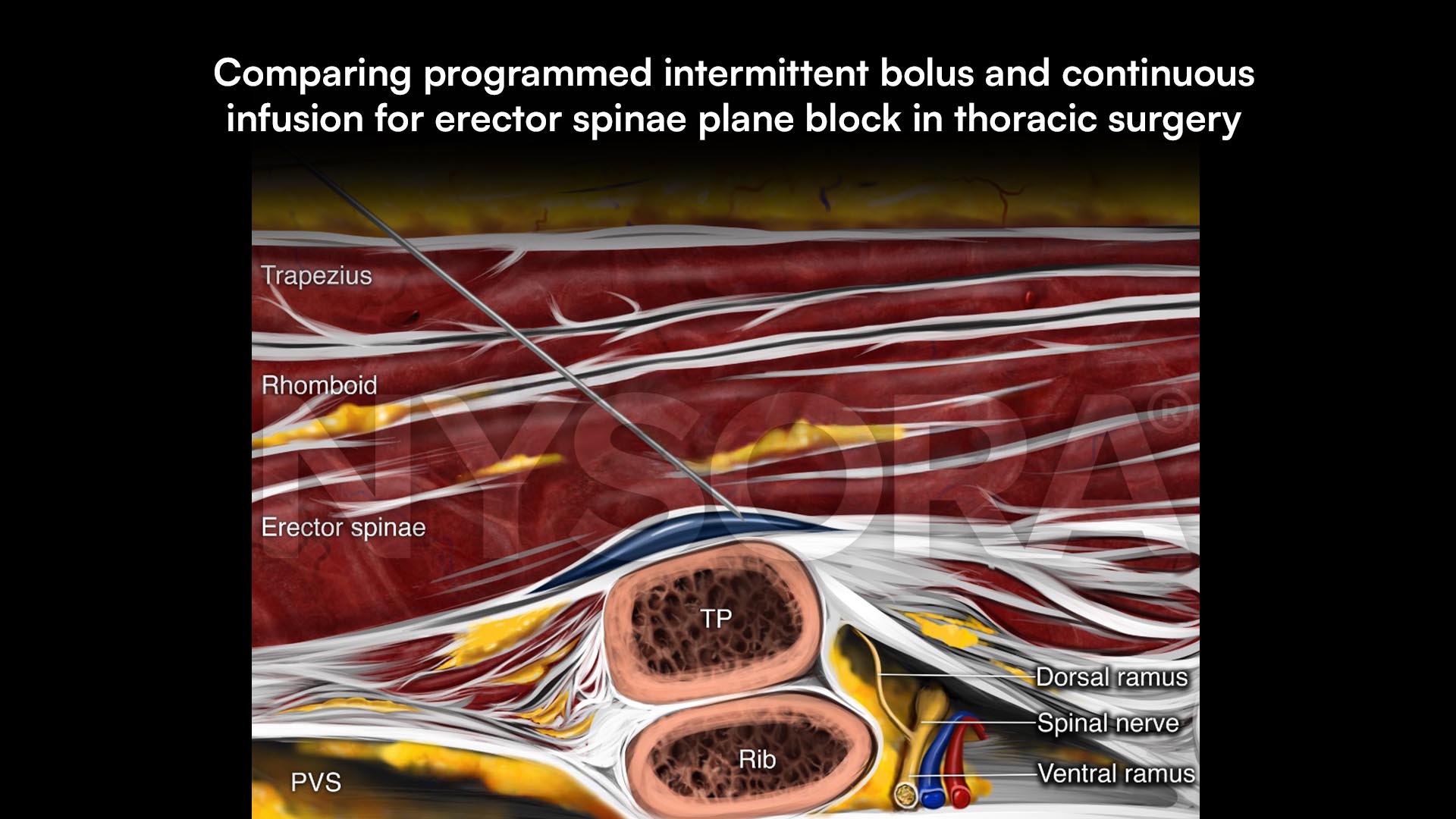
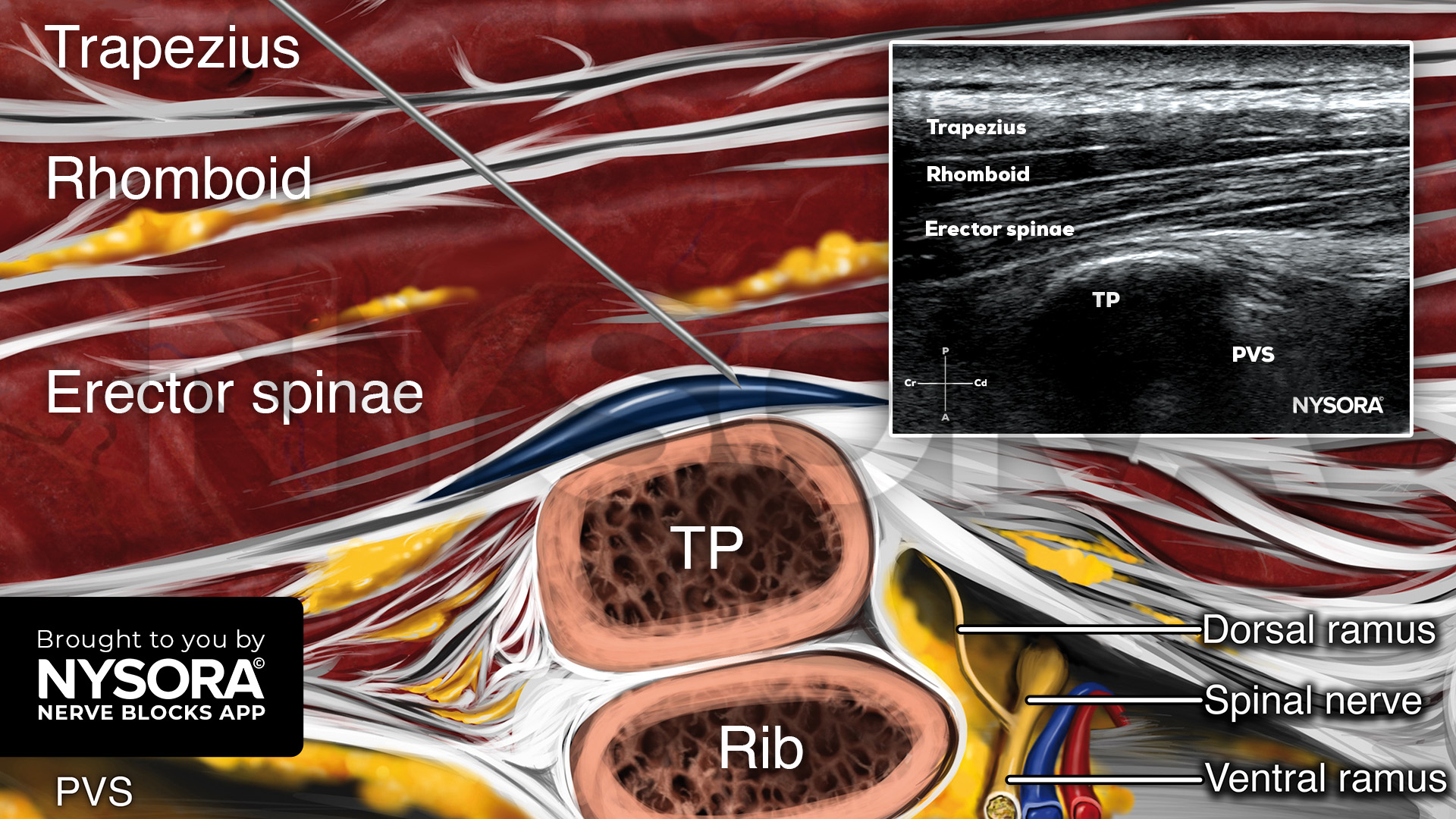
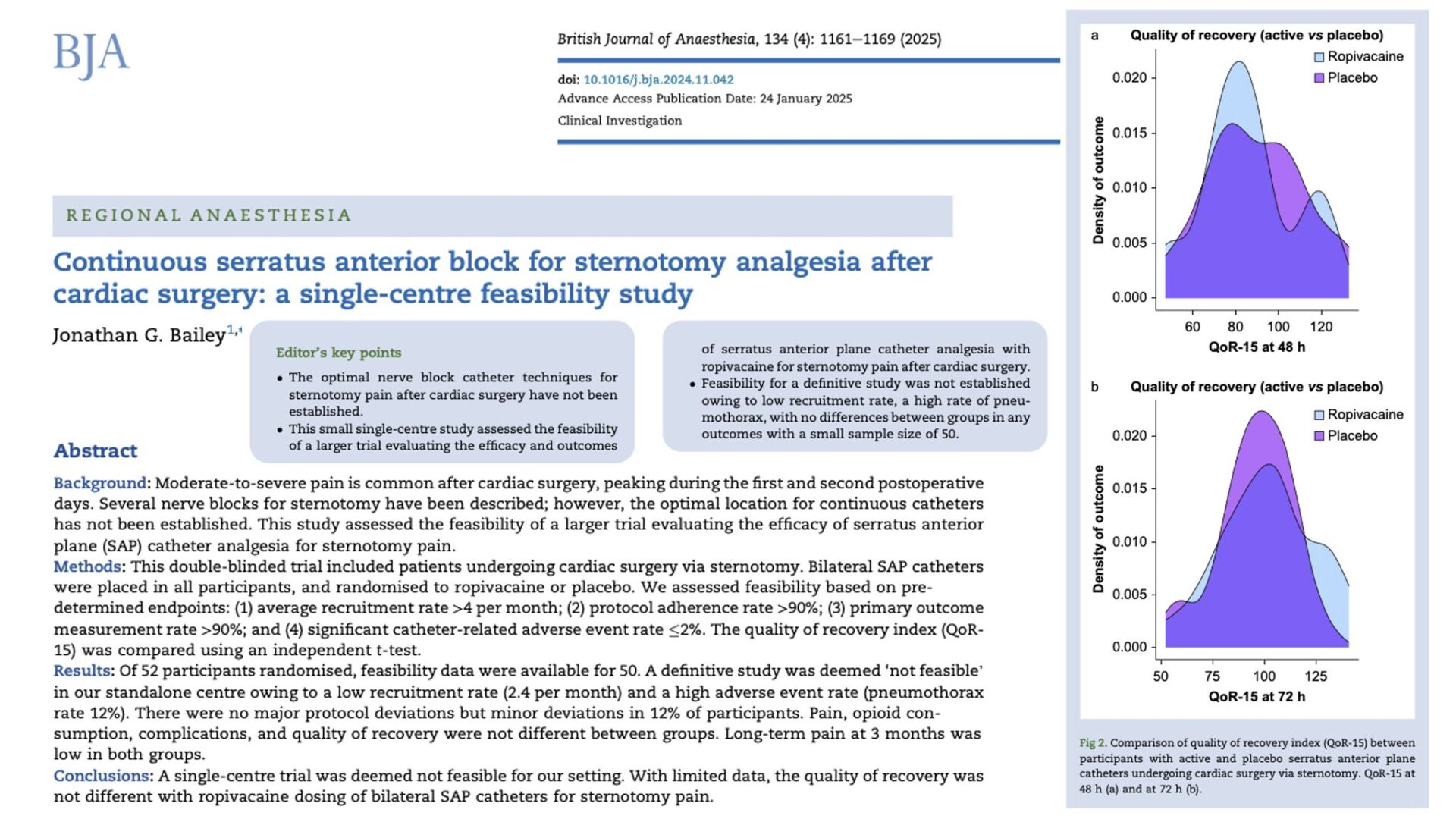
Effective pain management is essential after thoracoscopic surgeries, which are minimally invasive yet often associated with significant postoperative discomfort. The erector spinae plane (ESP) block has emerged as a promising regional anesthesia technique. This study investigates whether a programmed intermittent bolus (PIB) delivery system for ESP block offers better recovery and pain management compared to a continuous infusion (CI) method in thoracoscopic surgery patients.
Study objective and methods
