Postoperative delirium (POD) is a frequent, preventable, and serious complication in surgical patients, particularly in older adults. The 2024 update of the European Society of Anaesthesiology and Intensive Care (ESAIC) guidelines brings crucial advancements in the understanding, prevention, and management of POD.
What is postoperative delirium?
POD is an acute neurocognitive disorder that typically occurs within the first few days after surgery. It is characterized by:
- Inattention
- Altered consciousness or disorganized thinking
- Fluctuating course
POD is associated with:
- Longer hospital stays
- Higher complication rates
- Increased mortality and long-term cognitive decline
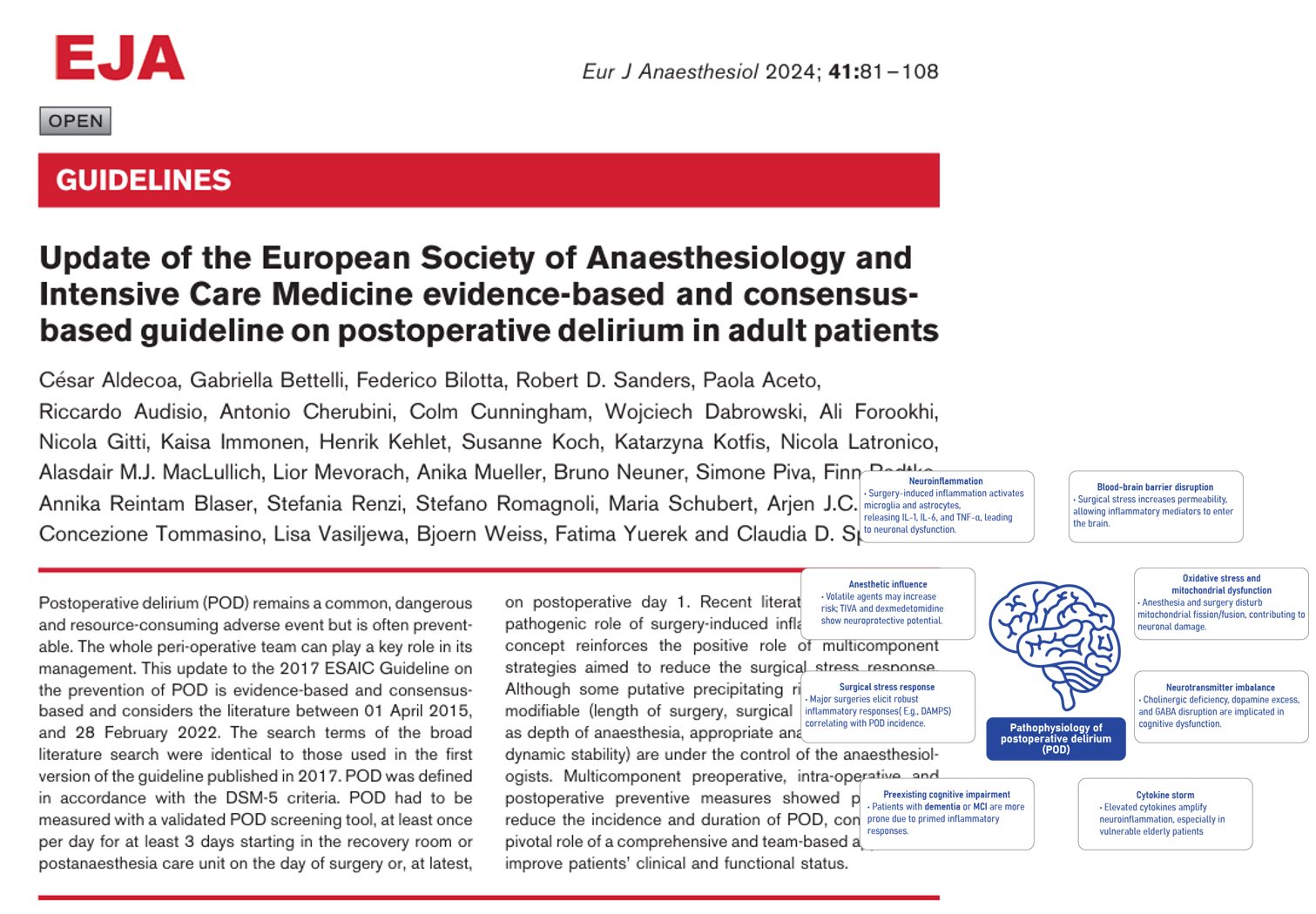
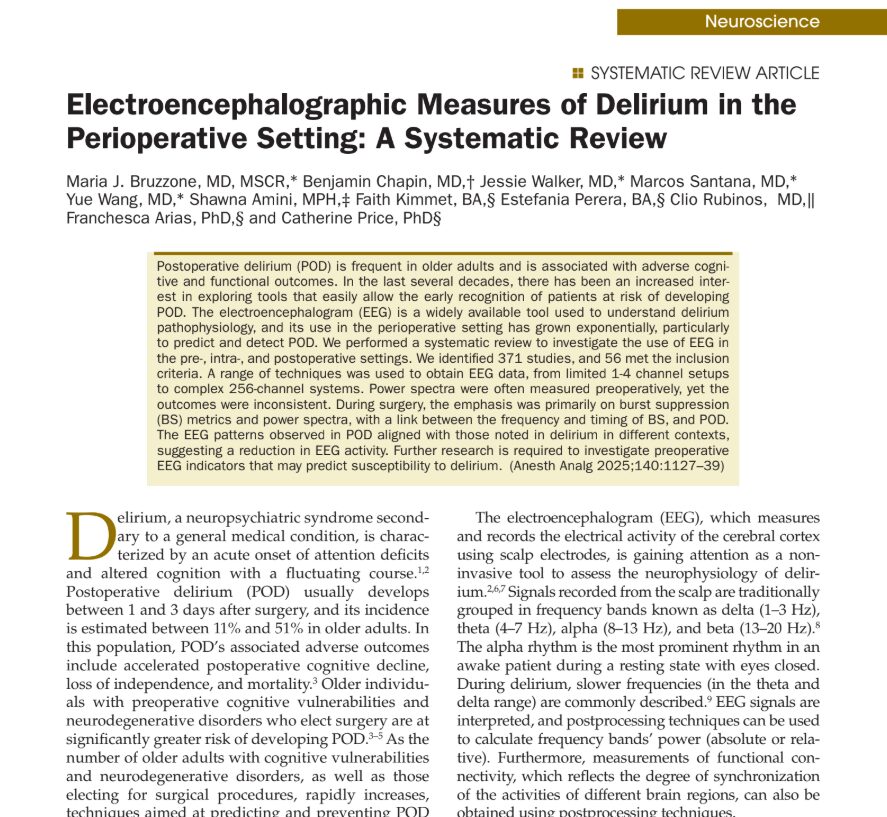
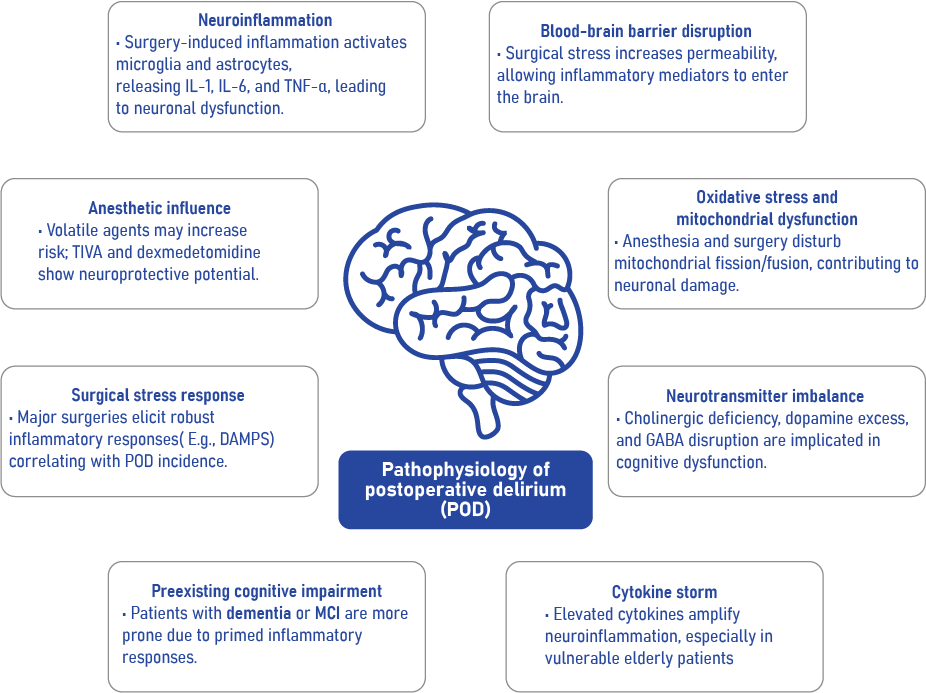
Pathophysiology of POD
POD arises from the interaction between preexisting patient vulnerabilities and surgical stressors that affect the brain. The updated guidelines highlight several key biological mechanisms.
Major contributors include:
- Neuroinflammation triggered by surgery
- Blood-brain barrier disruption
- Mitochondrial dysfunction
- Neurotransmitter imbalances
- Preexisting cognitive impairment
- Cytokine storms and anesthetic influence
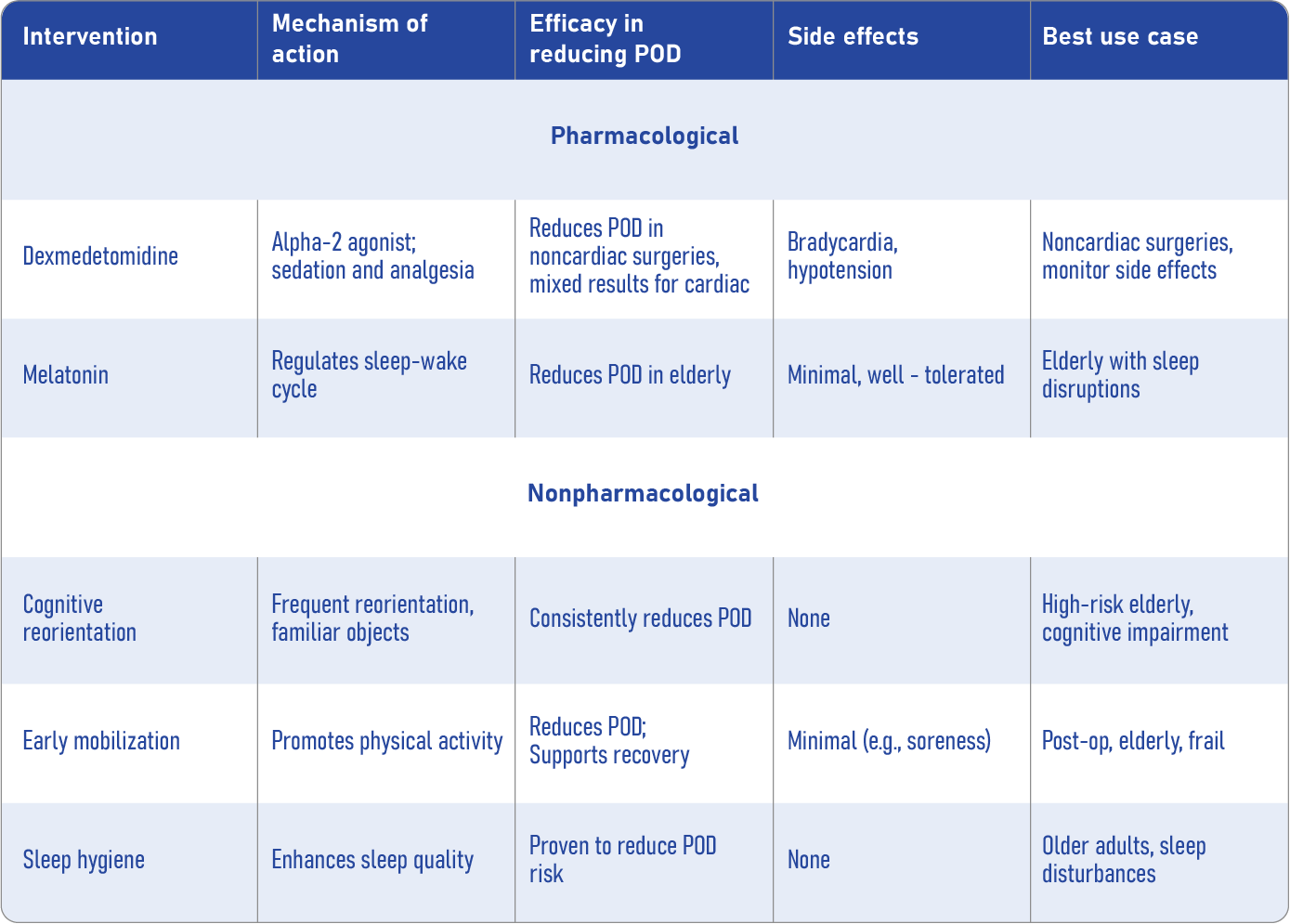
