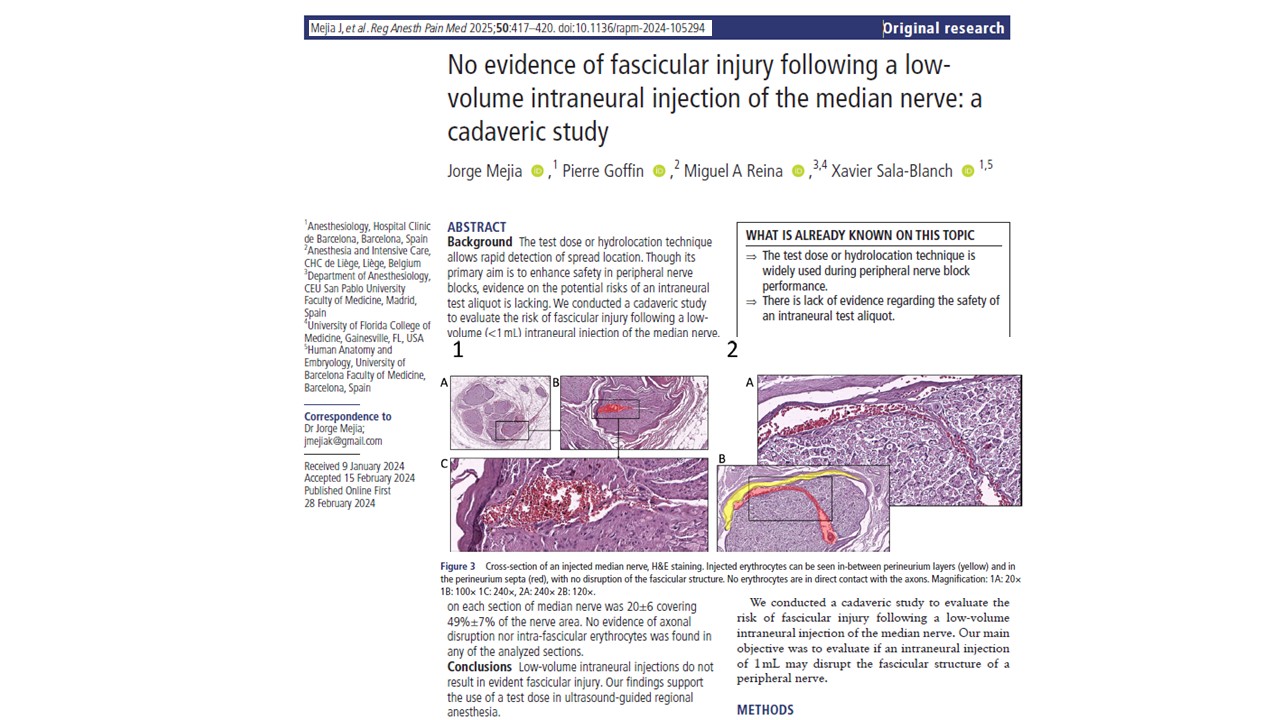
A recent cadaver-based investigation by Mejia et al. 2025, published in RAPM, provides new insights into the structural effects of low-volume intraneural injections in regional anesthesia. The study investigated whether administering a small volume of fluid, 1 mL, into the median nerve resulted in any fascicular damage. Despite longstanding concerns that intraneural injections can cause nerve injury, the study’s findings suggest that under controlled conditions, low-volume intraneural injections do not result in structural disruption of the nerve fascicles.
