Tibial fractures, including shaft and plateau injuries, are among the most common orthopedic traumas requiring surgical fixation. Effective pain management in this context is critical not only for patient comfort and mobility but also for reducing postoperative opioid reliance—a goal of increasing importance amid ongoing opioid stewardship efforts.
However, a persistent concern in orthopedic anesthesia is the potential for regional anesthesia to mask acute compartment syndrome (ACS), a serious complication that requires rapid diagnosis and intervention. Characterized by increased intracompartmental pressure and pain out of proportion to the injury, ACS can lead to irreversible nerve and muscle damage if untreated. The gold standard for early diagnosis has long depended on the patient’s ability to report pain accurately.
This has led to a clinical dilemma: while regional nerve blocks provide superior analgesia, especially through techniques like perineural catheters or single-injection blocks, their use in high-risk fractures has been approached cautiously. The fear is that by blocking pain sensation, these techniques might obscure early signs of ACS, delaying treatment and resulting in poor outcomes.
To address this concern, a team of researchers from the University of Florida conducted a large-scale retrospective study. Their aim was to determine whether perioperative regional anesthesia increased the risk of missing ACS in patients undergoing surgical treatment of tibial shaft and plateau fractures.
Study objective and methods
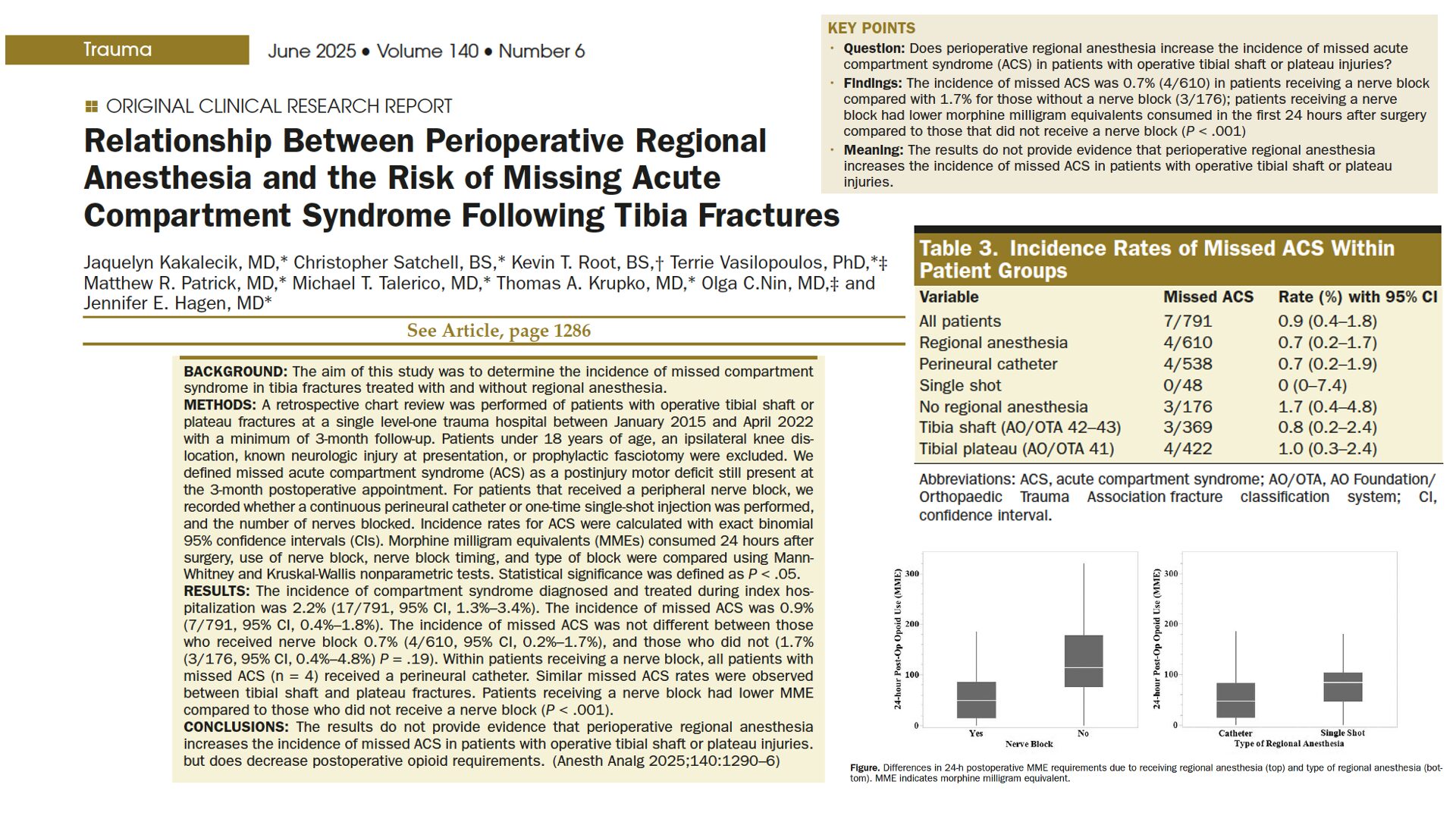
The central question was whether the use of regional anesthesia—specifically peripheral nerve blocks—would increase the likelihood of missed ACS in tibial fracture patients. A “missed” ACS was defined as a clinically significant event where a patient presented with a persistent motor deficit attributable to ACS that remained at the 3-month follow-up mark.
