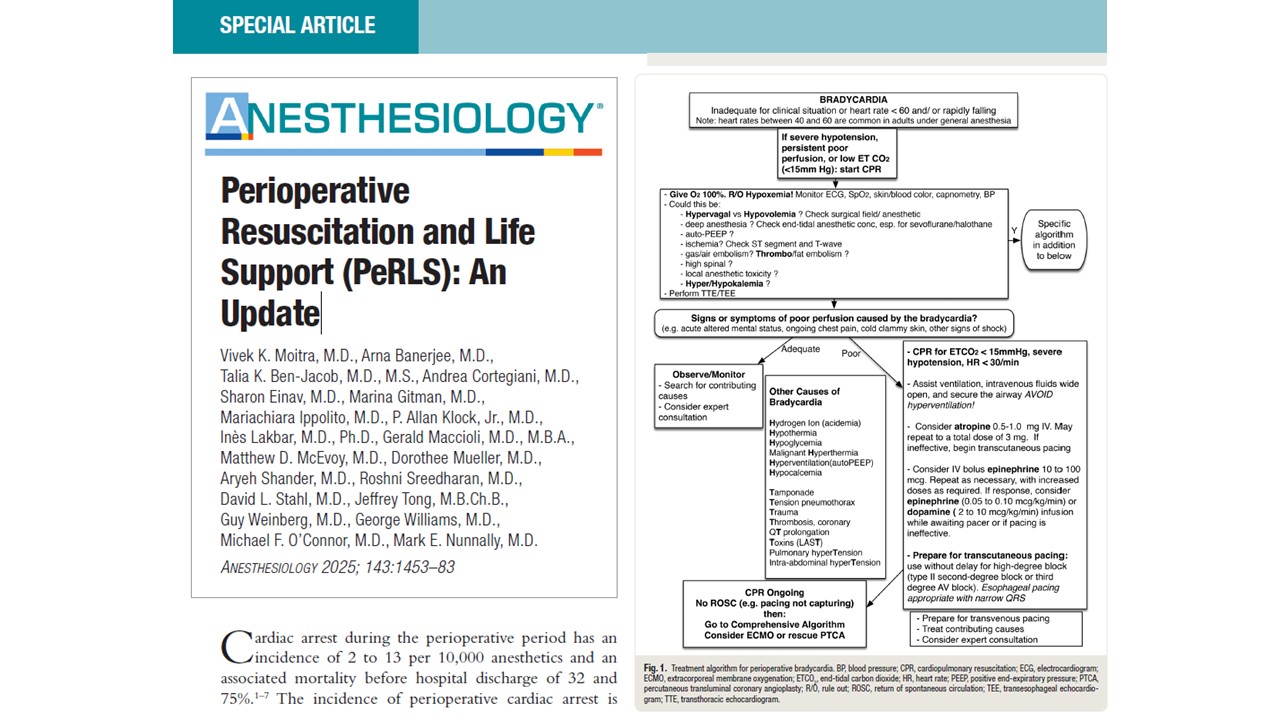
Cardiac arrest during surgery or the perioperative period is a critical event with devastating consequences. Mortality remains exceptionally high, between 56% and 65%, even when conventional advanced cardiovascular life support (ACLS) protocols are promptly applied. One emerging innovation that offers renewed hope is extracorporeal cardiopulmonary resuscitation (ECPR), which uses extracorporeal membrane oxygenation (ECMO) to sustain circulation and oxygenation during cardiac arrest unresponsive to standard resuscitation efforts.
In their May 2024 clinical focus review, Pande et al. (Anesthesiology) present a comprehensive analysis of the role of ECPR in adult perioperative settings. Their findings help anesthesiologists and perioperative physicians navigate this complex, resource-intensive intervention and clarify when and how ECPR can transform a catastrophic arrest into a survivable event.
Why this topic matters
- Conventional CPR fails to achieve adequate organ perfusion in many patients, particularly during prolonged resuscitation.
- ECPR can restore near-normal perfusion, buying time for teams to identify and reverse the underlying cause of arrest.
