Thinner skin and fragile veins
- Challenge: The skin in elderly patients tends to be thinner and more delicate, and the veins are more fragile and prone to bruising or tearing.
- Solution: Use smaller gauge catheters whenever possible and a vein stabilizer or vein viewer to assist.
A) Thin skin and fragile veins in elderly patients. B) Veins in elderly are prone to bruising. C) Dehydration and loss of elasticity of subcutaneous tissue complicate IV cannulation in elderly patients.

Example of thrombosed, overused peripheral veins that have become unusable (A, B, C). The vein over the lateral aspect of the proximal wrist (D) appears still usable, but has thickened wall, and requires a smaller gauge IV catheter (e.g. 22G), good stabilization and rapid (snake-bite) insertion for successful cannulation.
Decreased vein elasticity
- Challenge: Veins in the elderly may be sclerotic with hypertrophic walls, making them more difficult to stabilize (rolling veins) and more challenging for the needle to enter.
- Solution: Stabilize the vein with the non-dominant hand and use traction to maintain the vein in position.
Less visible and palpable veins
- Challenge: Diminished skin turgor or increased adipose tissue can obscure vein visibility and palpability.
- Solution: Use vein illumination technology or ultrasound guidance to select a vein. Keep the arm in a dependent position to encourage venous filling.
More frequent valves and tortuous veins
- Challenge: The greater prevalence of intricate valves and tortuous veins, coupled with connective tissue atrophy in elderly patients, complicates IV cannulation.
- Solution: Use palpation to identify venous valves and avoid them. Ultrasound guidance can assist in identifying deeper, more suitable veins.

Stabilize the vein with the non-dominant hand and use digital traction with two fingers to maintain the vein in position.

Administering an IV in an elderly patient can be challenging because of decreased skin turgor, reduced elasticity in connective tissues, and veins that are both fragile and prone to shifting. The combination of these factors often leads to multiple attempts.
Less visible and palpable veins
- Challenge: Diminished skin turgor or increased adipose tissue can obscure vein visibility and palpability.
- Solution: Use vein illumination technology or ultrasound guidance to select a vein. Keep the arm in a dependent position to encourage venous filling.
More frequent valves and tortuous veins
- Challenge: The greater prevalence of intricate valves and tortuous veins, coupled with connective tissue atrophy in elderly patients, complicates IV cannulation.
- Solution: Use palpation to identify venous valves and avoid them. Ultrasound guidance can assist in identifying deeper, more suitable veins.

Tortuous veins on the dorsal side of the hand. Note the “bumpy” appearance of the valves.
History of multiple IV insertions
- Challenge: Previous IV cannulations can result in scar tissue, rendering some sites unsuitable for new insertions.
- Solution: Ask about previous IV sites and examine for scarred areas. Rotate sites when possible. Ask the patient where the IV works best for them. Many will point to where they previously had successful IVs.

