IPACK stands for Infiltration of local anesthetic between the Popliteal Artery and Capsule of the Knee. It is a motor-sparing technique that anesthetizes the small articular sensory nerves from the popliteal plexus and obturator nerve resulting in analgesia of the posterior knee capsule.
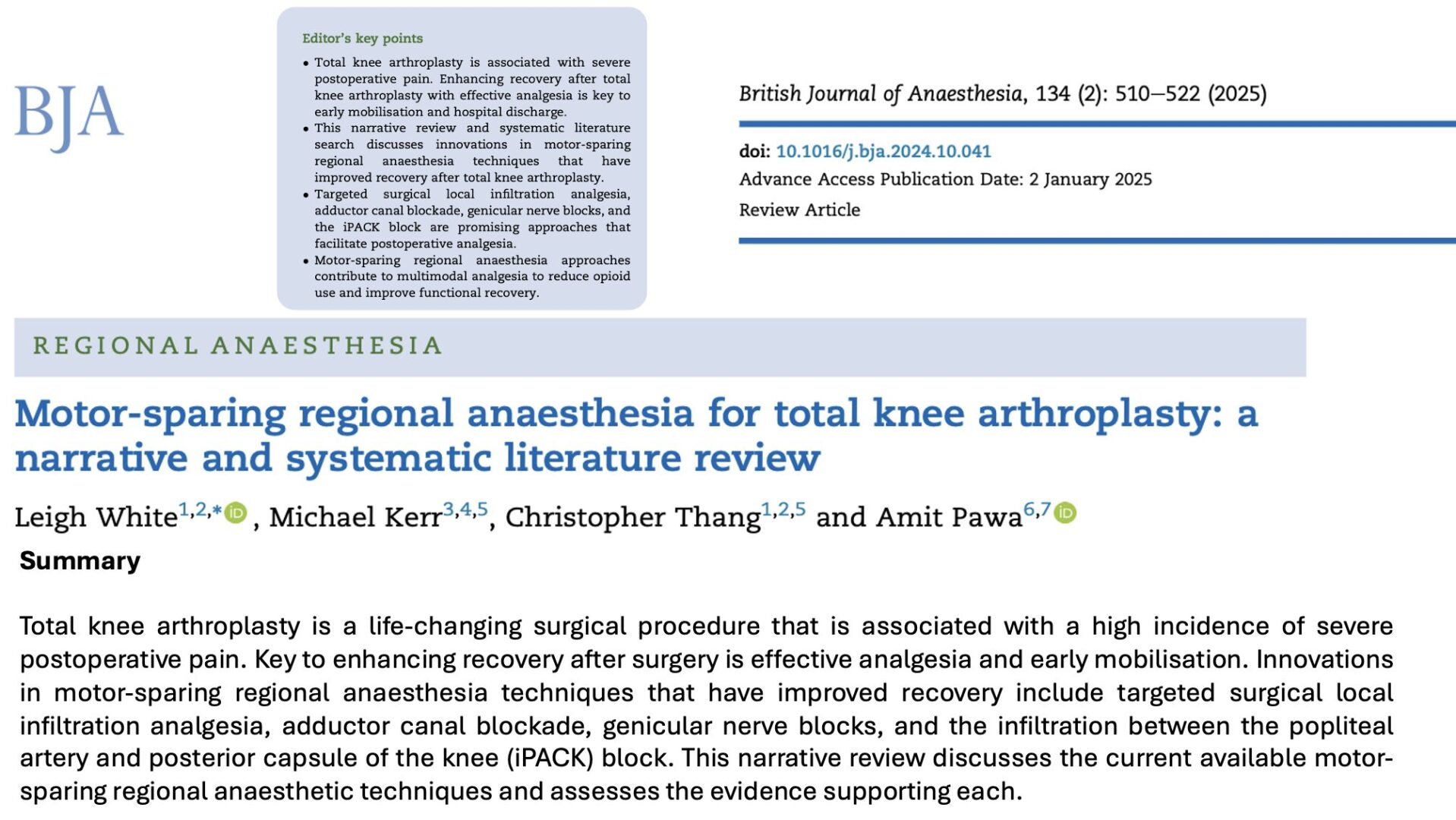
Ochroch et al. 2020 explored the role of the interspace between the popliteal artery and the capsule of the posterior knee (IPACK) block as part of a multimodal pain management protocol for total knee arthroplasty (TKA). The findings demonstrate that the IPACK block offers specific advantages in reducing posterior knee pain postoperatively, but its impact on broader recovery metrics remains uncertain.
