Enhancing postoperative recovery with pecs and serratus plane blocks in breast surgery
The systematic review and meta-analysis by Grape et al. 2020 highlights the efficacy of Pectoral Nerves (PECS) blocks and Serratus Plane Blocks (SPB) in managing postoperative pain after breast surgeries. This comprehensive study, involving 16 randomized trials and 1026 patients, sheds light on how these regional anesthesia techniques can improve recovery outcomes.
Understanding PECS blocks
PECS blocks are classified into two types:
- PECS 1: Administers local anesthetic between the pectoralis major and minor muscles to block medial and lateral pectoral nerves.
- PECS 2: Extends the block to include intercostal nerves and the long thoracic nerve by injecting anesthetic between the pectoralis minor and serratus anterior muscles.
Serratus Plane Block (SPB)
SPB involves injecting local anesthetic around the serratus anterior muscle to block intercostal and thoracodorsal nerves.
Benefits of regional anesthesia
Pain management
- PECS blocks reduce rest pain scores by an average of 1.5 to 2.2 points on a 10-point scale.
- SPB offers comparable reductions in postoperative pain intensity.
Reduced opioid use
- Morphine equivalent consumption decreased significantly, with reductions of up to 7.2 mg in the first 24 hours post-surgery.
- These reductions are critical in minimizing opioid-related side effects.
Minimized PONV
- PONV rates dropped from 30.8% in the control group to 18.7% with PECS blocks, providing a smoother recovery process.
Surgical applications
Breast cancer surgeries
- PECS blocks demonstrated enhanced analgesic efficacy for radical mastectomies, particularly when axillary lymph node dissection was not performed.
Reconstructive surgeries
- PECS and SPB have proven effective in reducing pain and improving recovery for breast reconstructions.
Ambulatory procedures
- The techniques are particularly advantageous for day surgeries, offering sufficient pain relief without prolonged hospital stays.
Safety and complications
The systematic review reported a high safety profile for these blocks:
- No block-related infections across studies.
- Reduced complications compared to traditional opioid-centric pain management.
Clinical recommendations
- PECS blocks should be integrated into multimodal analgesic protocols for breast surgeries.
- Timing is essential: blocks are best performed after general anesthesia induction but before surgery.
- Using long-acting anesthetics, such as ropivacaine or bupivacaine, ensures extended pain relief.
Key takeaways
- PECS blocks significantly reduce rest and dynamic pain scores at 2, 12, and 24 hours post-surgery.
- These blocks also lower postoperative opioid consumption and rates of nausea and vomiting (PONV).
- The benefits are consistent across various breast surgery types, including mastectomies and reconstructions.
Conclusion
Integrating PECS and Serratus Plane Blocks into postoperative care represents a transformative advancement for breast surgery patients, combining effective pain management with reduced reliance on opioids and lower rates of postoperative nausea and vomiting (PONV).
For more information, refer to the full article in the Journal of Clinical Anesthesia.
Grape S, Jaunin E, El-Boghdadly K, Chan V, Albrecht E. Analgesic efficacy of PECS and serratus plane blocks after breast surgery: A systematic review, meta-analysis and trial sequential analysis. J Clin Anesth. 2020 Aug;63:109744.
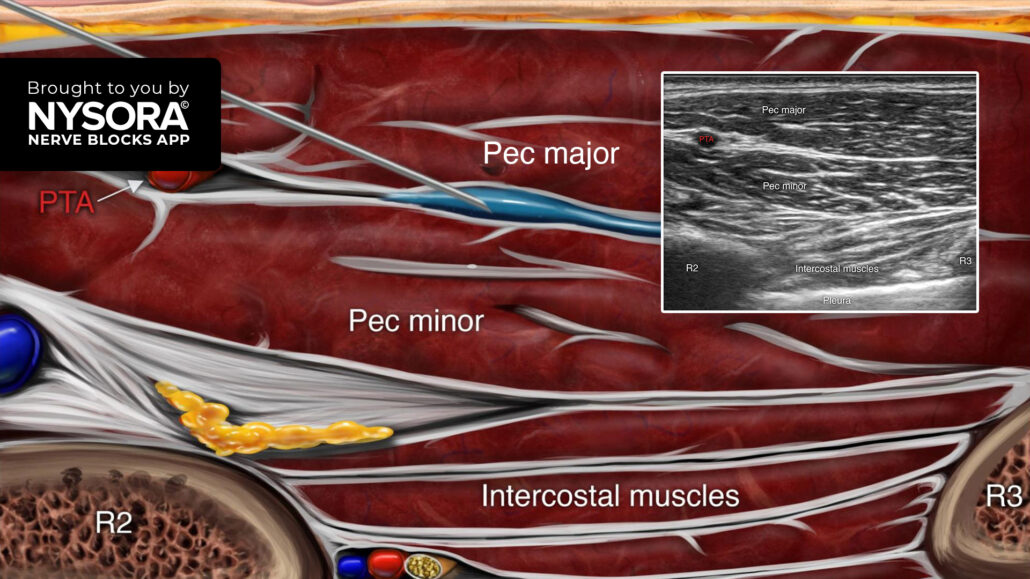
Learn the 3 key steps to successfully perform a PEC I block:
- Place the transducer in a sagittal orientation below the midline of the clavicle.
- Identify the pectoralis major and minor muscles with the axillary artery, vein, and elements of the brachial plexus lying under the fascia of the pectoralis minor. Slide the transducer caudally to identify the 2nd and 3rd ribs.
- Insert the needle in-plane, from cephalad to caudal, and inject 10-20 mL of local anesthetic between the pectoralis major and minor muscles.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!