Chronic low back pain (CLBP) is one of the most debilitating musculoskeletal conditions worldwide. Affecting millions of individuals across all age groups, it contributes to reduced quality of life, work disability, and escalating healthcare costs. Among the various causes of CLBP, lumbar facet joint syndrome (FJS) accounts for 10–15% of chronic cases.
Recent advancements in interventional pain management have introduced various forms of radiofrequency (RF) treatments as alternatives to conventional therapies. These treatments target the nerves that innervate the lumbar facet joints, aiming to disrupt pain signals and restore function. However, clinicians have long debated which RF modality offers the most effective and sustainable relief.
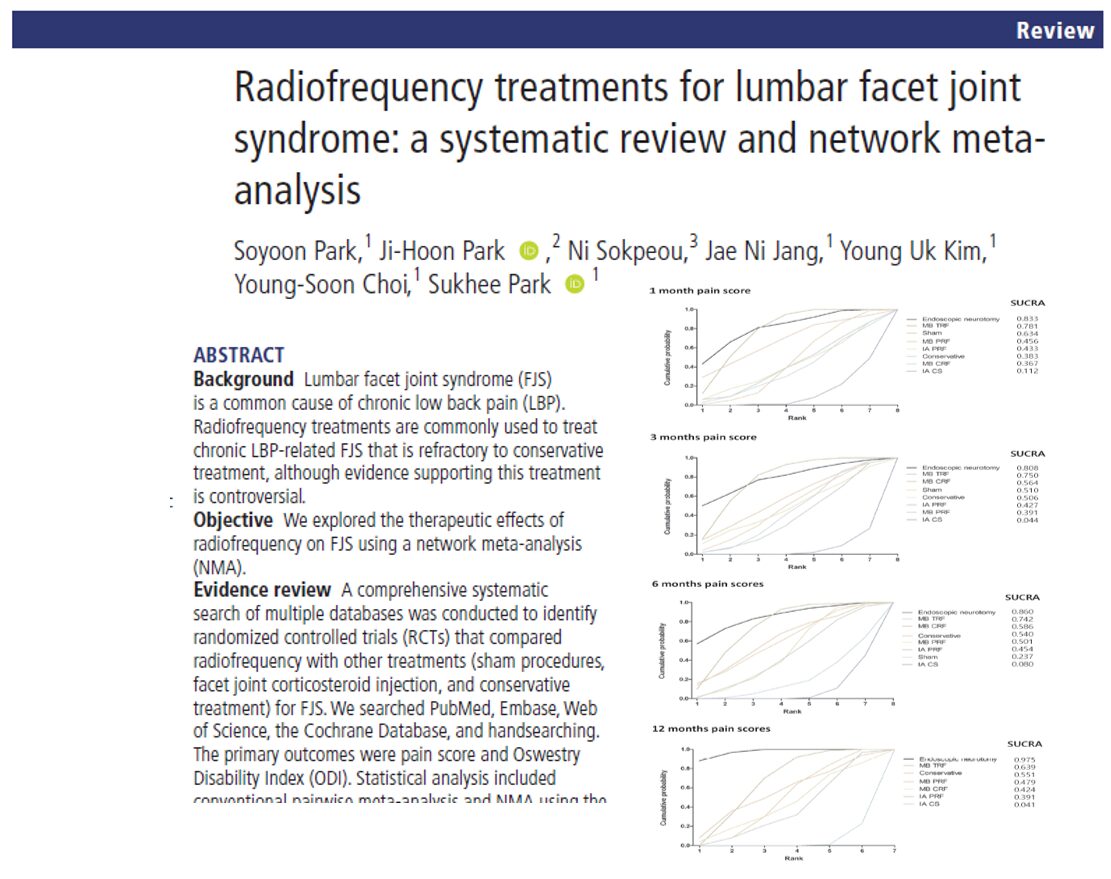
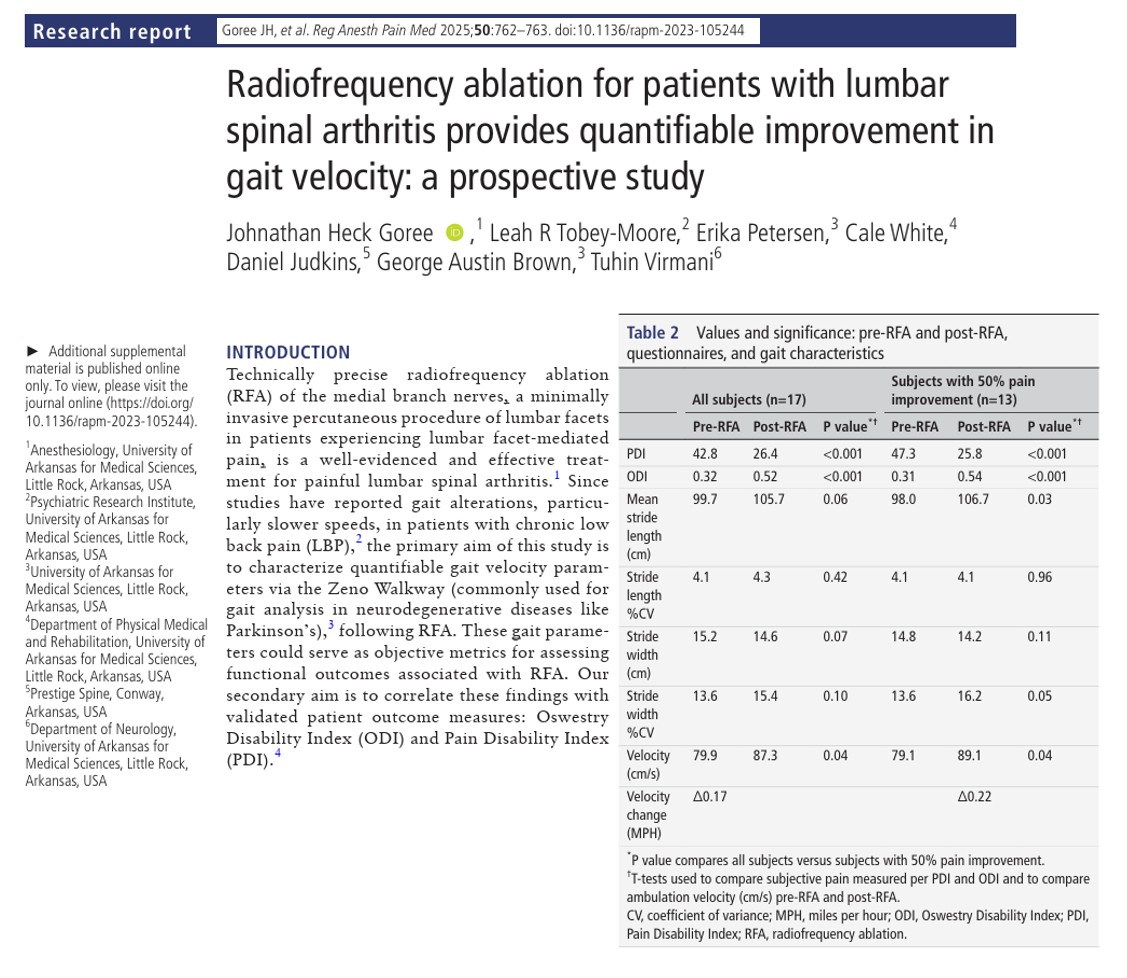
A new systematic review and network meta-analysis (NMA) published in Regional Anesthesia and Pain Medicine by Park et al. (2025) answers this critical question. The study evaluates the comparative effectiveness of four types of RF treatments: traditional RF (TRF), pulsed RF (PRF), cooled RF (CRF), and endoscopic neurotomy, against conservative management, sham procedures, and intra-articular corticosteroid (IA CS) injections.
Understanding lumbar facet joint syndrome
Facet joints, also known as zygapophysial joints, are small paired joints located at the back of the spine. They allow for flexibility while stabilizing the vertebral column. Over time, degeneration, inflammation, or injury can lead to facet joint arthropathy, resulting in lumbar FJS.
Key clinical features of FJS:
- Localized lower back pain, often worsened by extension or rotation
- Referred pain to the buttocks or posterior thighs
- Stiffness in the morning or after prolonged inactivity
- Pain relief with flexion or forward bending
The gold standard for diagnosis remains medial branch blocks (MBB) with local anesthetic, confirming the facet joint as the source of pain.
Radiofrequency ablation: a modern pain solution
Radiofrequency ablation (RFA) is a minimally invasive technique that uses heat or electrical currents to disable sensory nerves supplying the facet joints. It’s often used when conservative treatments fail.
Four types of RF treatments analyzed:
- Traditional RF (TRF): Continuous thermal lesioning to ablate medial branch nerves
- Pulsed RF (PRF): Intermittent high-voltage currents with minimal heat, preserving nerve structure
- Cooled RF (CRF): Expands the lesion size through controlled cooling
- Endoscopic neurotomy: Direct visualization and ablation of medial branches using an endoscope
Study methodology
- Number of RCTs included: 25
- Total participants: 1,969
- Time points evaluated: 1, 3, 6, and 12 months post-treatment
- Outcomes assessed:
- Pain reduction (measured using VAS and NRS)
- Functional improvement (measured via Oswestry Disability Index, ODI)
- Statistical method: Frequentist network meta-analysis using SUCRA scores for treatment ranking
Key findings
1. Endoscopic neurotomy is the most effective treatment
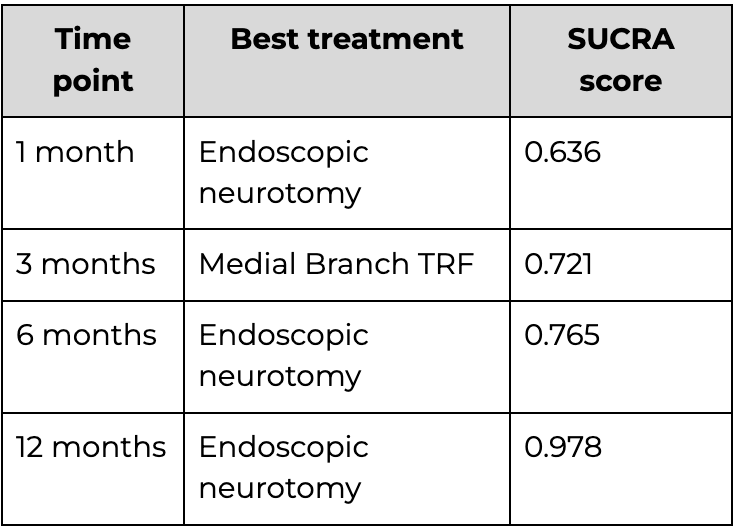
Across all four time points, endoscopic neurotomy achieved the highest SUCRA (Surface Under the Cumulative Ranking) scores for both pain relief and disability improvement.
Pain reduction SUCRA scores:
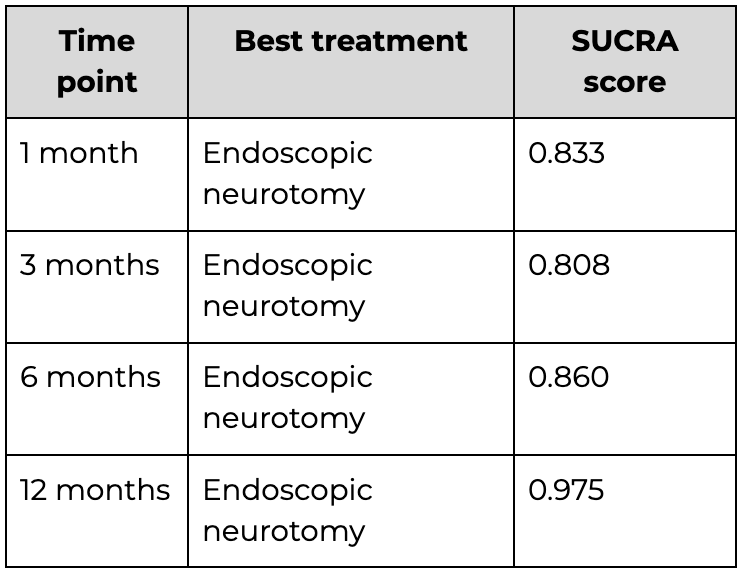
ODI (functional improvement) SUCRA scores:
How do other treatments compare?
Traditional RF (TRF)
- Ranked second or third consistently across time points
- Effective in reducing pain and improving ODI, especially mid-term
- Preferred for patients not eligible for endoscopic treatment
Pulsed RF (PRF)
- Less effective in long-term pain control compared to TRF and endoscopic
- Still demonstrated functional improvement at 6 and 12 months
Cooled RF (CRF)
- Moderate efficacy in pain reduction
- Fewer studies included—data quality considered lower
IA corticosteroid injections
- Short-term pain relief only
- Performed significantly worse at all time points in both pain and function
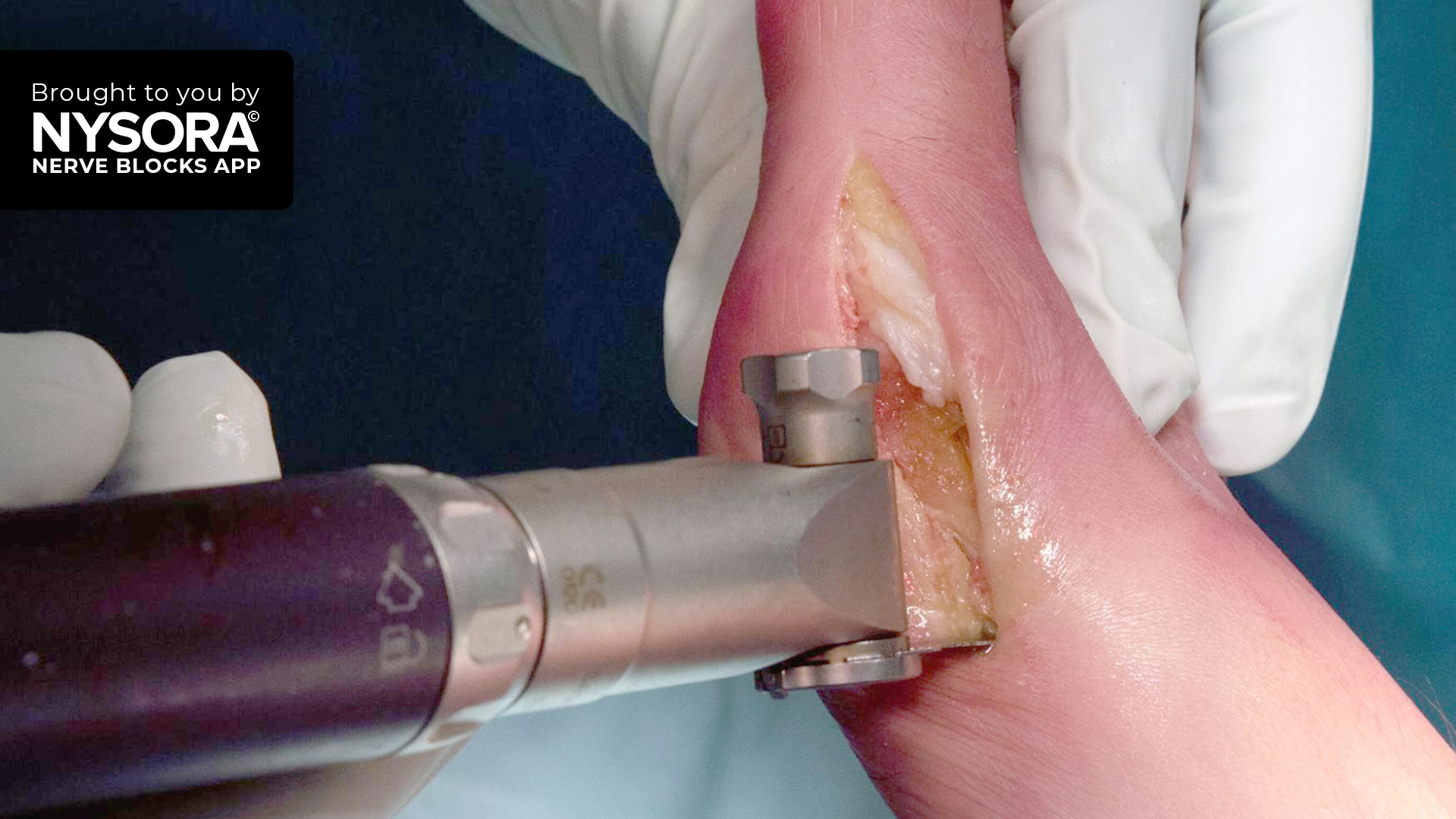
How are RF treatments performed?
5-step process for TRF/PRF:
- Patient positioning: Usually prone on the procedure table.
- Imaging guidance: Fluoroscopy or CT is used to guide the RF needle.
- Sensory and motor testing: Ensures correct nerve targeting.
- Lesioning: RF current applied for 60–90 seconds.
- Post-procedure monitoring: Observe for pain relief and adverse reactions.
Endoscopic neurotomy involves the insertion of a working channel and camera for direct visualization.
Clinical implications
This study has significant consequences for clinical practice:
- Endoscopic neurotomy should be considered the preferred option for patients with confirmed lumbar FJS and chronic symptoms.
- Medial branch TRF and PRF are effective alternatives in specific patient populations.
- IA CS injections may be phased out of long-term treatment strategies in favor of RF-based interventions.
Limitations to consider
Despite strong methodology, several limitations must be acknowledged:
- Heterogeneity in intervention protocols and patient populations
- Lack of long-term data beyond 12 months
- Variability in outcome measures across studies