Key highlights
Objective:
To determine whether adding the IPACK block to a multimodal analgesia regimen, including the adductor canal block (ACB), reduces posterior knee pain and improves recovery outcomes after TKA.
Study design:
- Prospective, randomized controlled trial.
- Conducted on 119 patients undergoing primary TKA.
- Patients were divided into two groups: ACB with IPACK and ACB with a sham block.
Primary outcome:
- Presence of posterior knee pain six hours after surgery.
Secondary outcomes:
- Pain scores, opioid consumption, mobility, and quality of recovery up to one week after surgery.
Methodology
Procedure:
- All participants received a multimodal perioperative pain protocol (MP3), including preoperative medications (acetaminophen, gabapentin, and celecoxib) and an ultrasound-guided continuous ACB.
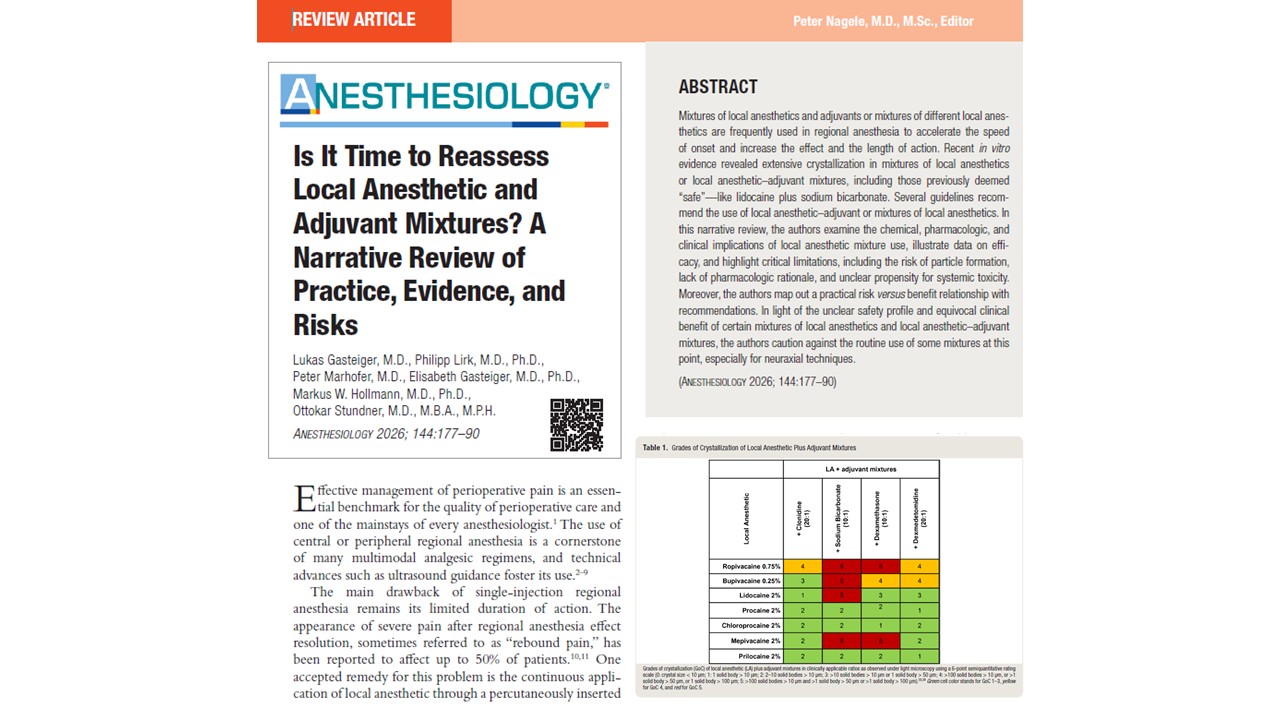
- The IPACK block was performed using 20 mL of 0.5% ropivacaine, targeting the posterior knee’s innervation while sparing motor function.
- Patients in the sham group received a superficial local anesthetic injection instead.
