Intraoperative hypotension (IOH), a frequent occurrence during major surgeries under general anesthesia (GA), is more than a fleeting drop in blood pressure; it’s a potential precursor to significant postoperative complications. A newly published systematic review by Lee et al. (A&A, 2025) offers a comprehensive examination of clinical strategies designed to mitigate IOH in patients undergoing major noncardiac surgery under GA. The findings, drawn from 48 randomized controlled trials (RCTs) involving over 46,000 patients, offer a nuanced examination of what works, what doesn’t, and where further research is needed.
What is intraoperative hypotension?
Intraoperative hypotension is typically defined by a sustained decrease in mean arterial pressure (MAP), often below 60–70 mm Hg. This condition, if prolonged or severe, can compromise perfusion to vital organs, including the brain, heart, and kidneys.
- MAP <65 mm Hg for ≥ 5 minutes: Moderate risk of organ damage
- MAP <65 mm Hg for ≥ 20 minutes: High risk of major organ injury
- MAP <60 mm Hg: Strong association with acute kidney injury (AKI), myocardial infarction (MI), and increased mortality
Given its impact, timely recognition and intervention are critical to improving surgical outcomes.
Major blood pressure optimization strategies
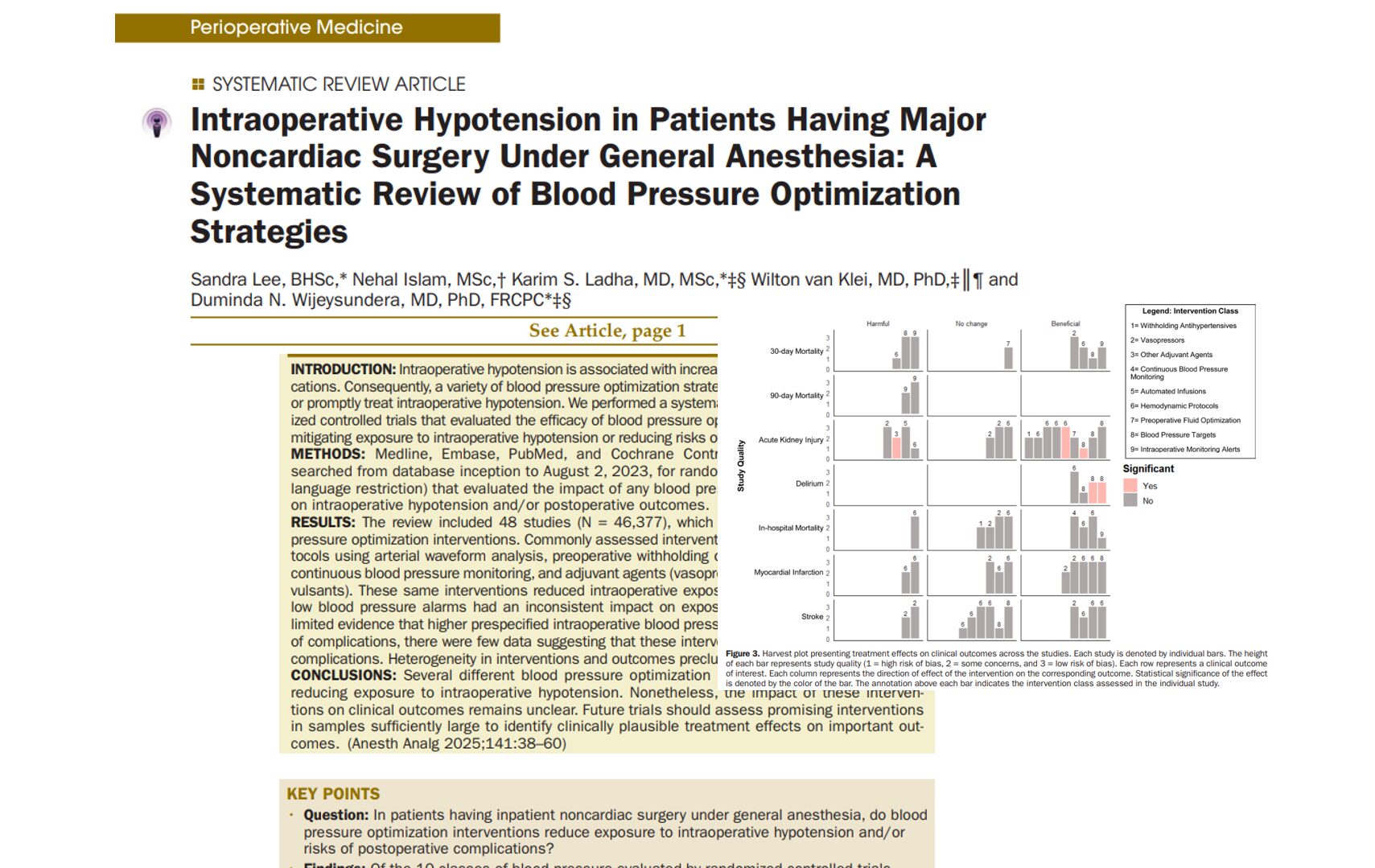
Lee et al. classified blood pressure optimization strategies into 10 categories (plus a combined strategy). Here’s a breakdown of the most effective approaches:
1. Protocolized hemodynamic management (± alarms)
- Devices used: Arterial waveform analysis, esophageal Doppler
- Findings: 8 of 12 studies showed reduced IOH
- Impact on outcomes: No consistent reduction in postoperative mortality, MI, or stroke
- Conclusion: Beneficial for intraoperative control, but evidence lacking for long-term outcome benefits