Background and rationale
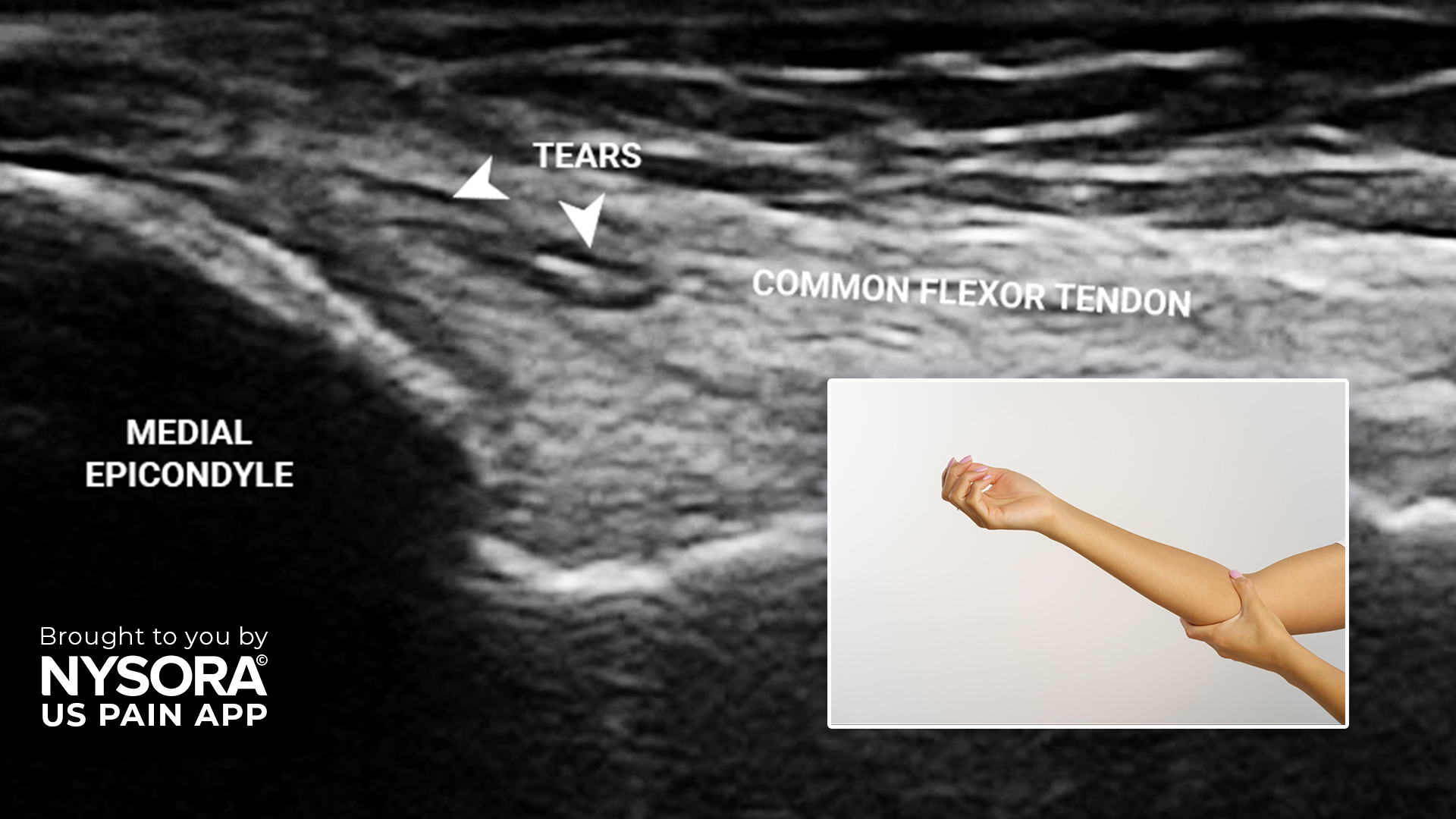
Peripheral nerve blocks (PNBs) are widely used in anesthetic practice for intraoperative and postoperative analgesia. Ultrasound guidance has improved the precision of these blocks, yet inadvertent intraneural injection remains a concern. Estimates suggest that intraneural needle placement occurs in 15% to 20% of cases using ultrasound guidance.
The test dose or hydrolocation technique involves injecting a small aliquot of fluid, typically less than 1 mL, into or around the nerve to confirm needle position. If swelling within the nerve is observed sonographically, the needle can be repositioned before administering a full anesthetic dose. While this method is intended to reduce risk, its safety profile has not been comprehensively evaluated, particularly concerning fascicular integrity.
This study was designed to assess whether a 1 mL intraneural injection into the median nerve leads to fascicular injury, using histological methods to detect any signs of perineurium disruption or intrafascicular injectate spread.
Study design and methodology
The study was conducted using ten fresh, unembalmed human cadaveric upper limbs. These specimens had no history of trauma, surgery, or neurological disease. The limbs were thawed and brought to room temperature before the procedures.
Step-by-step procedure
- Ultrasound identification:
- The median nerve was located in the forearm using a 6–13 MHz linear ultrasound transducer.
- The nerve was visualized between the deep and superficial flexor muscles.
- Injection protocol:
- A 22-gauge, 30° bevel insulated needle was inserted using an in-plane approach under continuous ultrasound visualization.