- Publication bias cannot be ruled out
Final recommendations for clinicians
- Assess each patient individually. Not all patients may qualify for endoscopic procedures.
- Consider comorbidities, prior surgeries, and insurance coverage when recommending treatment.
- Educate patients about the risks and benefits of RF options, including realistic timelines for improvement.
- Follow-up is critical. Pain relief may take weeks to peak, and reassessment ensures optimal outcomes.
Future perspectives
To further improve FJS management, researchers suggest:
- Conducting standardized, high-quality RCTs with long-term follow-up
- Investigating mechanisms of nerve regeneration and ablation
- Identifying biomarkers or imaging tools to predict treatment response
- Comparing the cost-effectiveness between RF types and surgery
Conclusion
This network meta-analysis is the most comprehensive comparison of RF therapies for lumbar facet joint syndrome to date. It confirms that endoscopic neurotomy is the most effective treatment, followed by medial branch traditional and pulsed RF. The findings not only guide clinical decision-making but also prompt a reevaluation of outdated treatment algorithms, particularly the overuse of corticosteroid injections in chronic FJS.
As more high-quality research emerges, personalized RF treatment strategies will likely become the cornerstone of chronic low back pain management.
For more information, refer to the full article in RAPM.
Park S, Park JH, Sokpeou N, et al. Radiofrequency treatments for lumbar facet joint syndrome: a systematic review and network meta-analysis. Reg Anesth Pain Med. 2025;50(11):879-890. Published 2025 Nov 5.
For a detailed guide on ultrasound-guided lumbar facet joint injections, download NYSORA’s Ultrasound Pain app!