- The perioperative setting offers unique advantages: witnessed arrests, immediate access to clinicians, and often readily available ECMO resources.
What is extracorporeal CPR?
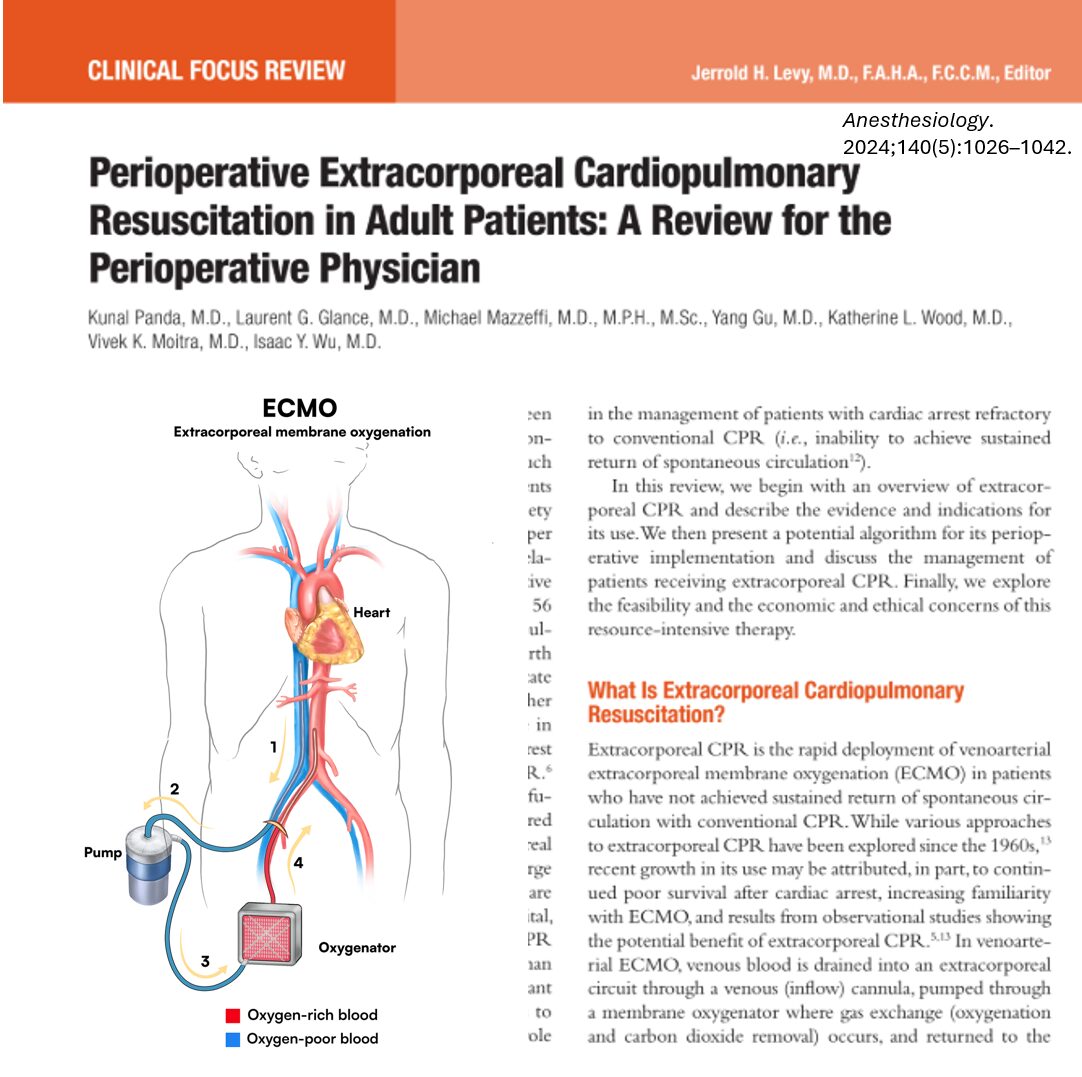
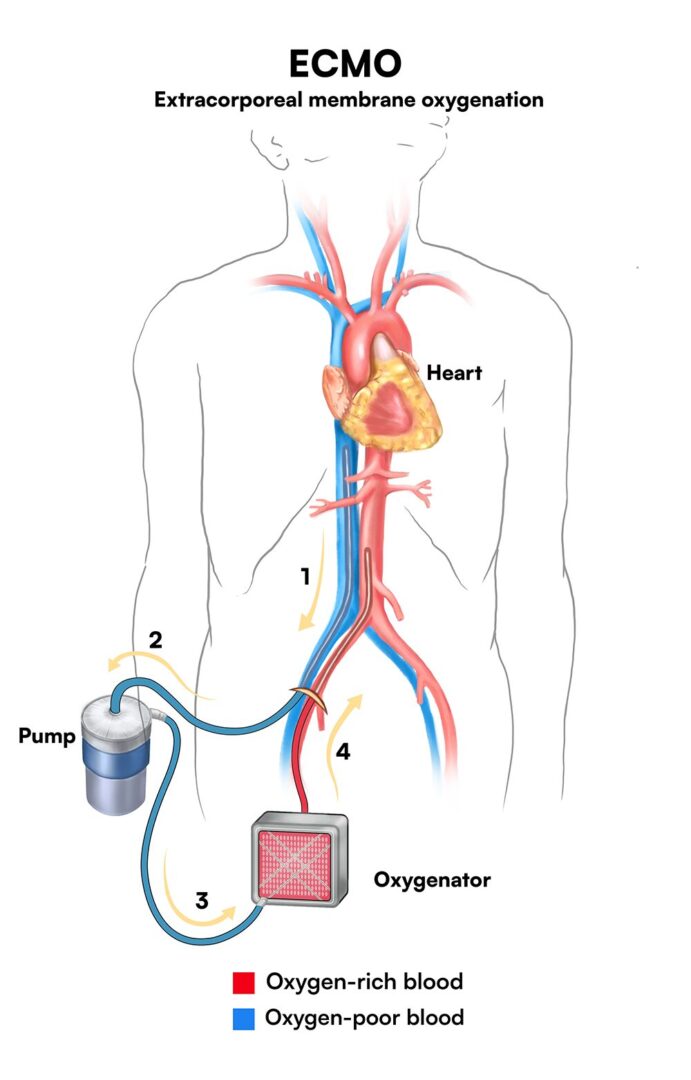
ECPR involves the rapid deployment of venoarterial ECMO during a cardiac arrest when return of spontaneous circulation (ROSC) is not achieved with conventional CPR. This system temporarily:
- Drains venous blood (typically via femoral vein),
- Oxygenates it externally,
- Pumps it back into the arterial circulation (typically via femoral artery),
- Providing continuous oxygenated blood flow to vital organs.
Unlike CPR, which delivers ~25% of normal cardiac output, ECMO can provide full end-organ perfusion, reducing the risk of ischemic brain and organ injury.
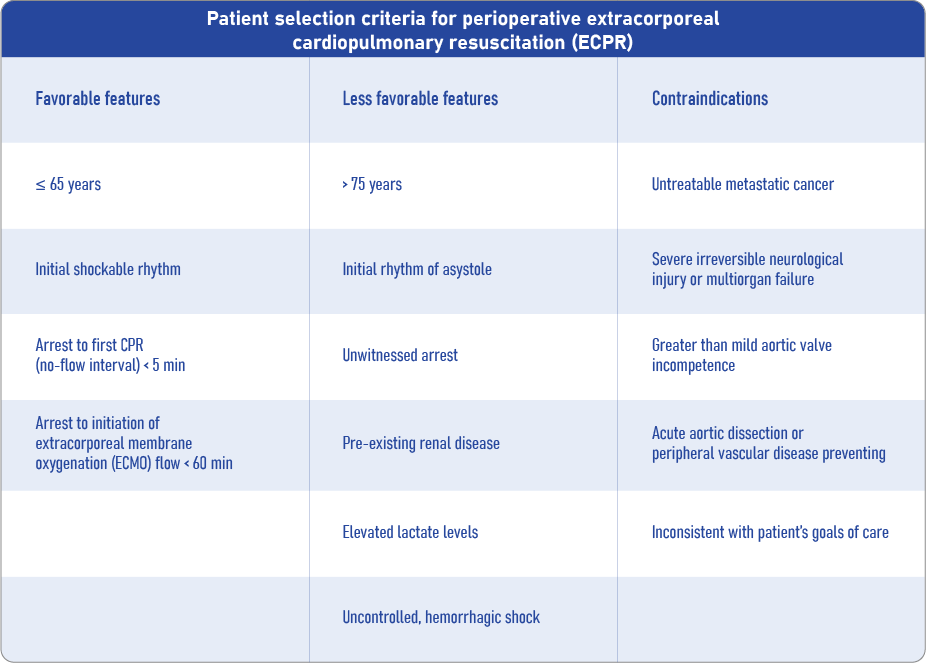
Indications: when to consider ECPR?
ECPR should be considered when the cardiac arrest is witnessed, the cause is potentially reversible, and conventional CPR fails to restore circulation within 10–20 minutes. Key indicators include:
Neurologic viability
- No-flow time < 5 minutes: time from arrest to initiation of CPR.
- Low-flow time < 60 minutes: total time on conventional CPR before ECMO support.
Cardiac rhythm
- Shockable rhythms (ventricular fibrillation, pulseless VT) are associated with better outcomes.
- Asystole or PEA are less favorable but not absolute contraindications if other criteria are met.
Patient characteristics
- Age ≤ 65 offers better survival odds.
- Fewer comorbidities, particularly no severe renal failure or metastatic cancer.
- Lactate < 10 mmol/L is favorable.
- Prearrest functional status should be good.
Step-by-step: implementing perioperative ECPR
-
Anticipation
- Identify high-risk patients preoperatively (e.g., cardiac surgery, severe comorbidities).
- Discuss potential ECMO candidacy during surgical safety briefing.
-
Recognition and ACLS
- Immediately initiate standard ACLS upon recognition of cardiac arrest.
- Ensure high-quality chest compressions and early defibrillation if indicated.
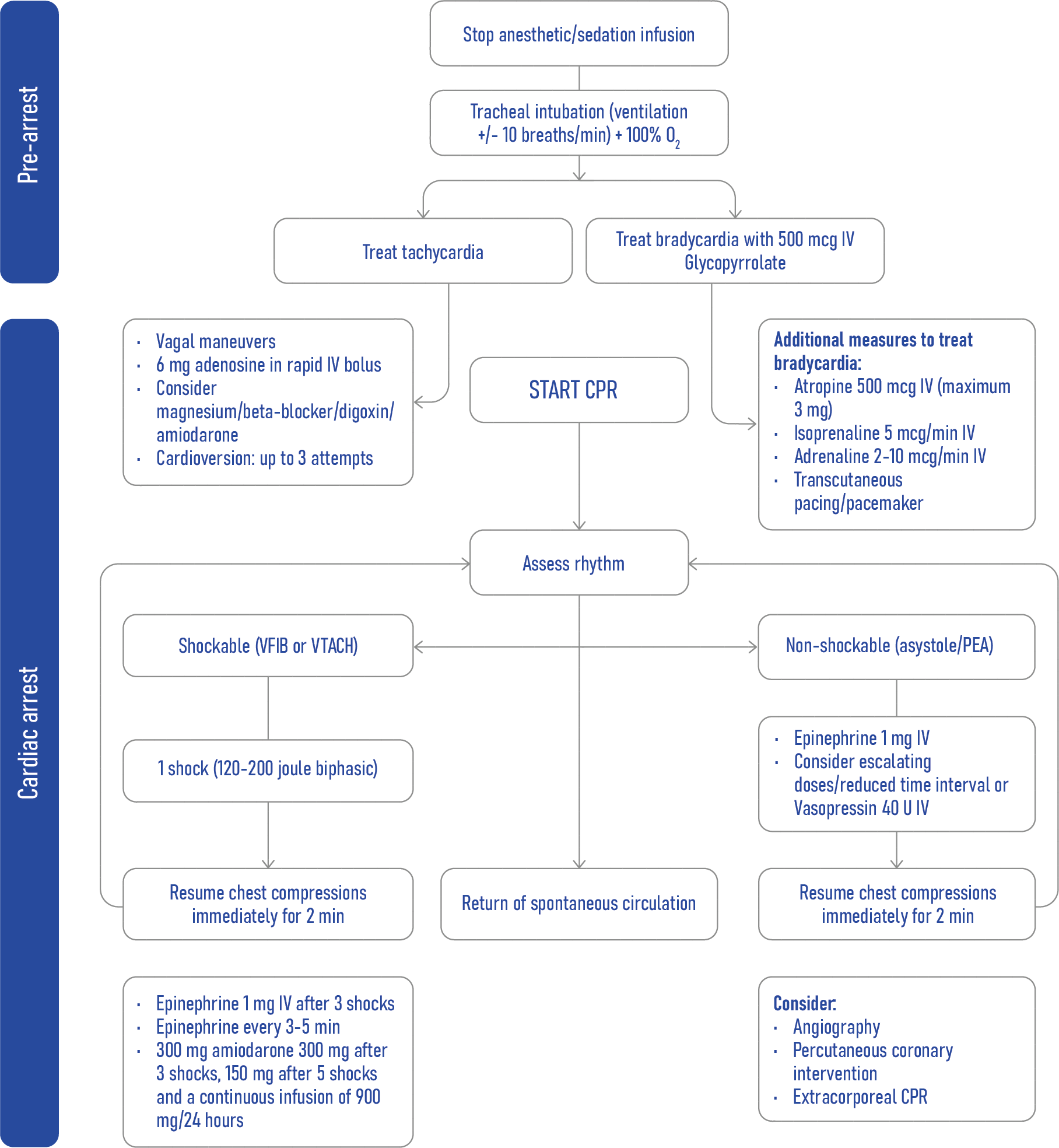
-
Rapid eligibility assessment
- Confirm no-flow and low-flow times.
- Assess age, rhythm, comorbidities, and reversible causes.
-
Team activation
- Alert ECMO team immediately if ECPR is considered.
- Coordinate anesthesia, perfusion, and surgical teams for cannulation.
-
Cannulation
- Peripheral cannulation (femoral vein/artery) is preferred for speed.
- Utilize ultrasound or TEE guidance to avoid vascular complications.