Outcome assessment:
- Pain location and intensity were recorded at six-hour intervals using a standardized chart.
- Functional recovery was evaluated through ambulation distance and Timed Up and Go (TUG) tests.
- Postoperative opioid consumption and patient-reported quality of recovery were also analyzed.
Results
- Reduction in posterior knee pain:
- The incidence of posterior knee pain at six hours was significantly lower in the IPACK group (21.7%) compared to the sham group (45.8%, p < 0.01).
- This benefit diminished over the next 48 hours, with pain levels converging between the groups.
- Pain scores:
- Patients in the IPACK group reported slightly lower pain scores at six, 12, and 48 hours postoperatively.
- The differences in mean pain scores were modest but statistically significant at some intervals.
- Opioid consumption:
- No significant differences in opioid requirements were observed between the two groups over the 48 hours.
- Functional recovery:
- Ambulation distances and TUG scores were comparable across both groups.
- Adding the IPACK block did not significantly affect physical therapy outcomes or the quality of recovery scores.
Discussion
Clinical relevance:
The IPACK block reduces immediate postoperative posterior knee pain without compromising motor function. Thus, it is a viable alternative to traditional sciatic nerve blocks, which can impair mobility.
Limitations of impact:
Despite its targeted pain relief, the IPACK block did not translate to significant improvements in opioid consumption, functional recovery, or overall quality of recovery metrics. These findings suggest its benefits may be limited to early postoperative pain management.
Safety and feasibility:
The IPACK block was safely performed under ultrasound guidance, with no reported complications such as foot drop or vascular injury. Its ease of implementation and safety profile further enhance its appeal as part of multimodal analgesia protocols.
Conclusion
The IPACK block shows promise as a motor-sparing technique for reducing posterior knee pain after TKA. However, its benefits appear limited to the immediate postoperative period, with no significant impact on long-term recovery or opioid use. Future research should explore strategies to prolong its analgesic effect, such as using adjuvants or continuous infusion techniques, to maximize its potential in postoperative pain management.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Ochroch J, Qi V, Badiola I, Grosh T, Cai L, Graff V, Nelson C, Israelite C, Elkassabany NM. Analgesic efficacy of adding the IPACK block to a multimodal analgesia protocol for primary total knee arthroplasty. Reg Anesth Pain Med. 2020 Oct;45(10):799-804.
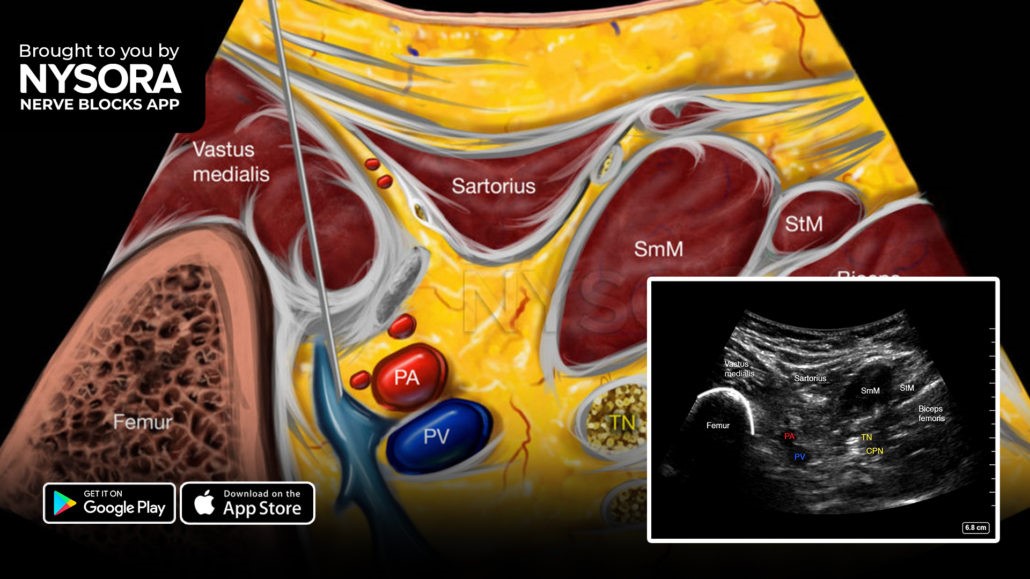
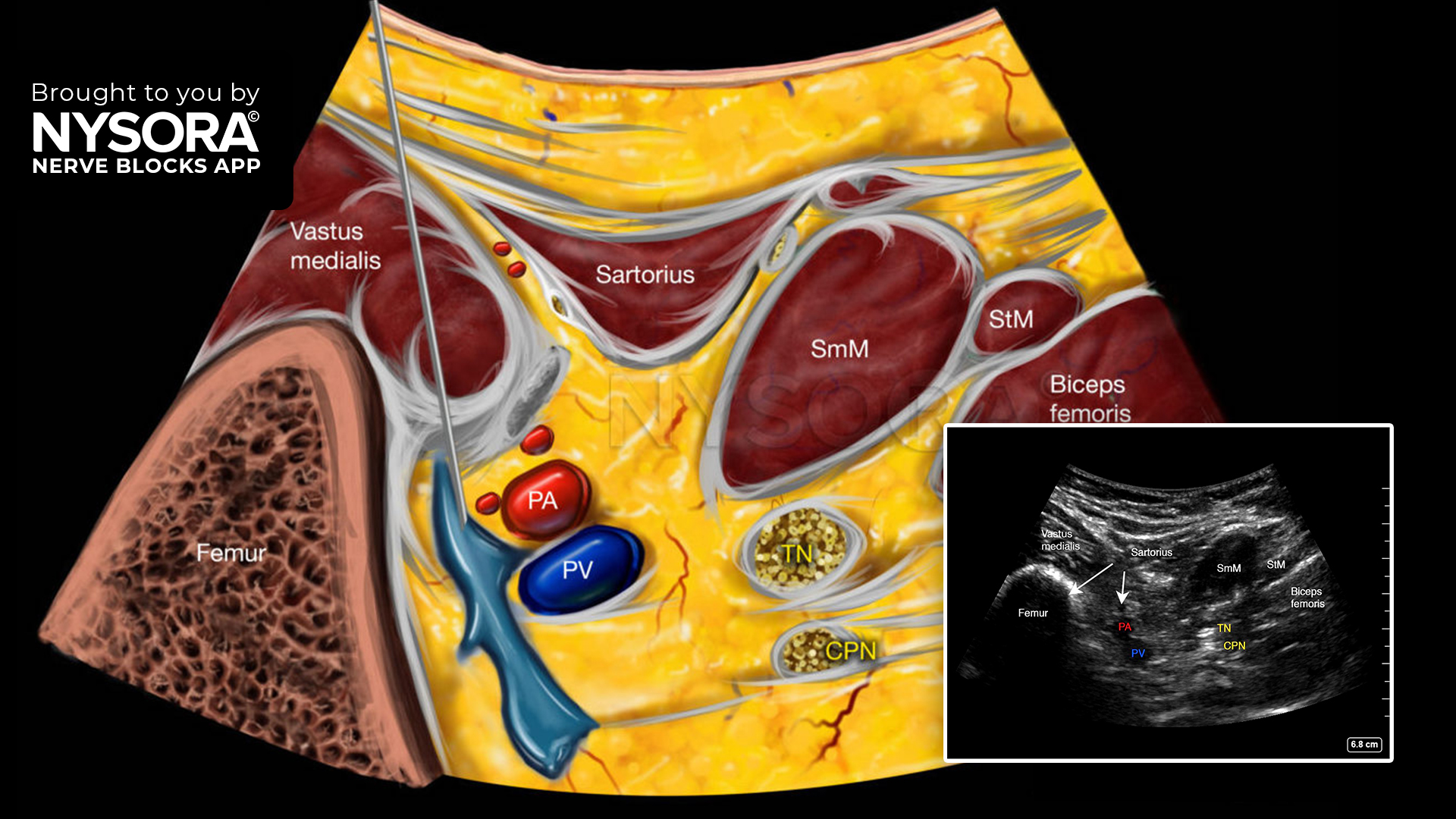
Here are 3 steps to successfully perform an IPACK block
- Place the transducer transversely over the medial aspect of the knee, 2-3 cm above the patella.
- Slide the transducer proximal and distal to identify the distal femoral shaft and popliteal artery.
- Insert the needle in-plane, from the anteromedial aspect of the knee, toward the space between the popliteal artery and femur, and inject 15-20 mL of local anesthetic.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!