- Intraneural location was confirmed by visualizing nerve wall indentation, needle entry into the nerve, and nerve displacement during manipulation.
- A mixture containing methylene blue and heparinized blood was injected intraneurally at three sites along the nerve (proximal, mid, distal forearm).
- The injection rate was standardized at 10 mL/min using a syringe pump.
- Post-injection analysis:
- Nerves were dissected longitudinally, fixed in 10% formalin for four weeks, and then sectioned into 3 mm slices perpendicular to the nerve’s long axis.
- Each sample was stained with hematoxylin and eosin (H&E) and examined under light microscopy with magnification up to 800×.
Findings and observations
A total of 30 intraneural injections were performed, and 352 histological sections were analyzed. The study’s primary outcome was the presence or absence of fascicular injury, defined as:
- Perineurium or axonal disruption
- Presence of erythrocytes inside the nerve fascicles
Key results
- Sonographic evidence:
- All injections showed nerve swelling on ultrasound, indicating the spread of intraneural fluid.
- The extent of injectate spread averaged 2 cm in both the proximal and distal directions from the injection point.
- Histological findings:
- No disruption of the perineurium was observed in any sample.
- Erythrocytes, used as a marker of injectate location, were consistently found in the interfascicular adipose tissue but not within the fascicles themselves.
- Some sections showed erythrocytes between layers of the perineurium, but none in direct contact with axons.
- Spread distribution:
- Erythrocytes were present in the internal epineurium in 100% of samples and between perineurium layers in approximately 9%.
- No sample exhibited erythrocytes inside fascicles, suggesting that the injectate did not penetrate the innermost protective barriers.
Clinical context
These results provide histological evidence that a controlled, low-volume intraneural injection into the median nerve does not breach the perineurium or disrupt fascicular architecture. While sonographic signs, such as nerve swelling, are often treated as potential red flags, this study suggests that they do not necessarily correlate with fascicular damage when the injected volume is small and precisely administered.
The structural barriers within peripheral nerves, epineurium, perineurium, and endoneurium, provide substantial protection against intrafascicular infiltration. The perineurium, in particular, forms a dense, multilayered sheath that limits the spread of fluids under low-pressure conditions.
Additionally, the physical properties of injectate distribution play a role. Fluids injected into a solid structure tend to move along paths of least resistance. In this study, injectate moved preferentially into interfascicular fat and connective tissue, rather than penetrating into densely packed fascicles.
Limitations
While the findings are encouraging, the study’s authors note several limitations:
- Cadaveric model:
- The elasticity and tissue hydration in cadavers differ from those in live tissue, which may influence the spread patterns and mechanical properties.
- Nerve specificity:
- Only the median nerve was evaluated. Results may not generalize to other peripheral nerves with different fascicle-to-connective tissue ratios.
- Histological sensitivity:
- Although the analysis aimed to detect fascicular damage, very subtle injuries or transient inflammatory responses may have been missed.
- Functional outcomes:
- The study did not assess sensory or motor function post-injection, which would be necessary to fully evaluate clinical safety.
Implications for clinical practice
This study offers preliminary support for the continued use of low-volume test injections during ultrasound-guided regional anesthesia. When intraneural placement is identified early through sonographic monitoring, a 1 mL injection appears not to result in fascicular injury, at least from a structural standpoint.
The results suggest that careful technique and prompt identification of intraneural injection allow for safe adjustments, potentially reducing the risk of injecting larger volumes into vulnerable neural structures. This is particularly relevant in high-stakes environments such as operating rooms, where nerve injury can have significant consequences.
However, the decision to employ test doses should still take into account the individual patient, nerve anatomy, and procedural context. Additional research, particularly in live patients and across different nerves, is required to establish a comprehensive safety profile.
Conclusion
This cadaveric study contributes to the understanding of the effects of low-volume intraneural injections in peripheral nerve blocks. It demonstrates that, under controlled conditions, a 1 mL injection into the median nerve does not result in observable fascicular injury. While these findings are limited to structural analysis and a specific nerve, they provide a basis for further investigation and may help inform safer practices in regional anesthesia.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Mejia J, Goffin P, Reina MA, Sala-Blanch X. No evidence of fascicular injury following a low-volume intraneural injection of the median nerve: a cadaveric study. Reg Anesth Pain Med. 2025 May 6;50(5):417-420.Read more about intraneural injections and nerve injury in the Regional Anesthesia Module on the NYSORA360!