Lumbar disc herniation (LDH) is a common spinal condition characterized by the displacement of disc material that can compress adjacent nerve roots, causing significant lower back and leg pain. When conservative treatments fail, surgical intervention—typically microdiscectomy—is often required. However, despite the minimally invasive nature of this procedure, patients frequently experience severe postoperative pain and postoperative nausea and vomiting (PONV), both of which can delay recovery and reduce patient satisfaction.
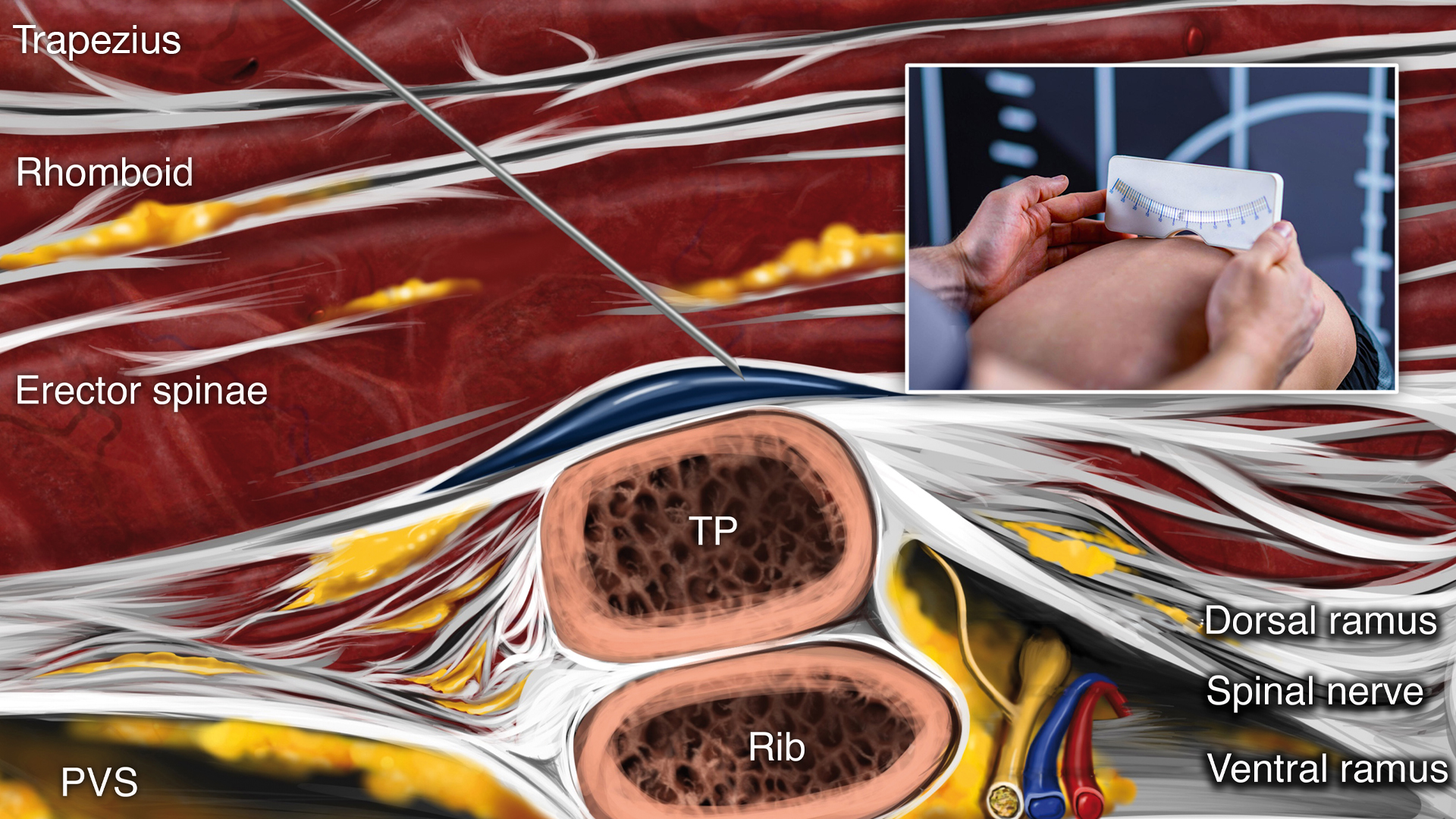
Postoperative pain is known to increase the incidence of PONV, and the reliance on opioids for pain control further exacerbates this risk. The erector spinae plane (ESP) block has emerged as a promising regional anesthesia technique that targets the dorsal rami of spinal nerves to provide analgesia without the systemic side effects of opioids. While the ESP block has demonstrated effectiveness in various surgical contexts, its impact on PONV, particularly in spinal surgery, has not been thoroughly investigated.
A new study published in Regional Anesthesia & Pain Medicine aimed to fill this gap by evaluating the effect of the ESP block on PONV in patients undergoing single-level LDH surgery. The study also explored associated outcomes such as intraoperative opioid use, pain intensity, and the need for rescue analgesics and antiemetics.
Study objective and methods
The primary objective of this randomized, double-blind, controlled trial was to determine whether the ESP block could reduce the incidence of PONV in patients undergoing elective LDH surgery under general anesthesia. Secondary objectives included assessing postoperative pain levels, the use of rescue medications, and exploring the correlation between pain and nausea severity.
The study enrolled 92 patients classified as American Society of Anesthesiologists (ASA) physical status I–II. Participants were randomly divided into two groups:
- ESP group (Group E): Received bilateral ESP block with 0.25% bupivacaine (20 mL per side) prior to surgical incision.
- Control group (Group C): Received a sham block using saline (20 mL per side).
Both groups underwent standardized general anesthesia protocols and received identical postoperative analgesia, including scheduled intravenous paracetamol and tramadol. Ondansetron was administered as prophylaxis for PONV. Assessments were made at 0, 2, 4, 12, and 24 hours postoperatively. PONV was defined as nausea with a Numerical Rating Scale (NRS) score ≥ 4, any vomiting episode, or the need for rescue antiemetic medication.
Key findings
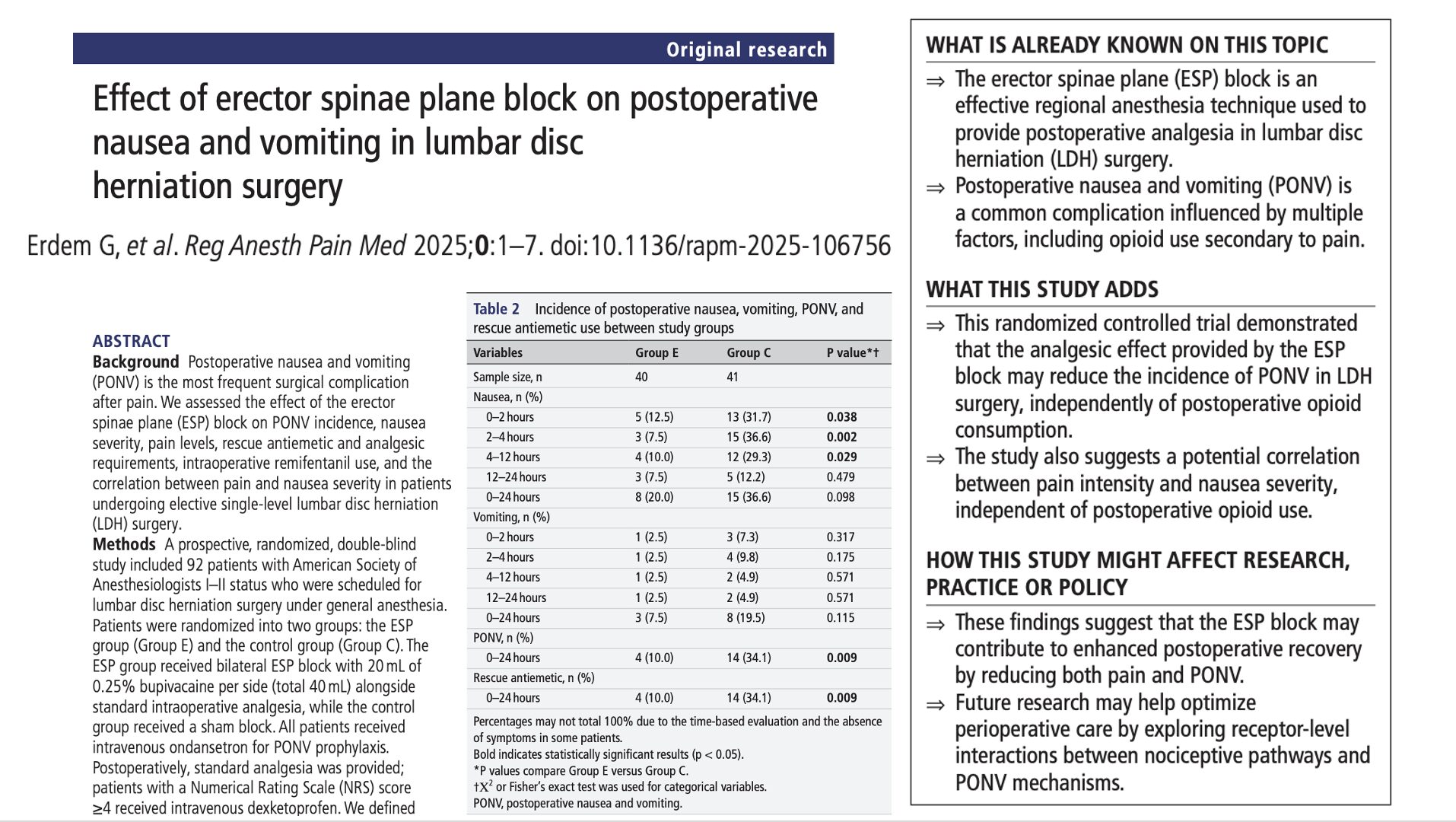
Out of 92 randomized patients, 81 completed the study (40 in Group E and 41 in Group C). The data revealed significant differences between the groups in several outcome measures:
PONV incidence: The ESP group had a markedly lower PONV rate over 24 hours (10%) compared to the control group (34.1%, p = 0.009). Rescue antiemetic use followed the same pattern (10% in Group E vs. 34.1% in Group C, p=0.009).
Nausea severity: Nausea was significantly less frequent in the ESP group during the early postoperative period:
- 0–2 hours: 12.5% in Group E vs. 31.7% in Group C (p = 0.038)
- 2–4 hours: 7.5% vs. 36.6% (p = 0.002)
- 4–12 hours: 10% vs. 29.3% (p = 0.029)
Pain control: The ESP group reported significantly lower pain scores at:
- 0–2 hours (median NRS 1 vs. 2, p < 0.001)
- 2–4 hours (NRS 2 vs. 3, p < 0.001)
- 4–12 hours (NRS 2 vs. 3, p = 0.030)
Rescue analgesic use: Fewer patients in Group E required additional pain relief over 24 hours (25%) compared to Group C (68.3%, p < 0.001).
Intraoperative opioid use: Median remifentanil consumption was significantly lower in Group E (350 µg vs. 640 µg, p < 0.001), indicating effective analgesia from the ESP block.
Pain-nausea correlation: Strong and statistically significant correlations were found between pain intensity and nausea severity:
- 0–2 hours: r = 0.738 (p < 0.001)
- 2–4 hours: r = 0.432 (p < 0.001)
- 4–12 hours: r = 0.465 (p < 0.001)
- 12–24 hours: r = 0.327 (p = 0.003)
These findings underscore the interconnected nature of pain and PONV and suggest that improving one may beneficially impact the other.
Conclusion
The study confirms the clinical utility of the ESP block in managing postoperative complications following lumbar discectomy. By significantly reducing both pain intensity and PONV incidence, the ESP block not only improves patient comfort but also contributes to faster recovery and potentially lower healthcare costs through reduced need for medications and shorter hospital stays.
Importantly, these benefits were achieved with a single preoperative injection, highlighting the ESP block’s practicality in routine surgical care. Unlike many strategies that target PONV or pain separately, the ESP block offers a dual advantage, potentially mediated through shared neurochemical pathways involving 5-HT3 and NK1 receptors.
Future research
While the results are promising, they also pave the way for further investigation:
- Mechanistic studies: Future trials should explore how ESP block affects serotonin and neurokinin receptor pathways involved in both pain and PONV. Animal studies and receptor-specific antagonist trials may help unravel these interactions.
- Extended outcome monitoring: Since the study focused on a 24-hour postoperative window, additional research is needed to assess long-term effects of ESP block on chronic pain, delayed PONV, and functional recovery.
- Comparative effectiveness studies: Trials comparing ESP block with other regional anesthesia techniques (e.g., quadratus lumborum block or paravertebral block) may further refine perioperative pain strategies in spinal surgery.
- Patient subgroups: Sub-analysis by patient characteristics such as age, sex, BMI, and prior opioid use history could help identify populations that would benefit most from ESP block.
In conclusion, this trial strengthens the evidence base for incorporating the ESP block into multimodal analgesic and antiemetic protocols in lumbar disc surgery. Its simplicity, efficacy, and safety profile make it an appealing choice for anesthesiologists seeking to improve patient recovery while minimizing opioid use and its associated complications.
For more detailed information, refer to the full article in RAPM.
Erdem G. et al. Effect of erector spinae plane block on postoperative nausea and vomiting in lumbar disc herniation surgery. Reg Anesth Pain Med. Published online June 30, 2025.
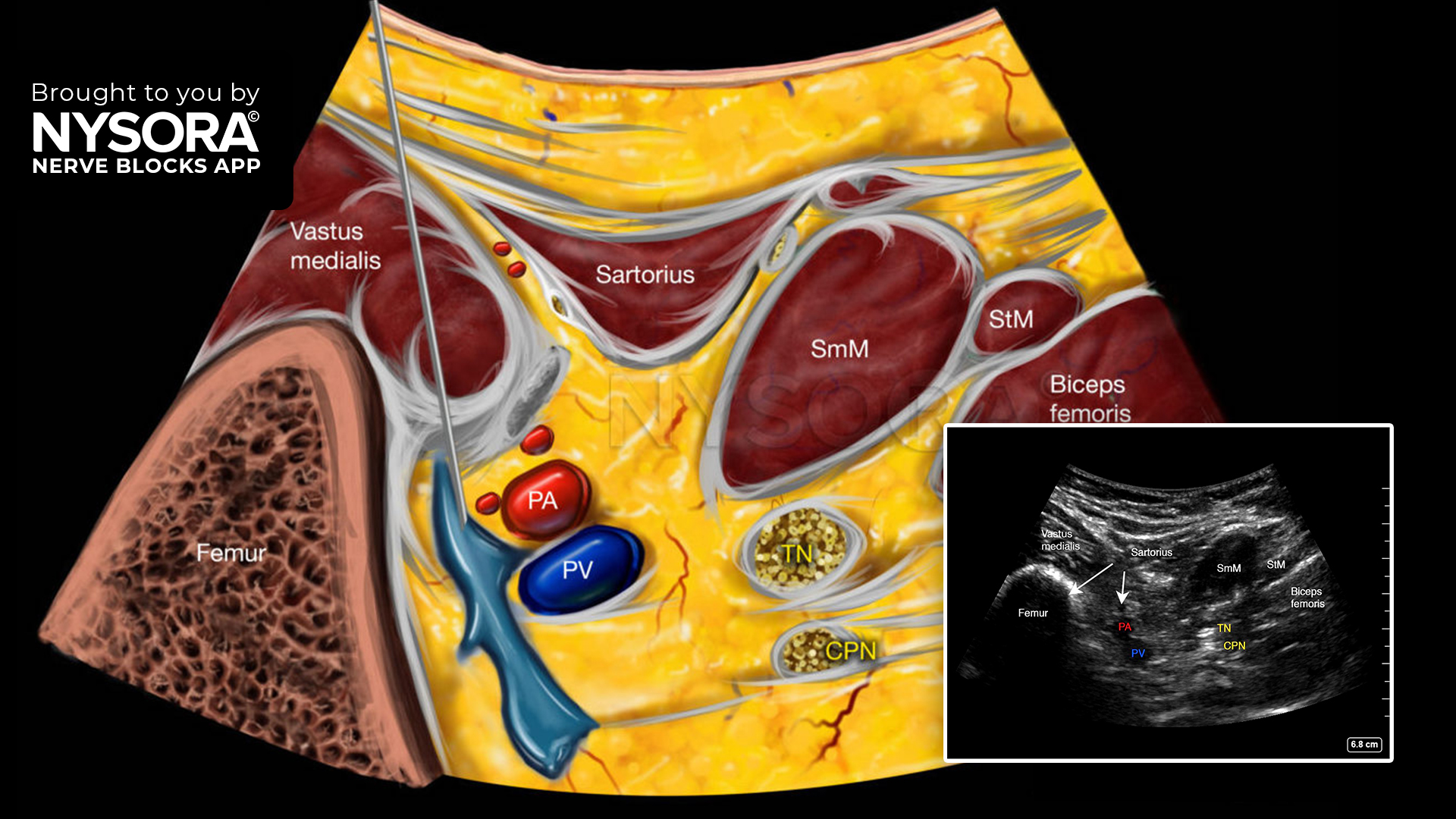
Download the Nerve Blocks App HERE for in-depth insights on the erector spinae plane block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!