Study design:
- Type: Retrospective chart review.
- Setting: Single level-one trauma center.
- Time frame: January 2015 to April 2022.
- Population: 791 adult patients.
- Underwent surgical fixation of tibial shaft (AO/OTA 42 or 43) or tibial plateau (AO/OTA 41) fractures.
- Divided into two groups: Those who received regional anesthesia (n = 610) and those who did not (n = 181).
Exclusion criteria:
- Patients under age 18.
- Patients with ipsilateral knee dislocations or significant neurologic injuries at presentation.
- Patients who underwent prophylactic fasciotomies.
Data collected included:
- Patient demographics and injury characteristics.
- Anesthetic technique and nerve block type.
- Opioid use (converted into morphine milligram equivalents [MME]).
- Diagnosis and timing of ACS.
- Neurologic outcomes at discharge and at 3-month follow-up.
Regional anesthesia details:
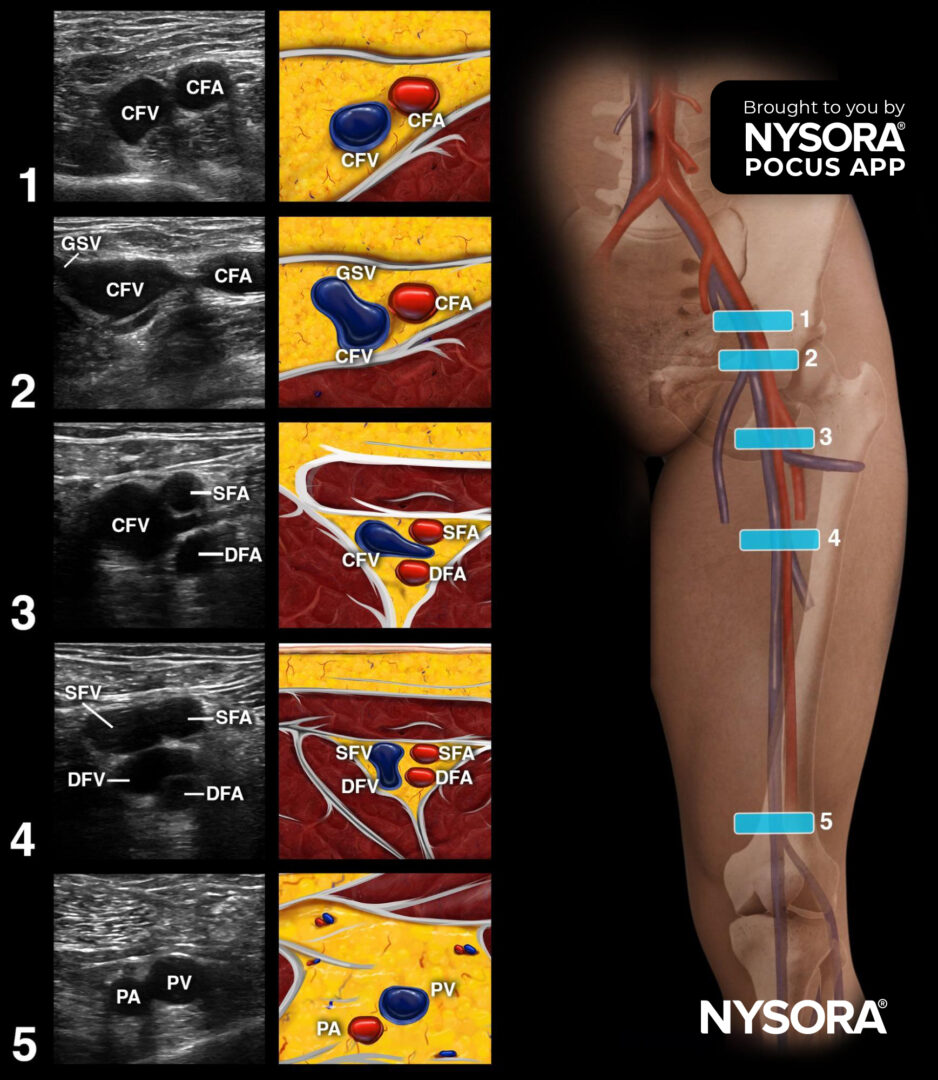
- 88.2% received perineural catheters.
