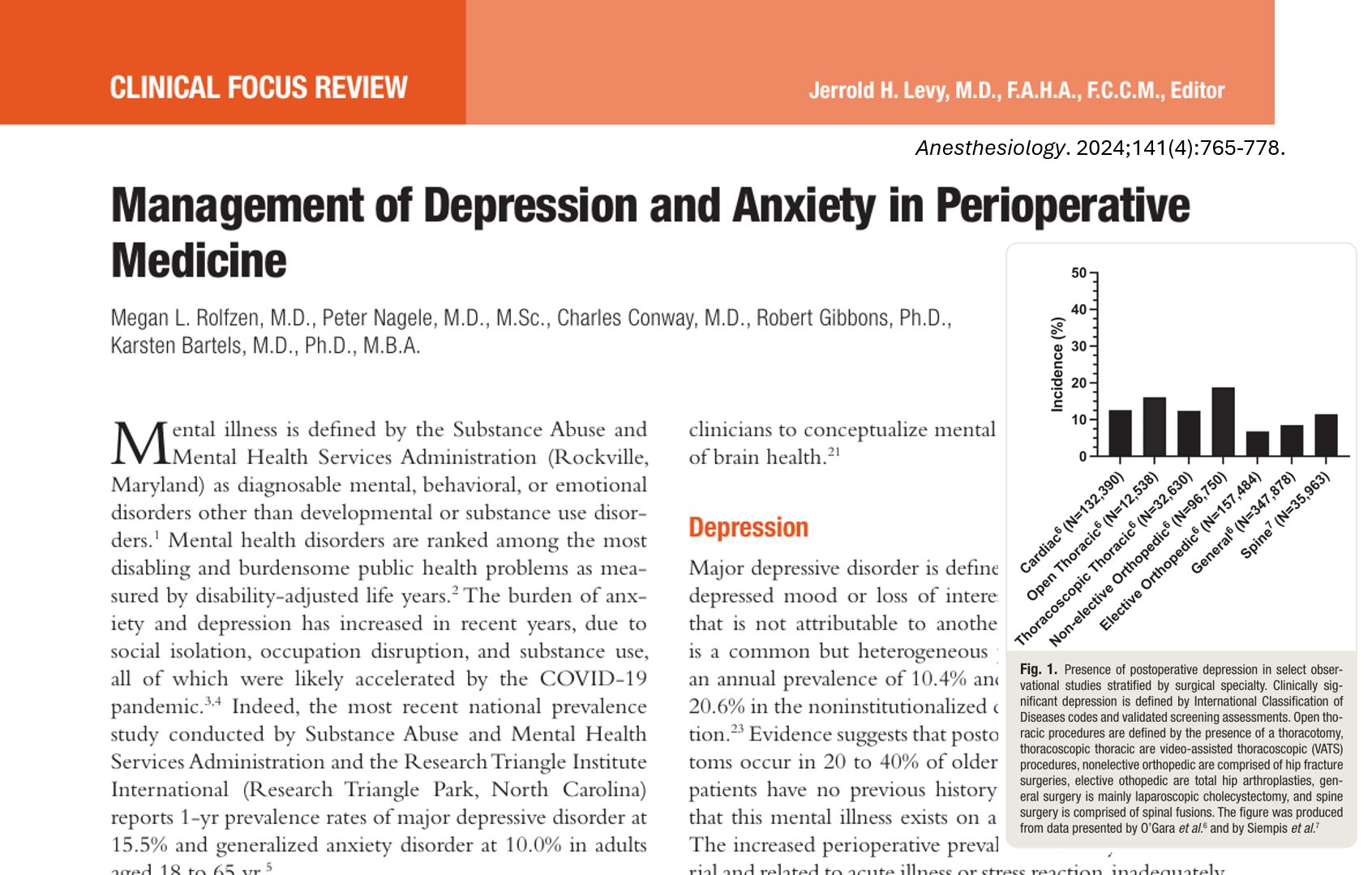
In a major effort to refine and enhance postoperative pain management strategies, a new systematic review and meta-analysis by Maagaard et al. 2025 provides crucial insights into the synergistic use of two pharmacologic agents—dexamethasone and dexmedetomidine—as adjuncts in peripheral nerve blocks. This study determined whether combining these agents offers superior analgesia duration and clinical outcomes compared to using them alone or in standard practice settings
Rationale and clinical relevance
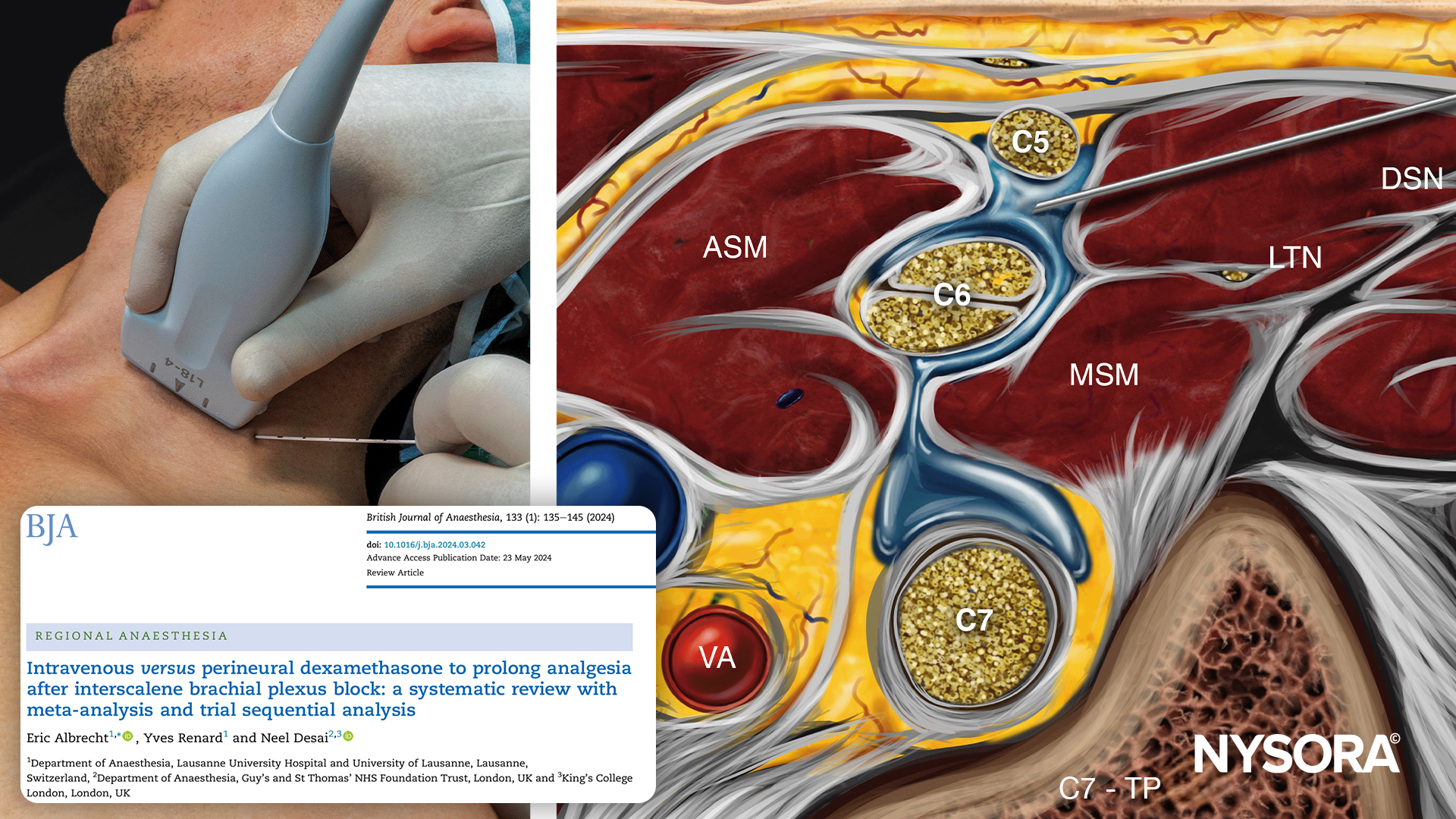
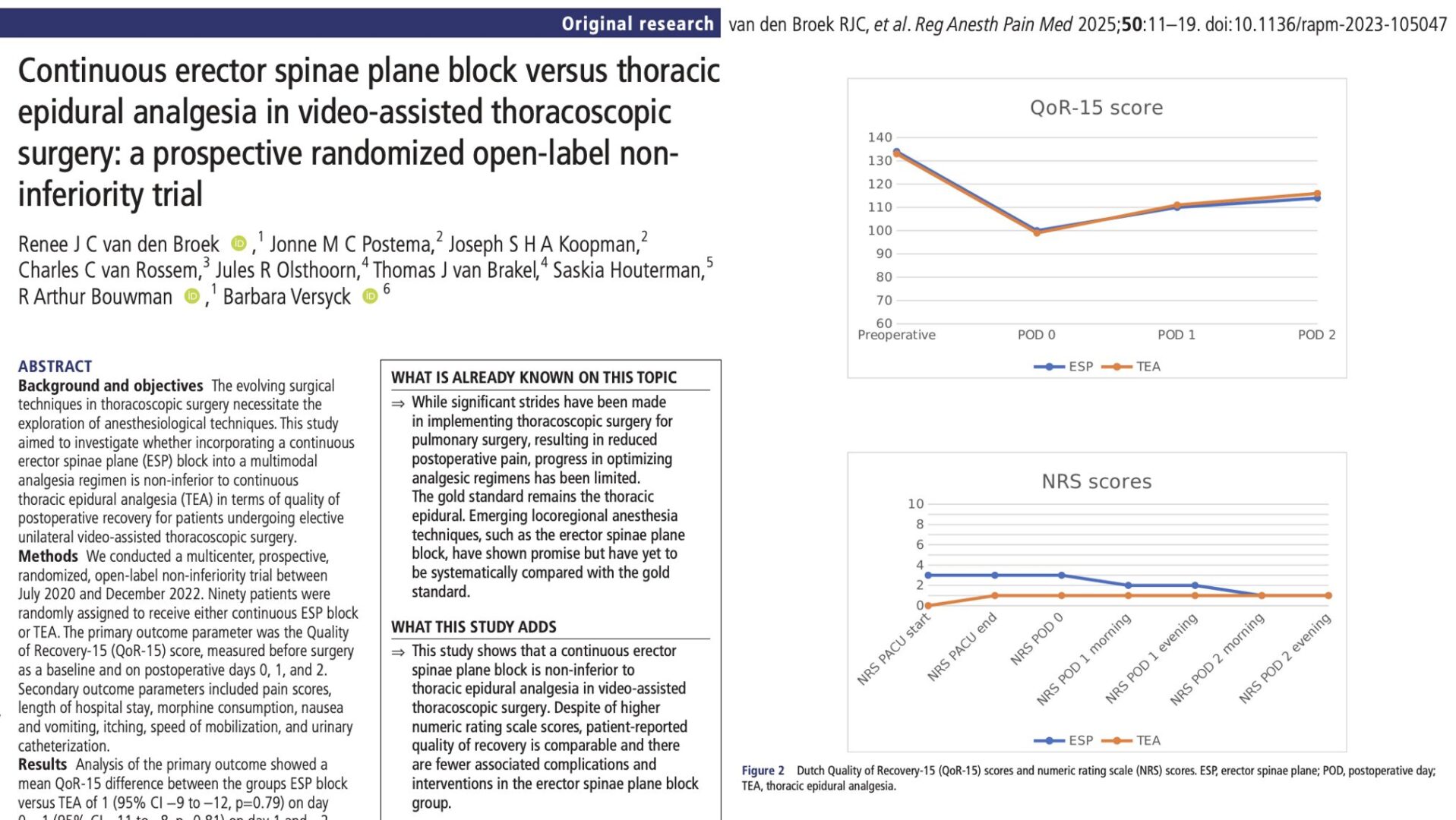
Peripheral nerve blocks are cornerstone interventions in regional anesthesia, widely utilized to provide site-specific analgesia during and after surgical procedures. However, a common limitation remains: the duration of the block is finite, often waning before the peak period of postoperative pain subsides. To address this issue, adjuvants like dexamethasone and dexmedetomidine are frequently added to local anesthetics to prolong their effects. While both agents have independently demonstrated efficacy, clinical equipoise persists around their combined use. Could combining them provide additive or even synergistic benefits? This systematic review addresses that critical question, offering high-level evidence to guide best practices in anesthesia.
Dexamethasone
- Mechanism: Glucocorticoid that reduces inflammation and inhibits nociceptive signal transduction via genomic and non-genomic pathways.
- Effect on nerve blocks: Enhances and prolongs analgesic effects, potentially via inhibition of prostaglandin synthesis and suppression of ectopic neuronal discharge.
- Preferred route: Intravenous (perineural use remains off-label).
Dexmedetomidine
- Mechanism: Selective α2-adrenergic receptor agonist that produces sedation, analgesia, and anxiolysis by inhibiting norepinephrine release.
- Effect on nerve blocks: Prolongs duration and reduces onset time of sensory and motor blockade.
- Preferred route: Both intravenous and perineural routes have been explored, with varying systemic vs. local efficacy outcomes.
The combination aims to harness both anti-inflammatory and neuroinhibitory mechanisms, theoretically providing extended and robust pain control.
Study design and methods
The systematic review included data from 9 randomized controlled trials published between 2019 and 2023, involving a total of 1023 participants across 14 direct comparisons.
Inclusion criteria:
- Adults ≥18 years undergoing surgery with peripheral nerve block.
- At least one study group received a combination of dexamethasone and dexmedetomidine.
Comparators included placebo, dexamethasone alone, or dexmedetomidine alone.
Outcomes measured:
- Primary outcome: Duration of analgesia (time to first pain or analgesic request).
- Secondary outcomes: Motor and sensory block duration, opioid use at 24/48/72 hours, adverse events (AEs and SAEs), pain scores.
Advanced analytical techniques, including trial sequential analysis (TSA) and GRADE certainty assessments, were employed to evaluate the strength and sufficiency of evidence. Subgroup and sensitivity analyses further bolstered the findings.
Key findings
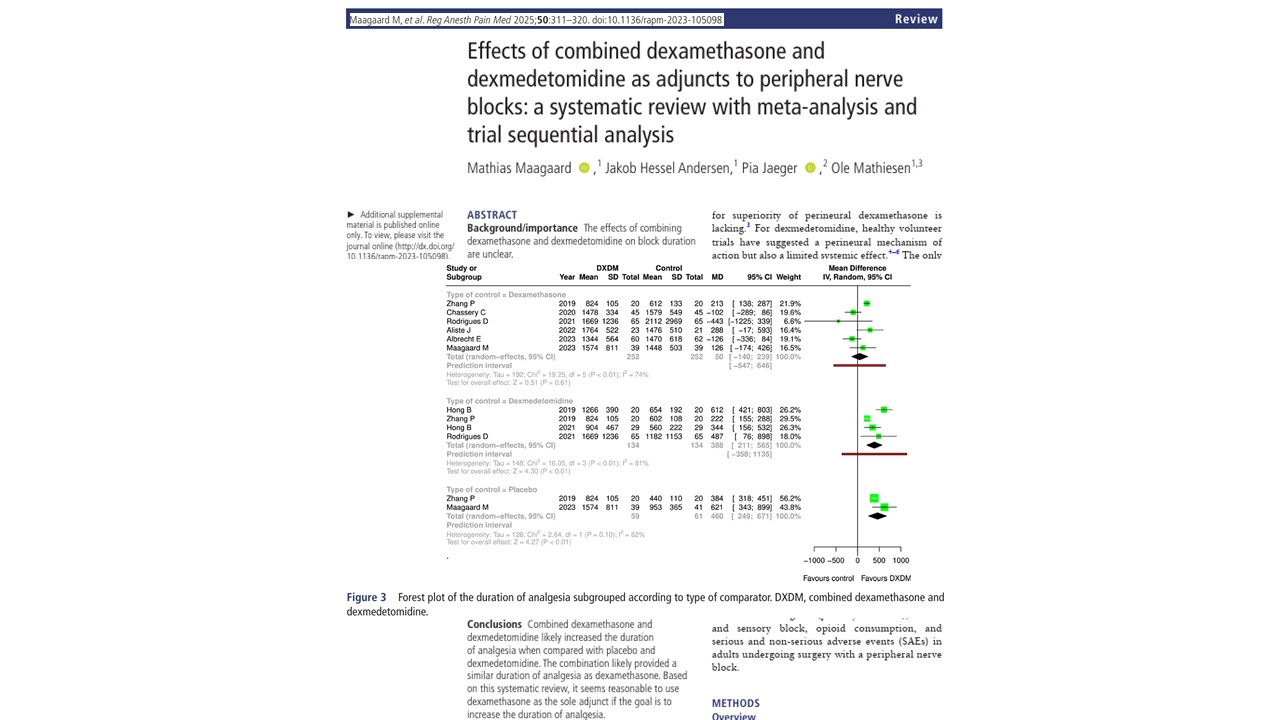
Prolongation of analgesia
The most consistent and statistically robust outcome was an increased analgesia duration when the combination was compared to:
- Placebo: +460 minutes (95% CI 249 to 671)
- Dexmedetomidine: +388 minutes (95% CI 211 to 565)
No meaningful advantage over dexamethasone
Compared to dexamethasone alone, the combination yielded:
- Mean difference: +50 minutes (95% CI −140 to 239)
- Conclusion: No clinically relevant benefit
This finding is pivotal: Dexamethasone alone produced prolonged block durations comparable to the combination.