Pharmacological vs. nonpharmacological interventions
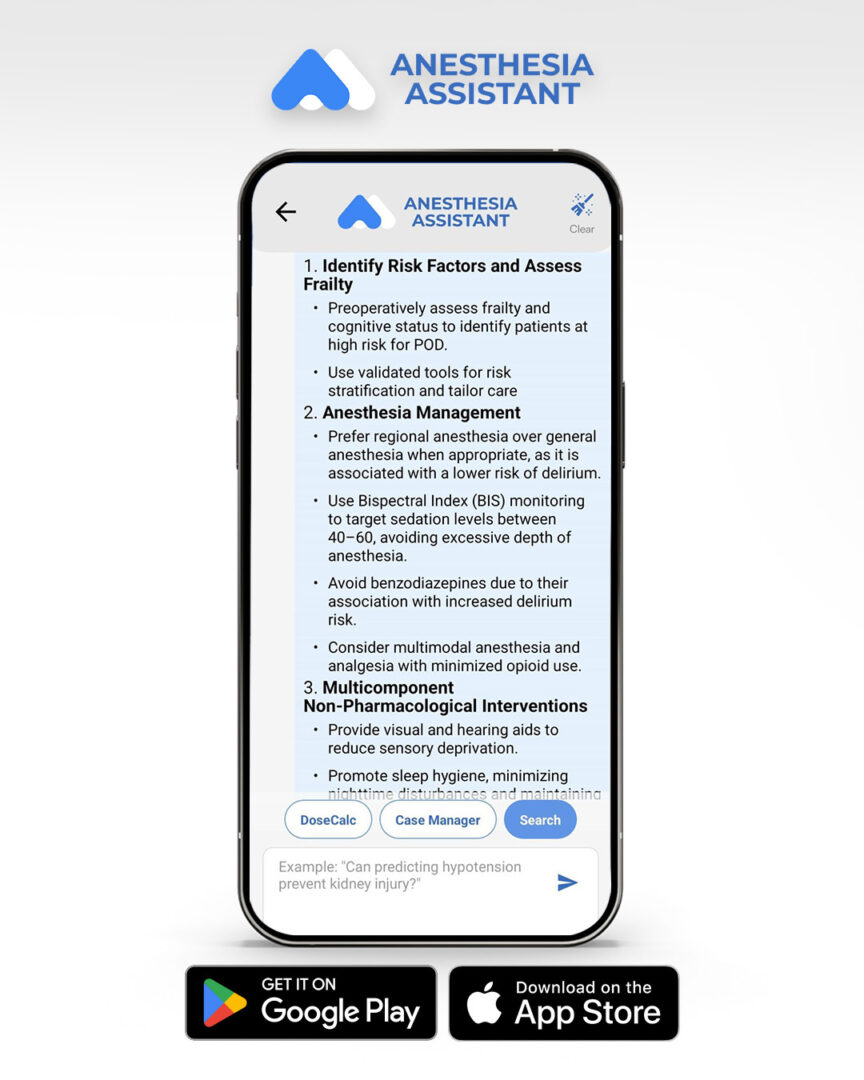
The new ESAIC guideline recommends a multimodal prevention approach. Below is a summary of interventions by category:
Evidence-based strategies: what works best?