The primary objective was to evaluate whether the PIB method for administering an ESP block offers superior recovery quality compared to CI in patients undergoing video-assisted thoracoscopic surgery (VATS). Conducted as a single-center, randomized, double-blind, controlled trial, the study included 60 participants randomized into two groups: 28 patients analyzed in the PIB group and 27 in the CI group.
- PIB group: Received levobupivacaine (0.125%) delivered as 20 mL boluses every 2 hours.
- CI group: Received levobupivacaine (0.125%) at a continuous rate of 10 mL per hour.
The primary outcome was the Quality of Recovery-15 (QoR-15) score at 24 hours post-surgery, assessing overall recovery experience. Secondary outcomes included pain scores at rest and during deep inspiration, opioid consumption, incidence of nausea and vomiting, and additional recovery metrics. This comprehensive approach aimed to identify differences in recovery quality and pain management between the two delivery methods.
Key findings
- Quality of recovery: QoR-15 scores were similar between groups: PIB (median 115.5 [IQR 107–125]) vs. CI (median 110 [IQR 93–128], P = 0.29). Nausea and vomiting were less common in the PIB group, with 14% requiring antiemetics compared to 41% in the CI group (P = 0.04).
- Pain scores: Pain scores at rest and during deep inspiration were comparable between groups: PIB (rest: mean 3.2 ± 2.5, inspiration: mean 5.9 ± 2.3) vs. CI (rest: mean 3.0 ± 2.6, inspiration: mean 5.1 ± 2.9).
