geographic age disparities
Significant regional differences were observed:

- Asian patients were on average 8.6 years older than those in North America.
- Country-specific factors (healthcare policy, reimbursement models) accounted for 37.1% of the age variation.
-
Most common diagnoses: PSPS2 and CRPS
Pain syndromes driving SCS implantation included:
- Post-surgical pain syndrome (thoracolumbar, PSPS2): 44.9%
- CRPS: 13.5%
- Chronic low back pain (PSPS1): 13.5%
- Radiculopathy: 11.3%
- Neuropathic leg or neck pain: 10–12%
- Other syndromes (DPN, PHN, PVD): 3–5%
Patients with DPN or vascular pain were significantly older than those with CRPS or cervical radiculopathy, highlighting age-diagnosis interactions.
-
Gender parity
Across studies, 53% of SCS recipients were female, with no significant gender differences observed across regions or diagnoses.
Funding disparities and research bias
Who’s funding the science?
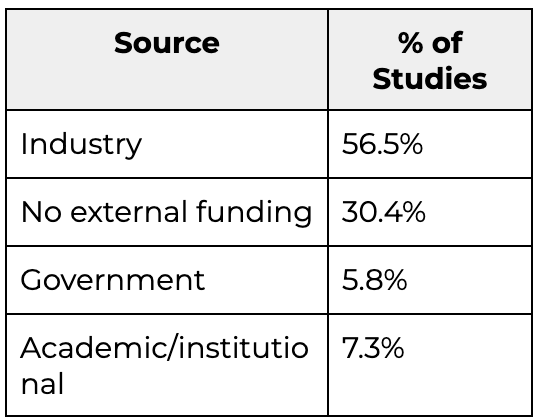
- Industry-funded studies were concentrated in Europe and North America.
- Only 6% of studies received governmental funding, suggesting a heavy reliance on manufacturers to support research.
Interestingly, funding source did not correlate with patient age, suggesting bias may affect research scope more than study design.
Study design breakdown
Of the 207 eligible studies (187 with complete data):
- 67.4% were observational cohort studies
- 22.9% were randomized controlled trials (RCTs)
- 6.4% were case series
- 3.2% were registry-based analyses
This distribution reflects the real-world focus of much of the SCS literature but highlights a need for more high-quality RCTs, especially in underrepresented regions.
Meta-regression and statistical modeling
The study employed meta-regression techniques to identify drivers of variation in patient age:
- Country-level characteristics explained 37.1% of the variance
- Continental differences accounted for 8.95%
- Diagnosis explained 17.2%
- Funding source showed no significant effect
- Study design and setting (public vs private hospitals) were also non-significant predictors
Clinical implications
This analysis provides actionable insights for pain specialists, health policymakers, and neuromodulation researchers:
- Patient age and diagnosis should be carefully considered in device selection and programming.
- Older patients may benefit from simplified, non-rechargeable devices with fewer complications.
- Resource allocation and training must be expanded in LMICs to improve equitable access.
- Standardized reporting of patient demographics in SCS trials is critical for global benchmarking.
Limitations of the study
The authors acknowledge several constraints:
- Low GRADE quality due to reliance on non-randomized studies
- Inconsistent outcome reporting across countries and diagnoses
- Lack of socioeconomic data on patients
- Publication bias was not formally assessed
Still, the review provides the most comprehensive SCS demographic synthesis to date.
Recommendations for future research
To close the knowledge and equity gaps in SCS therapy, the authors recommend:
- Expanding research in low-resource regions
- Funding independent, non-industry trials
- Standardizing demographic and outcome reporting
- Studying long-term outcomes stratified by age and diagnosis
- Integrating registry data with real-world evidence platforms
Conclusion
Spinal cord stimulation continues to evolve as a vital therapy for managing complex, chronic pain syndromes. However, this global meta-analysis reveals that access to this therapy remains uneven and age-dependent, shaped by systemic healthcare differences and economic barriers.
Vu PD, Mamun N, Feng L, et al. Global usage of spinal cord stimulation therapy for chronic pain syndromes: a systematic review and meta-analysis. Reg Anesth Pain Med. Published online August 31, 2025.
The findings provide an essential foundation for building more inclusive, representative, and equitable pain management systems worldwide. For patients, clinicians, and policymakers alike, it’s a call to action: innovation must be paired with accessibility, and global excellence must include global equity.
For more information, refer to the full article in RAPM.
For step-by-step guidance on chronic pain management and recent literature updates, download NYSORA’s Pain Medicine Assistant App.