IV Antihypertensives and Brain Blood Flow
Intravenous (IV) antihypertensive therapies are frontline tools in managing acute hypertension, particularly in intensive care units (ICUs), emergency departments, and perioperative settings. Rapid control of dangerously high blood pressure is essential to prevent catastrophic events such as stroke, myocardial infarction, or aortic dissection. However, this rapid intervention introduces another clinical challenge: how these medications affect cerebral blood flow (CBF) and whether they compromise neurocognitive function.
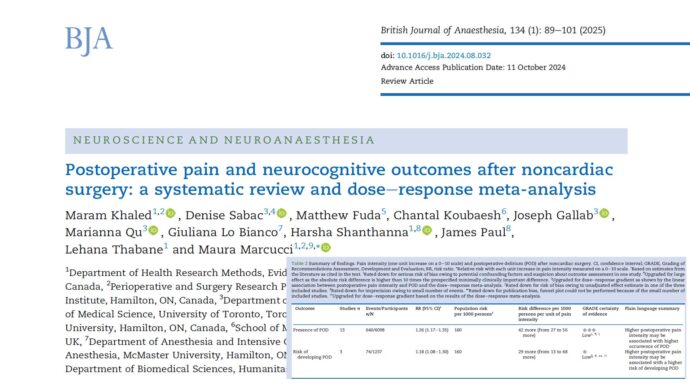
A landmark 2025 systematic review and meta-analysis published in the British Journal of Anaesthesia evaluated this concern across a wide array of clinical contexts. This comprehensive investigation, which synthesized data from 50 studies and 73 patient subgroups, provides the clearest picture yet of how various IV antihypertensives affect brain perfusion and highlights the agents that require cautious use.
Key findings from the study
The systematic review uncovered important nuances regarding the effects of IV antihypertensives on cerebral circulation:
- Significant CBF reductions occurred predominantly in awake, normotensive individuals treated with nitroprusside or nitroglycerin.
- Median CBF drop: 14%
- Median mean arterial pressure (MAP) reduction: 17%
- Other agents, including labetalol, nicardipine, clevidipine, and metoprolol, demonstrated no statistically significant impact on CBF across normotensive, hypertensive, and intracranial pathology cohorts.
- Cerebral autoregulation remained intact in most cases, suggesting that the brain can buffer against moderate reductions in systemic blood pressure without compromising perfusion.
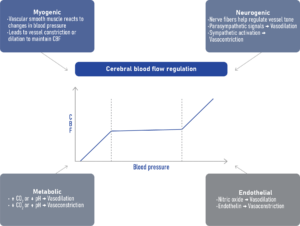
Understanding cerebral autoregulation
Cerebral autoregulation is the brain’s intrinsic ability to maintain consistent blood flow despite fluctuations in arterial blood pressure (ABP). It does so by adjusting the diameter of cerebral blood vessels:
- Vasodilation occurs when ABP drops.
- Vasoconstriction occurs when ABP rises.
This mechanism protects the brain from hypo- or hyperperfusion. However, its effectiveness is not absolute. In certain pathological states, such as traumatic brain injury, stroke, or severe systemic inflammation, autoregulation may be impaired, making the brain more susceptible to perfusion changes triggered by antihypertensive therapy.
Which drugs are most impactful?
Agents showing significant CBF reduction:
These medications require caution, particularly in patients with intact autoregulation but without high baseline ABP:
- Nitroprusside
- Nitroglycerin
Why they matter: These are potent venodilators that reduce cardiac preload and systemic vascular resistance. In doing so, they may decrease cardiac output and, subsequently, cerebral perfusion, especially when used aggressively or in normotensive individuals.
Agents with minimal CBF impact:
These drugs are generally considered safer options for cerebral perfusion:
- Labetalol
- Nicardipine
- Metoprolol
- Clevidipine
Why they matter: Their mechanisms, often involving balanced alpha and beta blockade or arterial vasodilation, tend to preserve cerebral perfusion pressures without dramatic shifts in preload or cardiac output.
Common clinical scenarios
1. Intraoperative controlled hypotension
- Purpose: Minimize blood loss during surgery.
- Risk: Hypotension can lead to inadequate cerebral perfusion, especially in elderly or vulnerable patients.
- Safe strategy: Use nicardipine or clevidipine for targeted reductions with preserved CBF.
2. Hypertensive emergencies
- Purpose: Prevent target-organ damage in crises like aortic dissection or hypertensive encephalopathy.
- Risk: Over-aggressive MAP reduction can cause cerebral hypoperfusion.
- Recommendation: Gradual BP reduction (not more than 25% within the first hour).
3. Acute stroke post-thrombectomy
- Purpose: Limit reperfusion injury and cerebral edema.
- Risk: Excessive BP lowering can worsen ischemia in penumbral tissue.
- Evidence: Recent trials (e.g., ENCHANTED2/MT, BP-TARGET) caution against intensive BP targets due to worsened outcomes.
Clinical takeaway:
- Aim for balance. Control blood pressure without sacrificing brain perfusion.
- Tailor therapy. Match the drug to the patient’s physiological and neurological status.
- Monitor closely. Recognize the early signs of CBF compromise before neurocognitive damage occurs.
Final thoughts
This comprehensive review underscores that while most IV antihypertensive agents are safe regarding cerebral blood flow, certain drugs like nitroprusside and nitroglycerin require cautious use in specific scenarios. Maintaining a balance between effective BP control and preserving cerebral perfusion is essential for optimal neuroprotection.
Reference: Meacham KS. et al. Impact of intravenous antihypertensive therapy on cerebral blood flow and neurocognition: a systematic review and meta-analysis. Br J Anaesth. 2025;134:713-726.
For more information on this topic, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.