Strongly recommended
- Preoperative risk screening
- Multicomponent nonpharmacological bundles
- Team-based care planning
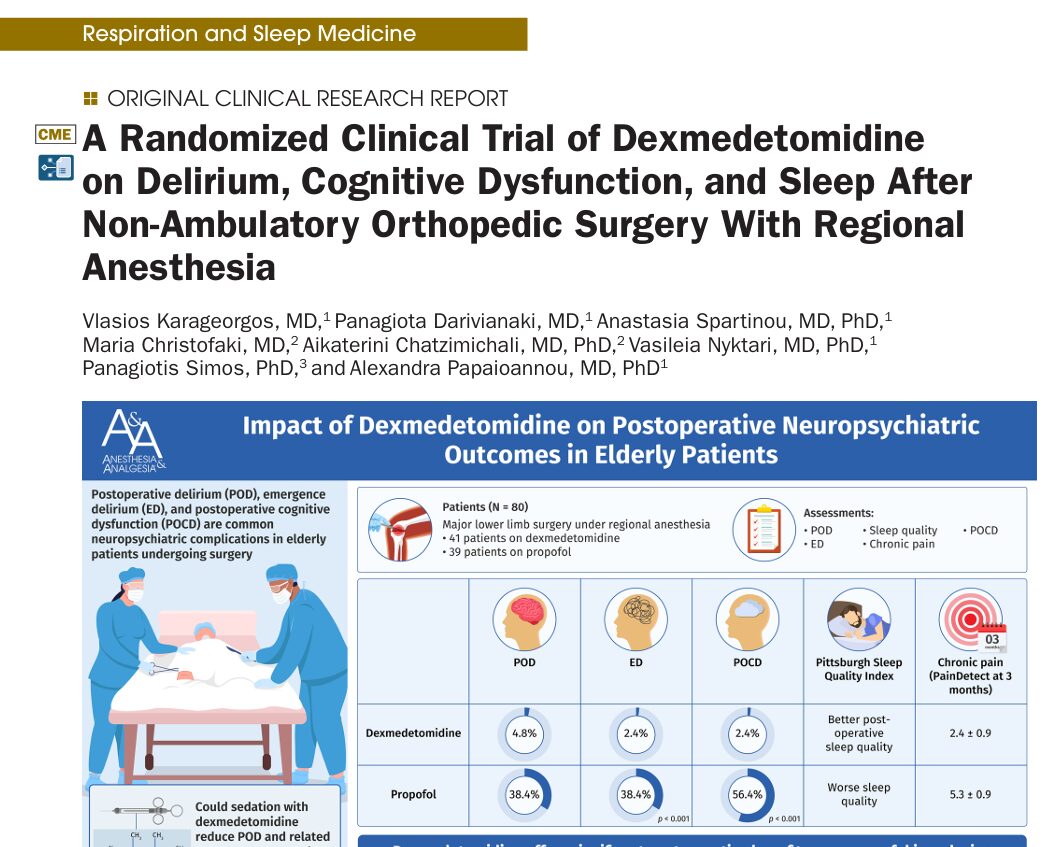
- Dexmedetomidine use (with caution) in selected patients
Not recommended for routine use
- Haloperidol or other neuroleptics
- Cholinesterase inhibitors
- Routine biomarker screening
- Specific anesthesia types (general vs regional)
How to prevent POD: step-by-step guide
1. Screen preoperatively
Use tools like MMSE, MOCA, or Mini-Cog. Assess:
- Cognitive function
- Frailty
- Comorbidities
- Medication list
- Nutritional status
2. Inform and coordinate the team
Document POD risk clearly in medical records and share with:
- Anaesthesiologists
- Surgeons
- Nurses
- Geriatric teams
3. Implement prevention bundles
Focus on:
- Reorientation strategies
- Sleep hygiene (quiet room, eye masks)
- Early mobilisation
- Nutrition support
- Family involvement
4. Monitor for POD
Use validated tools (CAM-ICU, Nu-DESC) daily for 3 days post-op, starting in recovery.
Key recommendations
- Risk screening: Mandatory for patients ≥60 years
- Cognitive tools: Mini-Cog, MOCA, ACE-R (MMSE if available)
- Drugs: Dexmedetomidine only in selected cases
- Non-drug measures: Multicomponent bundles strongly encouraged
- Anaesthesia type: No clear advantage of general vs. regional
- Surgery type: No conclusive difference between laparotomy and laparoscopy
- Biomarkers: Not currently recommended due to low specificity
Conclusion
The 2024 ESAIC guideline underscores a vital truth: postoperative delirium is preventable, but only through proactive, patient-specific, multidisciplinary action. Clinicians should focus on early screening, personalized care plans, and team communication to effectively reduce POD incidence and improve surgical outcomes.
Case of The Week with Anesthesia Assistant
What are the most effective strategies to prevent postoperative delirium in high-risk surgical patients?