Multiple failed attempts at IV cannulation can result in sites being unsuitable for new insertions.
Decreased patient tolerance
- Challenge: Lower tolerance to multiple punctures in elderly patients may be due to increased sensitivity to pain, anxiety, or cognitive dysfunction.
- Solution: Use local anesthetic and distraction techniques as appropriate and maintain clear, reassuring communication to alleviate discomfort.
Risk of phlebitis
- Challenge: Phlebitis, an inflammation of the veins, can be a complication of IV therapy, and certain medications are known to have a higher risk of causing this condition. These medications can irritate the vein’s inner lining, leading to inflammation and discomfort. Cumulative infusion of such medications and frequent IV cannulations can cause difficulties in future IV access.
- Solution: The risk of phlebitis can be reduced by proper dilution of medications, slow and steady infusion rates, and frequent rotation of IV sites. Using larger veins and ensuring proper IV catheter size and placement can also help minimize this risk. Always be vigilant for signs of phlebitis and take appropriate measures to prevent and manage it.
Some examples of medications that are commonly associated with the risk of phlebitis when administered intravenously include:
- Vancomycin: An antibiotic well-known for its potential to cause phlebitis. Infuse vancomycin slowly and dilute appropriately.
- Potassium chloride: Used to treat or prevent low potassium levels in the blood. High concentrations or rapid infusion of potassium chloride can be particularly irritating to veins.
- Chemotherapy agents: Many chemotherapeutic agents, such as doxorubicin and vincristine, are vesicants that can cause severe tissue damage if they leak from the vein. They can also cause phlebitis if infused too rapidly or in high concentrations.
- Calcium supplements: IV calcium (e.g. calcium gluconate) can be irritating to the vein walls, especially if infused rapidly.
- Amiodarone: Used for certain types of cardiac arrhythmias. Administer it through a central line to reduce the risk of phlebitis.
- Diazepam (Valium): Used for anxiety, seizures, and other conditions. It is known to be irritating to veins and can cause phlebitis.
- Ciprofloxacin: An antibiotic that, when given IV, can cause irritation to the veins.
- Nafcillin: An antibiotic used to treat bacterial infections, a frequent cause of phlebitis.
Other effects of various medications
The cumulative effects of various medications can further make IV cannulation challenging for the elderly. Here are some medications to be aware of. While immediate changes in an acute setting might not be feasible, understanding the mechanisms behind the effects of these commonly prescribed medications can provide valuable insight.
Anticoagulants
- Examples: Warfarin, heparin, dabigatran, apixaban, rivaroxaban.
- Challenge: Extended bleeding times complicate the post-insertion phase.
- Solution: Apply firm pressure post-insertion to prevent excessive hematomas hindering future cannulation attempts.
Antiplatelet agents
- Examples: Aspirin, clopidogrel.
- Challenge: Increased bleeding and hematoma risks.
- Solution: Monitor the insertion site closely for signs of prolonged bleeding.
Diuretics
- Examples: Furosemide, hydrochlorothiazide.
- Challenge: May cause dehydration, resulting in less visible veins.
- Solution: Assess hydration status before cannulation, and if necessary, hydrate the patient to enhance vein visibility.
Vasodilators
- Examples: Nifedipine, amlodipine, hydralazine.
- Challenge: Long-term use may modify vein tone and responsiveness.
- Solution: Be aware of potential vein behavior alterations during cannulation.
Steroids
- Examples: Prednisolone, cortisone.
- Challenge: Prolonged use might result in skin thinning, increasing the risk of skin tearing, though they may also cause fluid retention, which could influence vein condition.
- Solution: Proceed cautiously during cannulation and thoroughly assess the skin and vein condition.
Step-by-step technique of IV cannulation in the hand of an elderly patient demonstrating the difficulties with frail veins
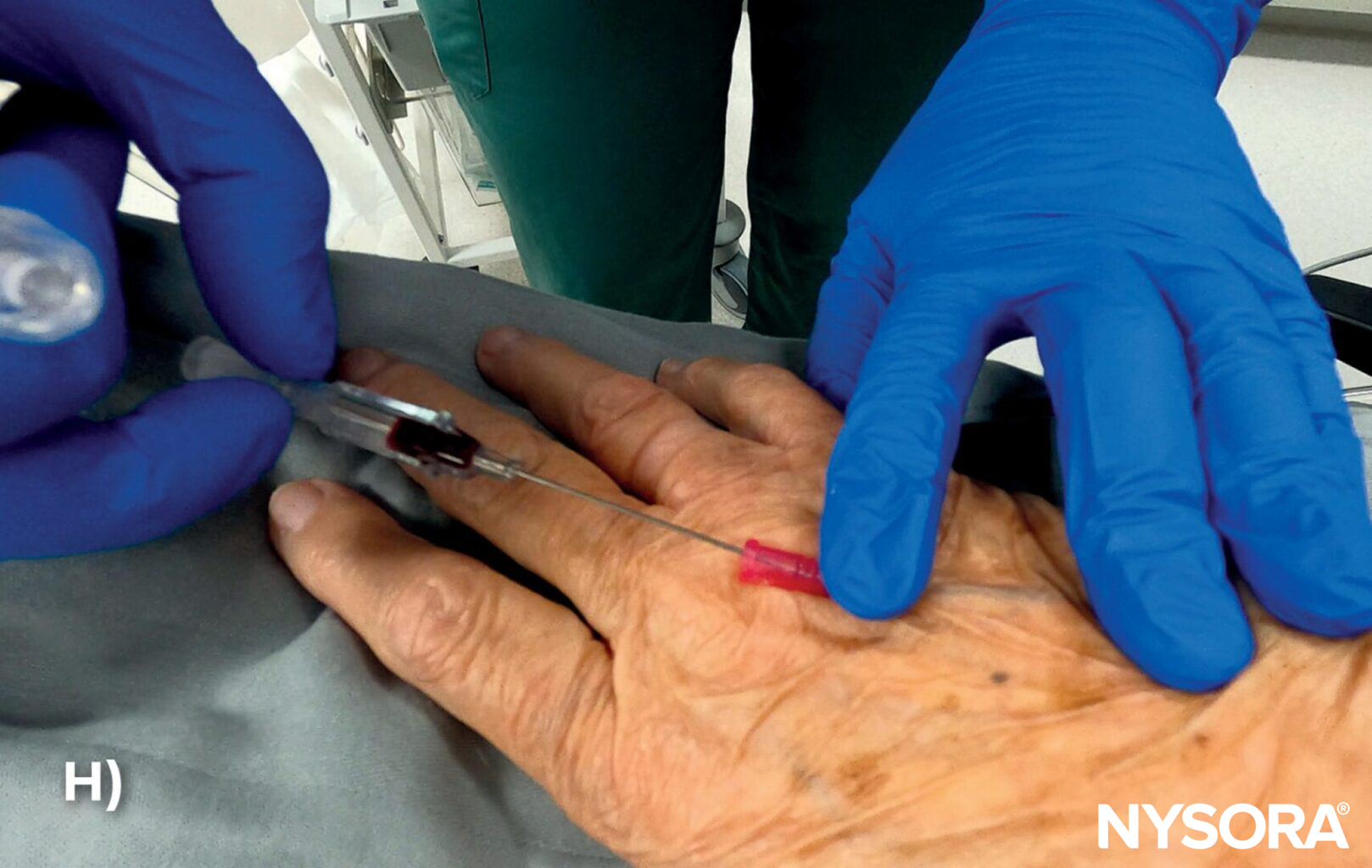
A) Lightly tap the skin to accomplish mild vasodilation to increase vein visibility. B) Disinfect the insertion site. C) Stabilize the hand and insert the needle at a shallow angle of ≤ 15 degrees. D) Advance the needle to ensure that the needle is in the vein. E) Blood in the flashback chamber indicates the needle is inside the vein. F) Advance the catheter an additional 1-2 mm to ensure the catheter tip is in the vein. G) Release the tourniquet. H) Retract the needle. I) Attach the IV tubing to the catheter. J) Secure the catheter with an occlusive dressing. K) Loop the IV tubing and tape it to the skin away from the insertion site.
TIPS
- Carefully tighten the tourniquet, as fragile veins can easily rupture at sites of previous attempts. Consider using a blood pressure cuff in a venostasis mode instead to achieve a more regulated and evenly distributed pressure.
- Older people tend to have more superficial veins with less supportive connective tissue. Lower the angle of the needle during insertion to prevent the needle from puncturing the vein’s wall (through and through).

Using a blood pressure cuff as a tourniquet during venipuncture in elderly patients.