- 7.9% received single-shot nerve blocks.
- 91.2% had both femoral and sciatic nerve blocks.
Key findings
-
Missed ACS was rare and not linked to regional anesthesia use
Only 7 out of 791 patients (0.9%) were identified as having missed ACS:
- Regional anesthesia group (n = 610): 4 patients (0.7%).
- No regional anesthesia group (n = 181): 3 patients (1.7%).
The difference was not statistically significant (P = 0.19). This finding directly contradicts the long-standing belief that regional anesthesia might conceal symptoms and delay diagnosis of ACS. Instead, patients with nerve blocks were not at greater risk—in fact, missed ACS occurred less frequently in this group, though not to a statistically meaningful extent.
-
All missed ACS cases in the regional anesthesia group involved perineural catheters
While this may suggest a trend worth further investigation, the study found no statistically significant difference in missed ACS incidence between perineural catheters and single-injection blocks. Nevertheless, this observation underlines the importance of vigilance when using continuous blocks.
-
Overall ACS rates were lower in the nerve block group
Interestingly, the study also found that patients who received regional anesthesia had a significantly lower incidence of ACS during their hospital stay:
- Regional anesthesia: 1.6%.
- No regional anesthesia: 4.5%.
- P = 0.041.
This could suggest a potential association between effective perioperative care—including pain management, surgical timing, and monitoring—and reduced ACS risk.
-
Significant opioid-sparing effect of regional anesthesia
Patients who received regional anesthesia had significantly lower opioid requirements in the first 24 hours postoperatively. This benefit was most pronounced in the perineural catheter group, highlighting the sustained analgesia advantage of continuous nerve blocks.
Median 24-hour MME: Lower in regional anesthesia group (< 0.001).
Reducing opioid consumption can lead to fewer adverse effects, improved recovery profiles, and lower risk of dependence, making this an important finding for both patient safety and healthcare policy.
Conclusion
This study offers reassuring and clinically meaningful insights for orthopedic and anesthesiology teams. It demonstrates that the use of perioperative regional anesthesia does not increase the risk of missing acute compartment syndrome in patients undergoing surgery for tibial fractures.
In fact, not only was the rate of missed ACS low in the nerve block group, but the overall incidence of ACS during hospitalization was significantly lower among patients receiving regional anesthesia. Furthermore, the marked reduction in opioid use reinforces the value of nerve blocks as part of modern multimodal pain strategies.
These findings suggest that—with appropriate monitoring and interprofessional collaboration—regional anesthesia can be safely and effectively used even in patients at theoretical risk for ACS. It challenges traditional hesitations surrounding nerve block use in trauma settings and supports broader integration of these techniques into perioperative care pathways.
Future research
Although this study represents one of the most comprehensive evaluations of its kind, several important questions remain unanswered. Future research should aim to:
- Conduct prospective studies: To validate these findings with standardized real-time monitoring and diagnostic protocols.
- Evaluate functional outcomes: Understanding the long-term impact of missed or diagnosed ACS will help refine criteria for “missed” cases and improve neurologic assessments.
- Compare block types and concentrations: Research should examine whether local anesthetic type or concentration influences the ability to detect evolving compartment syndrome.
- Develop monitoring algorithms: Formal protocols that combine regional anesthesia with frequent neurovascular checks could further reduce risks.
- Investigate multidisciplinary models: Studies that evaluate collaborative management between orthopedic, anesthesia, and acute pain services may offer deeper insights into optimal care pathways.
For more detailed information, refer to the full article in Anesthesia & Analgesia.
Kakalecik J. et al. Relationship Between Perioperative Regional Anesthesia and the Risk of Missing Acute Compartment Syndrome Following Tibia Fractures. Anesth Analg. Published online June 28, 2024.
Download the Nerve Blocks App HERE for in-depth insights on 60+ nerve block techniques from head to toe. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!