Today we’re talking about nerve stimulation in conjunction with ultrasound-guided nerve blocks – a controversial topic by some that we believe needs some much-deserved spotlight. Yes, we all know some experts vehemently oppose this practice, stating a lack of evidence. And using a nerve stimulator can be a hassle: the nerve stimulator needs to be connected, batteries need replacements, current needs to be dialed, the device has to be calibrated, nerve stimulation must be interpreted, etc. However, the hassles of using aside, we’re strongly advocating a broader perspective for the safety and enhancement of nerve block procedures. Let’s explore why.

Why Nerve Stimulators?
In an ideal world, we could rely solely on ultrasound for perfect needle guidance during nerve blocks. Yet, we know the reality can be far from ideal. Image quality, operator interpretation, and other variables can lead to inaccuracies. We see nerve stimulators as additional sensors – alert systems if you will, much like those in an airplane or car – which warn the operator of potential dangers. While the ultrasound tells us what we ‘see,’ the nerve stimulator tells us what we might ‘miss.’ It’s an extra layer of security to ensure we’re not venturing too close to the nerve.
Beyond Subjectivity: A Plea for Objective Standards
Here’s another angle to consider. The societies are currently failing to reach a consensus on regional anesthesia standards. This debate is stalling the development of our specialty. While not every practitioner is a professional car driver, we all need the right tools for safety.
Think about pulse oximetry, for example. Adopted in 1989 as a standard ASA monitor during anesthesia administration, despite the lack of clear-cut evidence of its impact on patient safety, it revolutionized anesthesia practice. It moved us away from subjective observations towards objective, measurable, and communicable data.{1}
Similar to this, nerve stimulators can provide objective evidence to practitioners during nerve block procedures, enhancing both patient safety and protection from legal liabilities. And just for the record, NYSORA’s research has revolutionized the nerve stimulation technology in 2003 where we published the inconsistency in manufacturing standards of nerve stimulators and established ideal characteristics of nerve stimulators used in peripheral nerve blocks, so if interested – this the best read on this topic {2}
A Safety Net in Medico-Legal Scenarios
From a medico-legal standpoint, nerve stimulators can offer vital objective data. An absent motor response throughout a nerve block procedure indicates that needle-nerve contact or intraneural needle placement was unlikely. Although it’s not a 100% guarantee, it strengthens the claim that the practitioner did their best to prevent nerve injury. A documentation that clearly states “NO” for nerve stimulator response, is an objective documentation, largely independent from the observers interpretation, as it is binary, “YES” or “NO”.
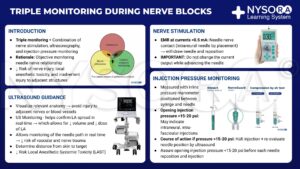
Adding injection pressure monitoring to the mix, recording that the injection pressure never breached 20 psi, further strengthens the practitioner’s case in any potential legal proceedings. {3}
To read more about triple monitoring during nerve blocks, check out NYSORA’s Compendium of Regional Anesthesia.
How to use Nerve stimulator with Ultrasound-guided nerve blocks
The game has changed. With ultrasound, we’re no longer hunting for that motor response to find the nerve. The ultrasound already does that job. Instead, we’re using the nerve stimulator as a safety net. Here’s how it works:
1️⃣ Set your nerve stimulator to 0.5 mA (0.1 msec) and let it be.
2️⃣ Use the ultrasound to guide your needle to the right place for injection. No motor response? Perfect. That’s what you want. Go ahead and inject your local anesthetic. 💉
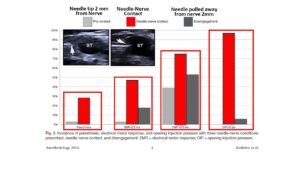
3️⃣ But what if you get a distal motor response? This means your needle might be too close to the nerve, or even on or inside it. Not an ideal situation.
4️⃣ So what do you do? You pull the needle back a bit until the motor response is gone. This ensures your needle is at a safe distance from the nerve before you proceed with the injection.
Remember, the goal here is safety, not localization. By integrating a nerve stimulator with your ultrasound-guided nerve blocks, you’re adding an extra layer of security to your procedure. It’s all about keeping nerve blocks safe and sound! {4, 5}
The Bottom Line
Nerve complications can occur despite our best efforts, but using tools like nerve stimulators and injection pressure monitors can assure us that we’ve done everything possible to prevent nerve injury. Click on the link below for the video on NYSORA’s YouTube Channel, where we explain why and how you should use nerve stimulators for an additional layer of safety in nerve blocks and bullet-proof medicolegal documentation.
Until then, remember – practice safe, practice smart, and never stop learning. And if you want to amp up your Regional Anesthesia game, you must have NYSORA’s Compendium of Regional Anesthesia. This power-packed guide comes brimming with animations, insightful illustrations, and real-life clinical videos, ready to transform your understanding of regional anesthesia.
Head over to Compendium of Regional Anesthesia and immerse yourself in an unrivaled learning experience! Your NYSORA team.
References
- Eichhorn JH. Prevention of intraoperative anesthesia accidents and related severe injury through safety monitoring. Anesthesiology. 1989 Apr;70(4):572-7.
- Hadzic A, Vloka J, Hadzic N, Thys DM, Santos AC. Nerve stimulators used for peripheral nerve blocks vary in their electrical characteristics. Anesthesiology. 2003;98(4):969-974.
- Gadsden JC, Choi JJ, Lin E, Robinson A. Opening injection pressure consistently detects needle-nerve contact during ultrasound-guided interscalene brachial plexus block. Anesthesiology. 2014;120(5):1246-1253.
- Tsai TP, Vuckovic I, Dilberovic F, et al: Intensity of the stimulating current may not be a reliable indicator of intraneural needle placement. Reg Anesth Pain Med 2008;33:207–210.
- Chan VWS, Brull R, McCartney CJL, Xu D, Abbas S, Shannon P. An Ultrasonographic and Histological Study of Intraneural Injection and Electrical Stimulation in Pigs. Anesthesia & Analgesia. 2007;104(5).