Motor and sensory block durations
- Motor block: modest prolongation over placebo, but not over other agents
- Sensory block: inconsistent findings; no definitive superiority of the combination
These results suggest that while some prolongation occurs, it’s not markedly different than single-agent dexamethasone.
Opioid consumption and pain scores
- 24-hour opioid use: Lower in the combination group vs. placebo and dexmedetomidine, but not versus dexamethasone.
- Pain scores (24–72h): Small and likely clinically insignificant reductions (0.5 to 1.3 points on a 10-point scale).
While opioid-sparing effects are desirable, the evidence does not show that combining the agents adds any clear benefit beyond what dexamethasone already achieves.
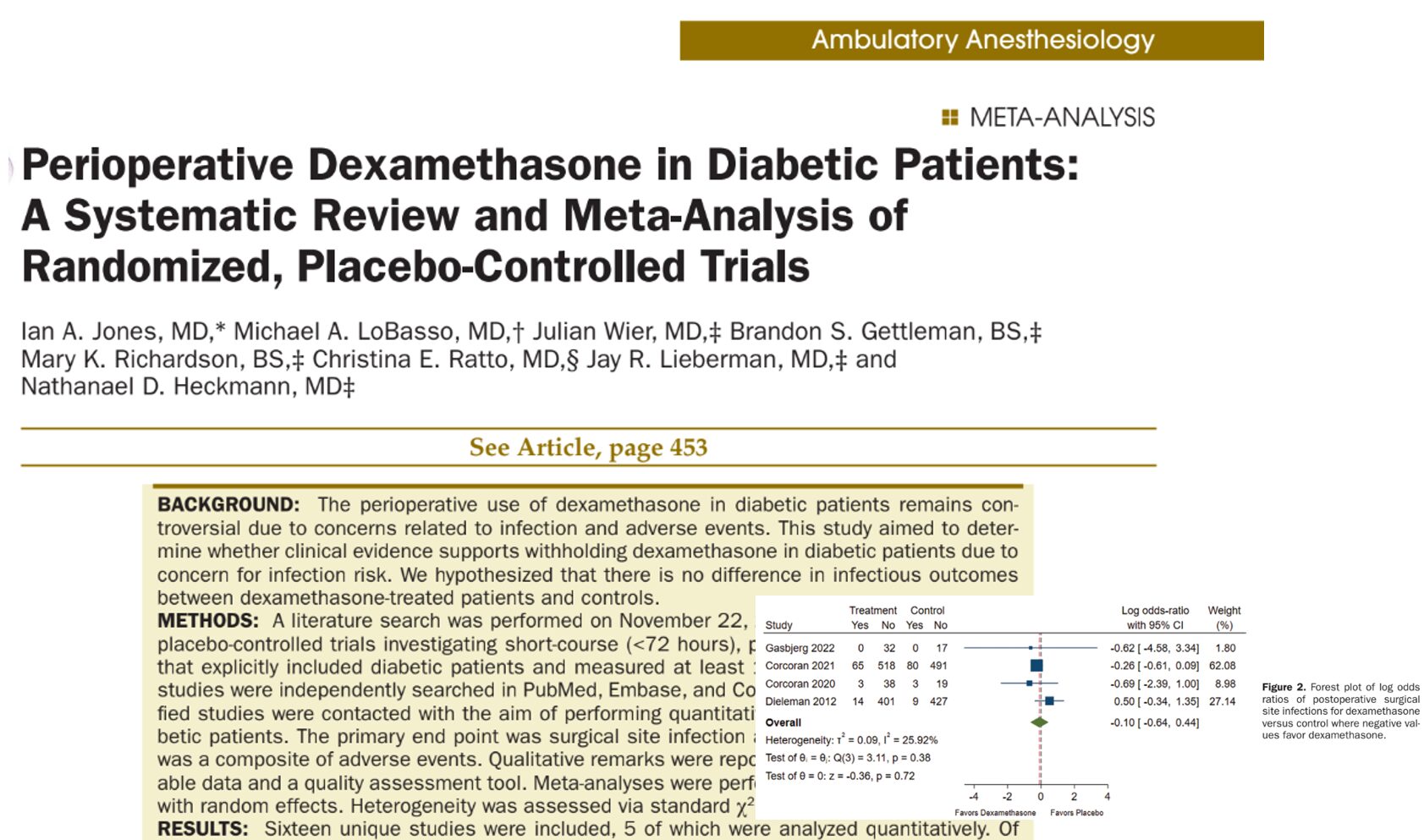
Safety and adverse events
Serious adverse events (SAEs)
- Extremely rare; no concerning trends observed.