- Opioid consumption: Rescue opioid use was similar, with the PIB group consuming a median of 53 mg (IQR 22.5–88.75) and the CI group 33.5 mg (IQR 15–53) over 24 hours (P = 0.06).
- Other metrics: No significant differences in inspiratory volume recovery, time to mobilization, or length of hospital stay.
Conclusion
The study found no significant differences in overall recovery quality or pain control between PIB and CI for ESP block delivery after VATS. However, the reduced incidence of nausea and vomiting in the PIB group highlights a potential benefit. The results suggest that the delivery method (PIB vs. CI) may be less important than the total volume and dose of local anesthetic used.
Future research
Future research should explore optimizing the delivery method of ESP blocks, focusing on patient subgroups who may benefit from specific techniques. Larger multicenter trials are needed to confirm findings and assess long-term recovery outcomes, including chronic pain prevention and functional mobility improvements.
For more detailed information, refer to the full article in BJA.
Eochagain AN, Moorthy A, Shaker J, et al. Programmed intermittent bolus versus continuous infusion for catheter-based erector spinae plane block on quality of recovery in thoracoscopic surgery: a single-centre randomised controlled trial. Br J Anaesth. 2024;133(4):874-881.
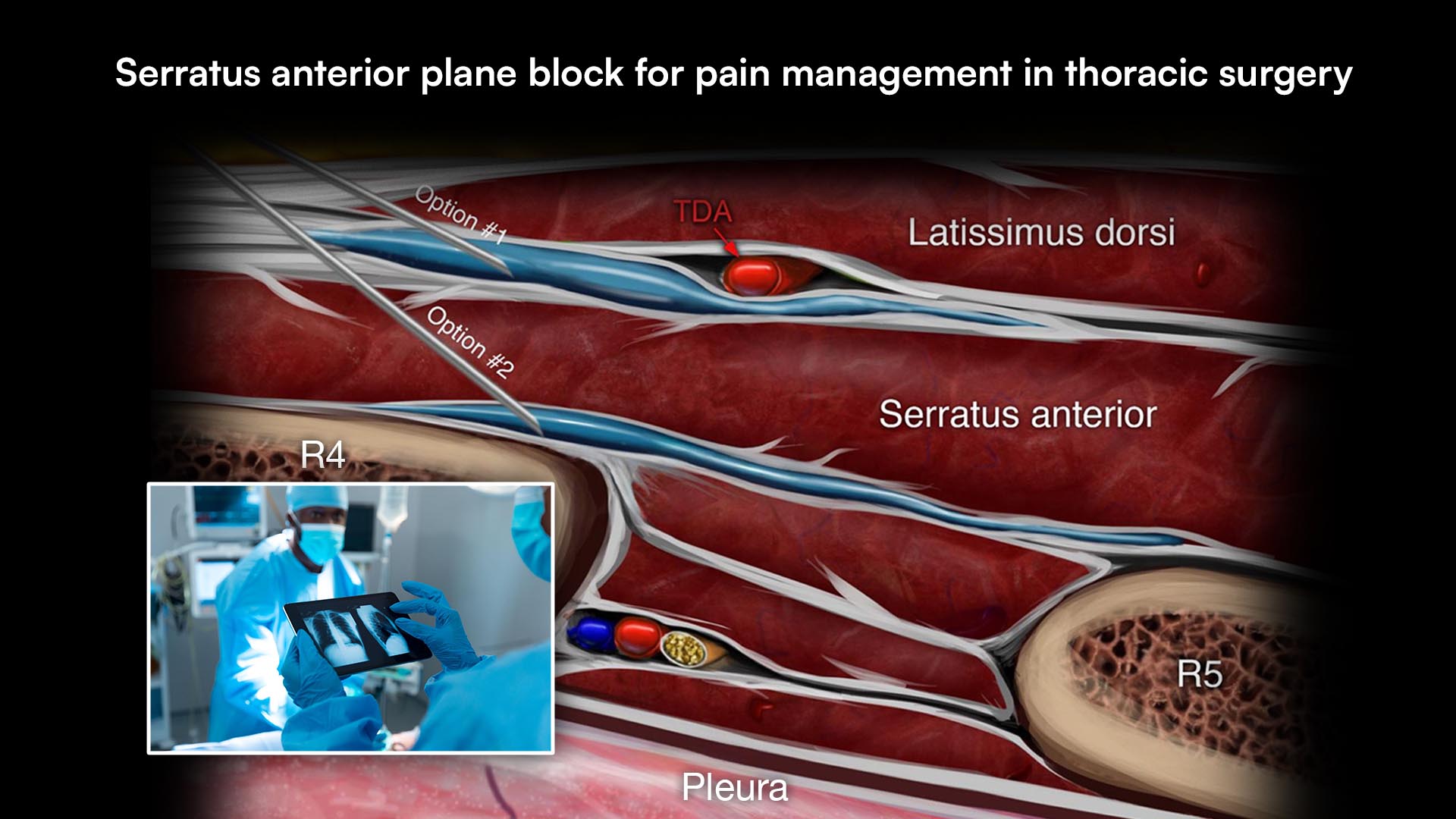
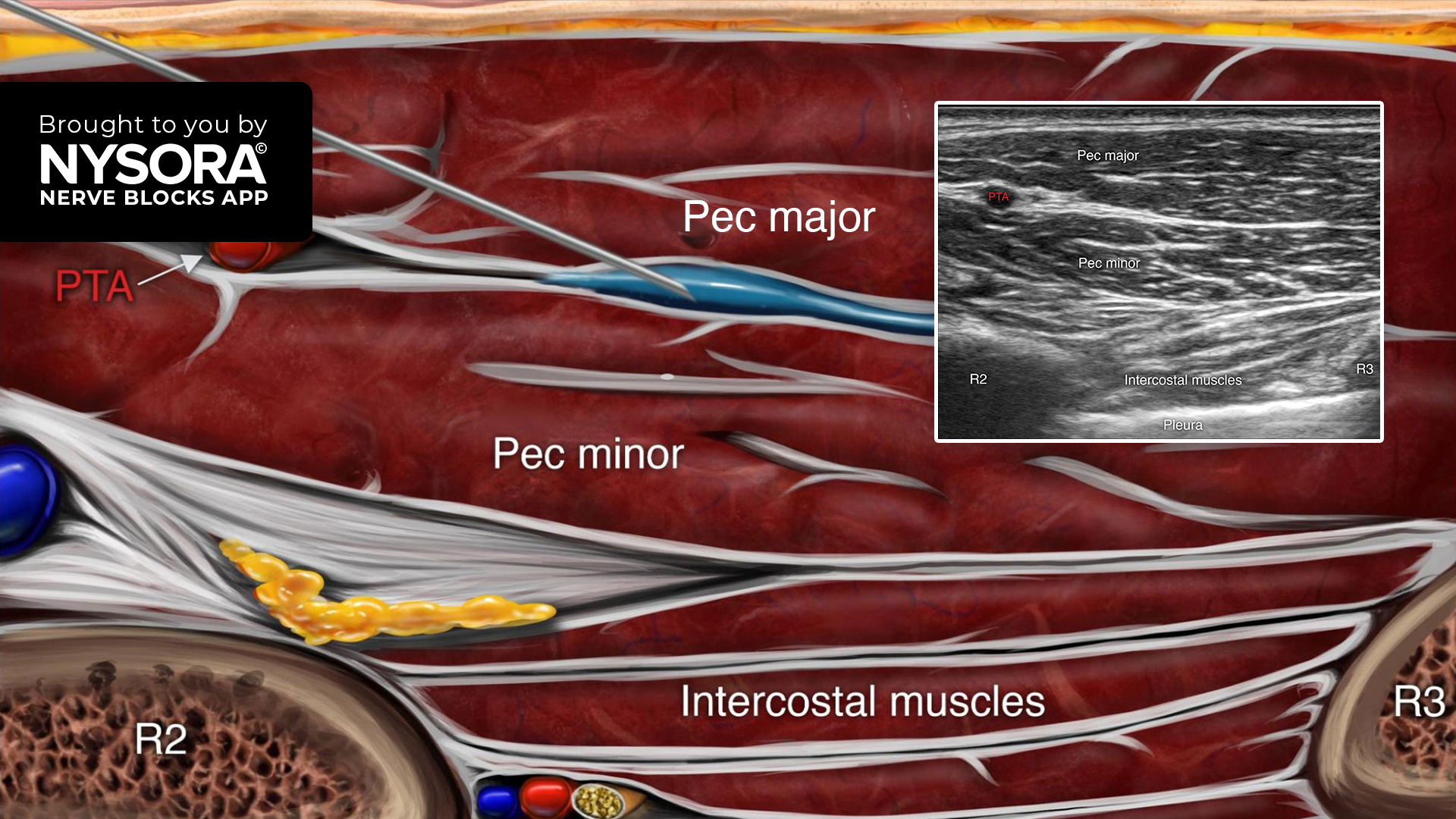
Download the Nerve Blocks App HERE for in-depth insights on the erector spinae plane block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Blocks Manual Course on NYSORA’s LMS!