2. Prespecified intraoperative blood pressure targets
- Approach: Maintain MAP ≥ 80 mm Hg or within 10% of baseline
- Findings:
- Lower risk of AKI and delirium in 3 of 6 studies
- No difference in 30-day mortality in other studies
- Conclusion: Tailored BP targets may enhance patient safety, particularly in those at higher risk
3. Continuous versus intermittent blood pressure monitoring
- Technology: Noninvasive finger cuff monitors
- Findings: All 4 studies demonstrated reduced IOH exposure
- Outcome effect: No change in mortality rates
- Conclusion: Valuable for early detection, especially during induction
4. Preoperative withholding of antihypertensives
- Medications affected: ACE inhibitors and ARBs
- Findings:
- 3 of 4 studies showed reduced IOH when drugs were withheld 12–36 hours pre-op
- A large trial combining drug withdrawal and target MAP strategy (n = 7490) showed reduced IOH, but no significant impact on cardiovascular outcomes
- Conclusion: Withholding certain antihypertensives pre-op is promising, but must be individualized
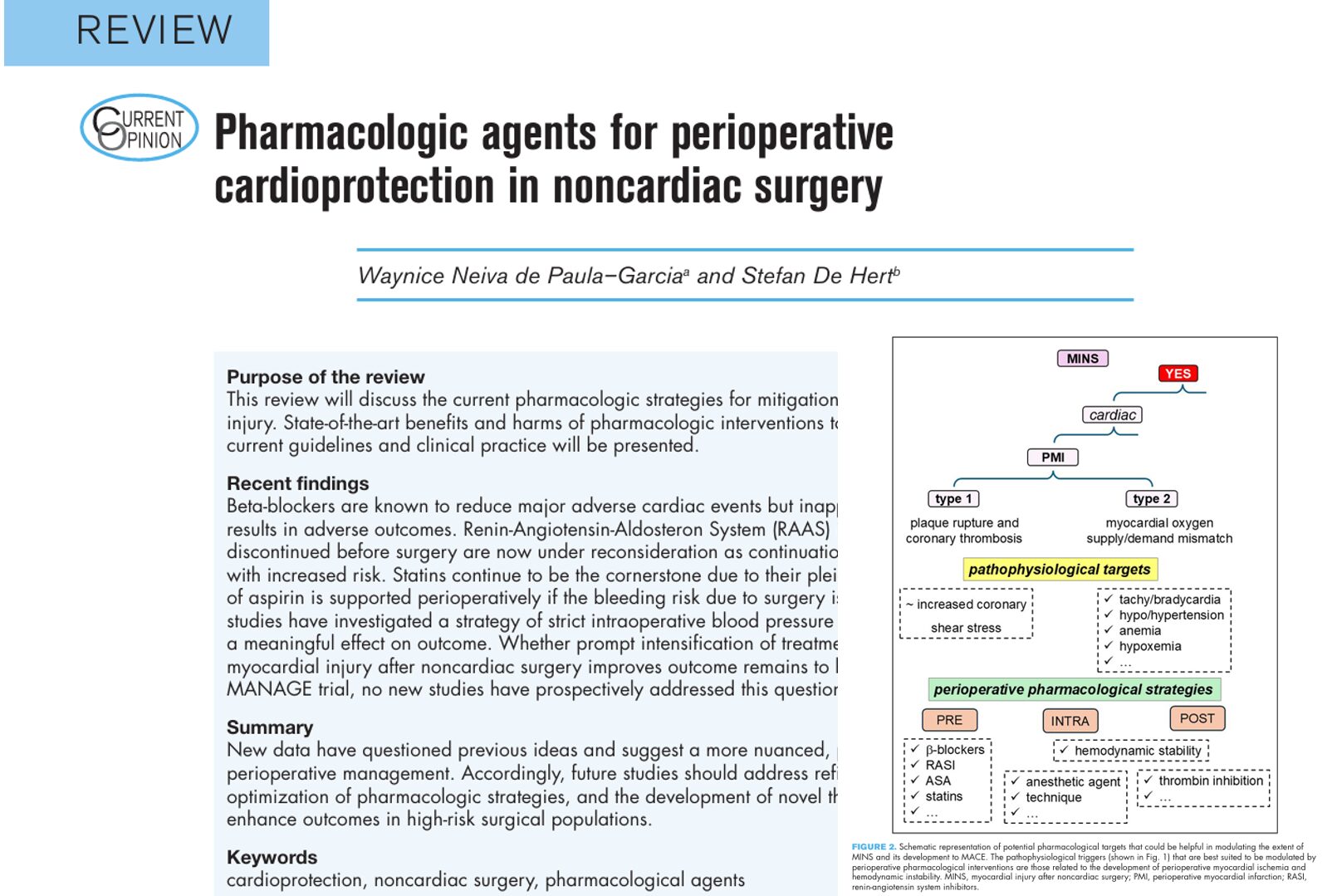
5. Vasopressors and adjuvant agents
- Vasopressors: Norepinephrine, ephedrine, phenylephrine
- Others: Atropine, glycopyrronium, gabapentin, methylene blue
- Findings:
- Norepinephrine consistently reduced IOH
- Gabapentin and atropine showed a mild benefit
- Methylene blue showed benefit, but requires larger studies
- Conclusion: Pharmacologic support is vital, with norepinephrine emerging as a top choice
6. Automated blood pressure management
- Tools: Closed-loop vasopressor systems
- Findings: Significant reductions in IOH exposure compared to manual titration
- Conclusion: Automation may enhance consistency and precision ,but needs broader validation
7. Intraoperative hypotension alerts
- Systems analyzed: SBP alarms, “double-low” and “triple-low” alerts
-
- “Double-low” (MAP <75 + deep anesthesia) improved outcomes
- “Triple-low” and standard SBP alarms had negligible effectsFindings:
- Conclusion: Advanced alert systems may improve response times ,but are not universally effective
8. Preoperative fluid optimization
- Methods: IV hydration, ultrasound-guided protocols
- Findings:
- All 5 studies demonstrated decreased IOH with fluid loading
- Lower MAP reductions during induction and fewer hypotensive episodes
- Conclusion: Simple yet effective, especially in fluid-sensitive patients
9. Prewarming
- Method: Warming blankets before anesthesia
- Findings: One small study showed no benefit and possible harm
- Conclusion: Not recommended based on current evidence
Final thoughts
The evidence presented by Lee et al. (2025) affirms that multiple interventions can reduce intraoperative hypotension. However, translating these reductions into improved clinical outcomes remains a challenge. Strategies like individualized BP targets, continuous monitoring, and protocolized management are promising but require broader implementation and more robust evidence.
Future trials must focus on:
- Standardizing definitions of hypotension
- Targeting high-risk populations
- Evaluating composite clinical outcomes beyond IOH
In the meantime, anesthesiologists should adopt a multimodal, evidence-based approach to manage intraoperative blood pressure effectively.
Reference: Lee S et al. Anesth Analg. 2025;141:38-60.
For more information on patient blood pressure optimization guidelines, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Here’s what MAIA Anesthesia Assistant recommends:
How to best optimize blood pressure during general anesthesia?