Patients with diabetes often have complications such as peripheral vascular disease, changes in skin texture, and susceptibility to infection, all of which can complicate the process of obtaining and maintaining reliable IV access.
The significance of understanding these challenges cannot be overstated, as IV access is essential for administering medications, fluids, and sometimes insulin, especially in acute care settings or during surgical procedures. The altered vascular integrity found in many diabetic patients, combined with potential edema and neuropathy, necessitates a strategic approach to cannulation, often requiring the use of ultrasound guidance, to improve success rates and minimize patient discomfort.
Vascular complications
- Challenge: Chronic hyperglycemia can lead to narrowed, hardened, or less elastic veins.
- Solution: Use ultrasound guidance to identify more robust veins. Consider deeper veins if superficial veins are compromised.
Skin changes and infections
- Challenge: Diabetes often alters skin texture, reduces the healing processes, and heightens infection susceptibility.
- Solution: Follow strict aseptic techniques during venipuncture to mitigate infection risks. Choose insertion sites free of skin changes or abnormalities.
Neuropathy and sensation change
- Challenge: Diabetic neuropathy may alter pain perception.
- Solution: Communicate clearly with the patient to understand their comfort level. Use local anesthetics judiciously to maintain patient comfort.
Fluid and electrolyte imbalances
- Challenge: Diabetic patients may present with dehydration or other fluid and electrolyte imbalances that can make veins less filled and more difficult to cannulate.
- Solution: Orally hydrate the patient to enhance venous volume and distensibility. Monitor the patient’s electrolyte status and adjust care accordingly.
Thickened skin or scar tissue
- Challenge: Repeated insulin injections can lead to thickened skin or scar tissue areas, which may interfere with IV placement.
- Solution: Avoid areas of lipohypertrophy or thickened skin when selecting an IV site. Rotate IV sites and educate diabetic patients on rotating their injection sites to prevent skin complications.
Step-by-step technique of a double IV cannulation in a diabetic patient
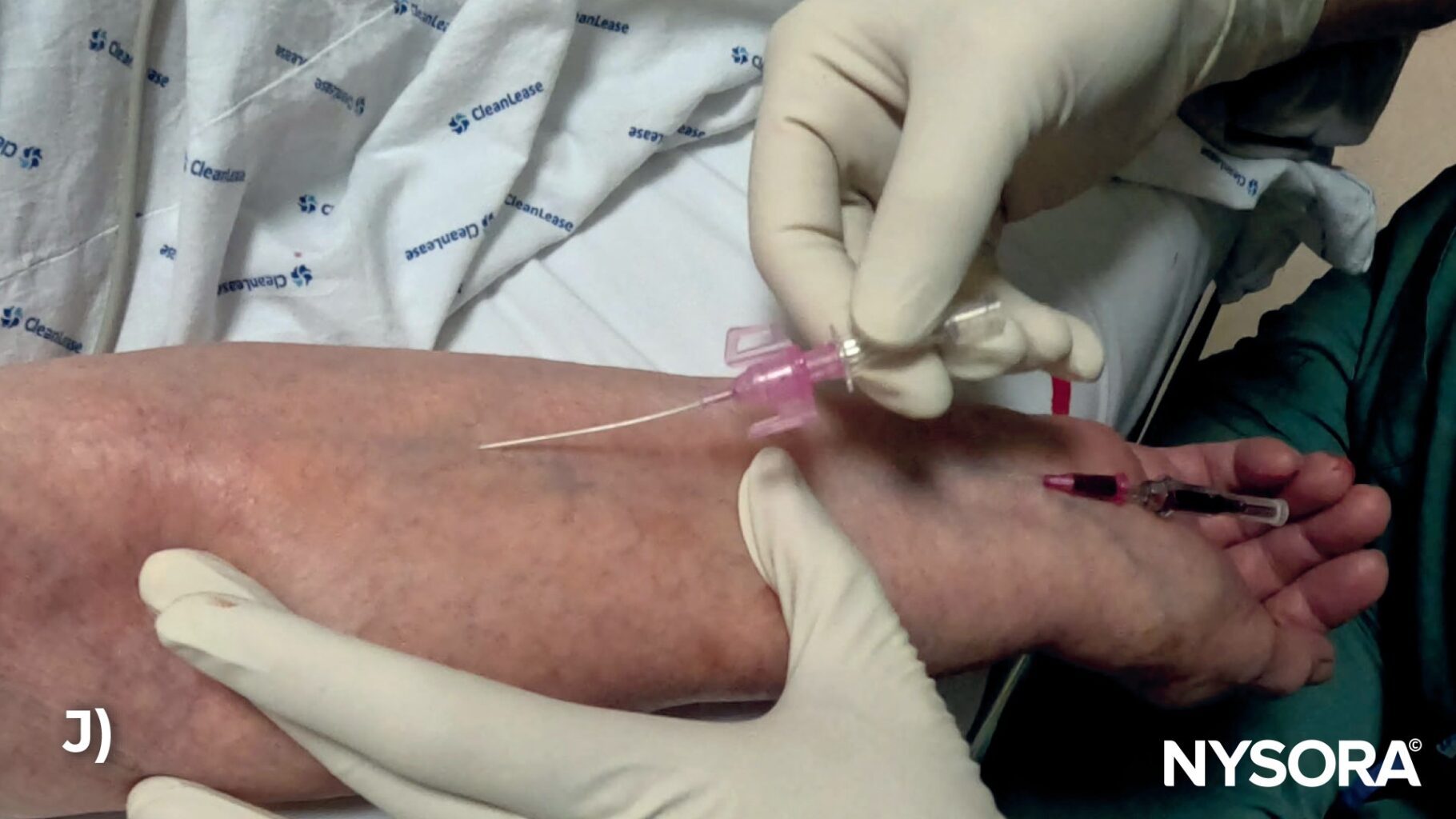
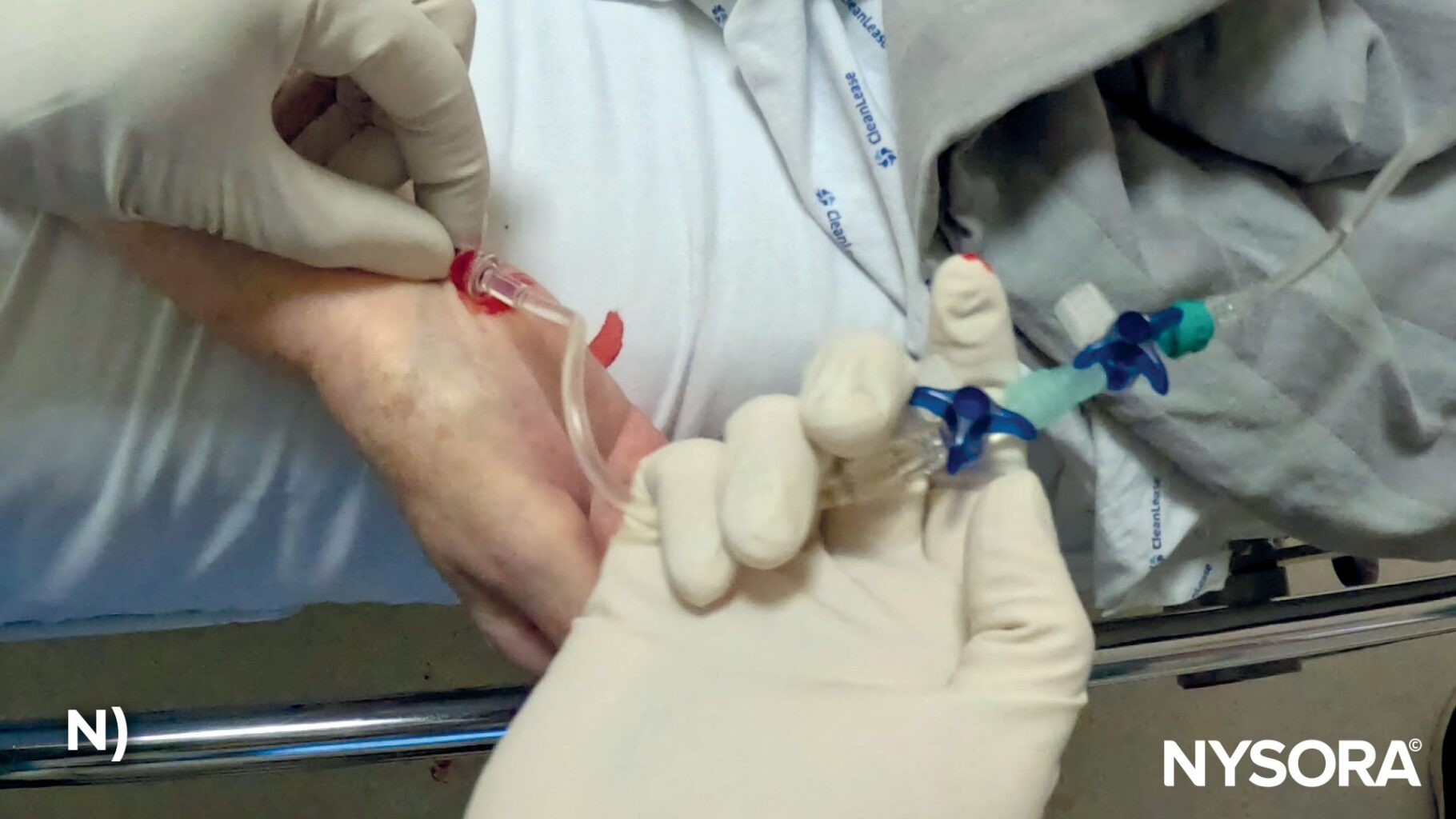
Double IV access in a patient with diabetes who required two IV lines for infusion of IV fluids for volume resuscitation and infusion of antibiotics. Note the tortuous and sclerotic appearance of the superficial veins in the patient’s forearm. A) Apply the tourniquet. B) Identify suitable veins for IV cannulation. C) Disinfect the skin to make the veins more prominent. D) Use a bent and short 20G catheter.E) Stabilize the hand and insert the needle with a low angle. F) Look out for the blood flashback. G) Advance the catheter. H) One workable IV cannulation is established. I) Use a bent and winged 20G catheter to establish the second IV access point. J) Stabilize the arm and insert the needle with a very low angle. K) Look out for the blood flashback. L) Advance the catheter and retract the needle. M) A proximal and distal IV access point. N) Attach the IV tubing. O) Secure the catheter with adhesive dressing.
VIDEO: https://youtu.be/y9LtTJSvJjs