- The combination group had no SAEs, while isolated SAEs in the comparator groups were unrelated to the intervention.
Non-serious adverse events
- Occurrence rates were similar across groups.
- No significant increase in nausea, bradycardia, or sedation in the combination group.
The combination appears well tolerated, but larger trials are needed for firm conclusions due to small sample sizes.
Subgroup and sensitivity analyses
To test the robustness of findings, subgroup analyses were examined:
- Surgical location (upper vs. lower extremity)
- Block site (interscalene, infraclavicular, popliteal)
- Adjuvant dosing and administration route
No subgroup showed consistent or significant deviation from the core findings. Moreover, leave-one-out and best/worst-case sensitivity tests upheld the primary outcomes, affirming the reliability of the conclusions.
Implications for clinical practice
Key takeaways:
- Dexamethasone remains the superior single-agent adjuvant for prolonging nerve block analgesia.
- Combining it with dexmedetomidine does not provide additional benefit substantial enough to justify routine use.
- Dexmedetomidine alone is inferior to dexamethasone or the combination, and may not warrant use if prolongation is the sole aim.
- Given the off-label status of perineural dexamethasone, intravenous administration remains the recommended route (dose: 0.1–0.2 mg/kg).
These findings align with current clinical guidelines and underscore the need to critically evaluate novel combinations, particularly when they increase cost, complexity, or risk.
Limitations and caveats
Despite its strength, the review is not without limitations:
- High risk of bias in several trials.
- Variability in dosing regimens and block definitions.
- Lack of uniform outcome measurement, with subjective metrics like “time to first pain”.
- Insufficient power to detect rare but serious adverse events.
Standardization in future trials, especially regarding objective pain assessments and block verification methods, is critical for advancing this field.
Future research
- Larger RCTs to assess long-term safety and recovery quality
- Comparative effectiveness research across other adjuncts like clonidine, magnesium, or midazolam
- Network meta-analyses to elucidate relative rankings of all available adjuvants
- Patient-centered outcomes, such as satisfaction, return to function, and quality of recovery
The ultimate goal should be a personalized approach to regional anesthesia, where adjuncts are tailored to patient risk profiles and surgical needs.
Conclusion
This definitive review affirms that while dexamethasone and dexmedetomidine can be safely used in combination, there is no added advantage over dexamethasone alone for prolonging peripheral nerve block analgesia. Clinicians should confidently use dexamethasone as the first-line adjuvant and remain judicious about layering additional agents without strong supporting evidence. With increasing emphasis on value-based care, these findings encourage smarter, evidence-based decisions prioritizing efficacy, safety, and cost-effectiveness.
For more information, refer to the full article in Regional Anesthesia and Pain Medicine.
Maagaard M, Andersen JH, Jaeger P, Mathiesen O. Effects of combined dexamethasone and dexmedetomidine as adjuncts to peripheral nerve blocks: a systematic review with meta-analysis and trial sequential analysis. Reg Anesth Pain Med. 2025 Apr 10;50(4):311-320.
Read more about adjuvants in the Regional Anesthesia Module on the NYSORA360!