- Initiate ECMO flows at 3–4 L/min.
-
Ongoing support
- Maintain ECMO until ROSC or definitive therapy (e.g., cath lab, surgery).
- Monitor for complications such as left ventricular distension, limb ischemia, and bleeding.
Post-resuscitation care
Ventilation
- Use lung-protective settings: low tidal volumes (4–6 mL/kg), low driving pressures.
- Avoid hyperoxia and significant hypocapnia.
Temperature management
- Targeted temperature (32–36°C) for 24–72 hours may reduce brain injury.
- However, trials like TTM-2 show no clear advantage of hypothermia over normothermia.
- Monitor for arrhythmias or hypotension if cooling.
Hemodynamic management
- Titrate ECMO flow to maintain MAP 60–80 mmHg.
- Watch for left ventricular distension, which may require:
- Inotropes or vasodilators,
- IABP or Impella,
- Left atrial decompression procedures.
Oxygenation and perfusion
- Monitor right upper extremity PaO₂ to detect differential hypoxemia (Harlequin syndrome).
- Adjust ECMO and ventilator settings accordingly.
Conclusion
ECPR offers a powerful option for managing refractory perioperative cardiac arrest, especially when used promptly in well-selected patients. With the right infrastructure, training, and ethical oversight, it can significantly improve outcomes in critical scenarios. While not suitable for every case, ECPR has the potential to turn a dire emergency into a survivable event when applied wisely.
Reference: Pande K et al. Perioperative extracorporeal cardiopulmonary resuscitation in adult patients: A review for the perioperative physician. Anesthesiology. 2024;140:1026–1042.
Read more about this topic in NYSORA’s Anesthesia Updates.