|
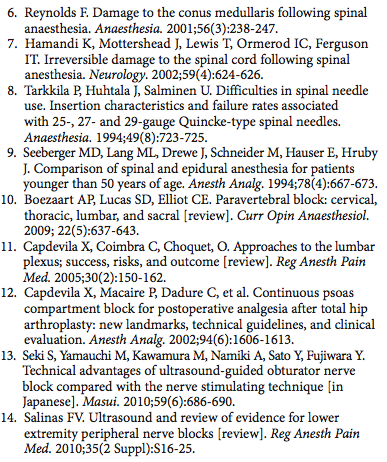
Introduction Authors: Manoj Karmakar and Catherine Vandepitte Central neuraxial blocks (CNBs), which include spinal, epidural, combined spinal epidural (CSE), and caudal epidural injections, are commonly practiced regional anesthesia techniques in the perioperative period, for obstetric anesthesia and analgesia, as well as for managing chronic pain. (1) Traditionally, CNBs are performed using surface anatomic landmarks, operator tactile sensation (loss of resistance) during needle advancement, and/or visualizing the free flow of cerebrospinal fluid. Although anatomic landmarks are fortuitous because spinous processes provide a relatively reliable surface landmark in many patients, they are not always easily recognized or reliable signs in patients with obesity, (2) edema, underlying spinal deformity, or after back surgery. Even in the absence of spine abnormalities, data suggest that a clinical estimate of a specific intervertebral space based on the surface anatomy may not be accurate in many patients. (3,4) In other words, a clinical estimate of an intervertebral space often results in needle placement one or two spinal levels higher than intended. (3,5,6) This estimation error has been attributed as a cause of injury of the conus medullaris or spinal cord after spinal anesthesia. (5,7) The difficulty of identifying the correct level is particularly present in patients with obesity and when accessing intervertebral space in the upper spinal levels. (3,5,7) Therefore, the Tuffier’s line, a surface anatomic landmark that is used ubiquitously during CNB, is not a consistent landmark. (6) Moreover, because of the blind nature of the landmark-based techniques, it is not possible for the operator to predict the ease or difficulty of needle placement prior to skin puncture. In a study of 300 spinal anesthetics, 15% of attempts were judged to be technically difficult, and 10% required more than five attempts. (8 )In another study including 202 patients who were under 50 years of age, failed CNB was reported in 5% of cases. (9) Thus the need to establish a more reliable method to identify the spinal levels and needle advancement toward the neuraxis continues to inspire clinical and imaging studies. Although a number of surface-based landmarks and nerve stimulation-guided peripheral nerve block techniques are well established, localization and block of the deeper positioned peripheral nerves and plexi remain largely “blind” procedures (e.g., lumbar plexus block, sciatic block, and infraclavicular block). This is particularly true with nerve block procedures where nerve stimulation is not easily accomplished due to the specifics of the anatomy (e.g., deep position) and where the goal of the procedure is to place the needle in a certain anatomical space, rather than localize the nerves that are not easily accessible to nerve stimulation (e.g., intercostals blocks, paravertebral blocks, and fascia iliaca blocks). Consequently, significant research efforts have focused on improving the current techniques of block and establishing more reliable surface landmarks and needle orientation procedures. (10-12) Due to the nature of the surface-based procedures and inherent difficulty with electrolocalization of deeply positioned peripheral nerves, many of these procedures are not used commonly and are confined to a few practices where substantial expertise is available. The introduction of ultrasound guidance in regional anesthesia has sparked a renewed interest in these procedures. (13,14) Ultrasound can be used to depict the location and spatial relationship (e.g., depth) of the osseous landmarks to help estimate both the correct site as well as the depth of needle insertion. Imaging of the deep structures as well as structures that are concealed by osseous processes requires considerable skill and dexterity. In addition, needle visualization and needle-nerve interface can be challenging because of interference with the osseous structures and depth of the needle placement. Given these limitations and a close relationship of the nerve structures to the centroneuroaxis, questions have been raised about the overall safety of ultrasound-guided neuraxial blocks, lumbar plexus and paravertebral blocks if taught as a standard practice. At the time of this publication, ultrasound-guided blocks for the purpose of neuraxial anesthesia, and perineuraxially located nerves and plexi are not well-established. These advanced ultrasound-guided or ultrasound-assisted block techniques are currently practiced only by experts who have spent considerable time mastering ultrasound anatomy. Often, even the most experienced privately admit that ultrasound-guided centroneuraxial blocks are not practical as a routine practice. For example, in our practice most centroneuraxial blocks are done without ultrasound guidance, whereas ultrasound is being increasingly used for lumbar plexus and paraveretebral blocks. For this reason and to avoid imparting a false impression that these are standard techniques, we have opted to discuss them within the context of ultrasound anatomy, rather than as well-established procedures. An informed reader then can make use of the presented anatomical, pharmacological and technical information to devise own techniques and/or make decisions regarding the applicability of ultrasound in these techniques in his/her own practice.
|
Explore NYSORA knowledge base for free: