Living donor liver transplantation (LDLT) is a major surgical procedure that saves lives but also presents significant challenges, especially regarding postoperative pain management. While enhanced recovery after surgery (ERAS) protocols emphasize multimodal analgesia, the evidence supporting specific strategies has historically been weak. A recent systematic review by Saglietti et al. (2025) offers a comprehensive look at evolving analgesic techniques and their role in improving outcomes in LDLT patients.
Why pain management in liver transplant matters
Effective perioperative pain control is critical for:
- Early mobilization
- Prevention of postoperative complications
- Avoidance of chronic pain syndromes
- Improved graft survival and patient outcomes
However, despite its importance, there’s considerable variability in analgesic practices due to a lack of high-quality evidence.
Current challenges and clinical practice gaps
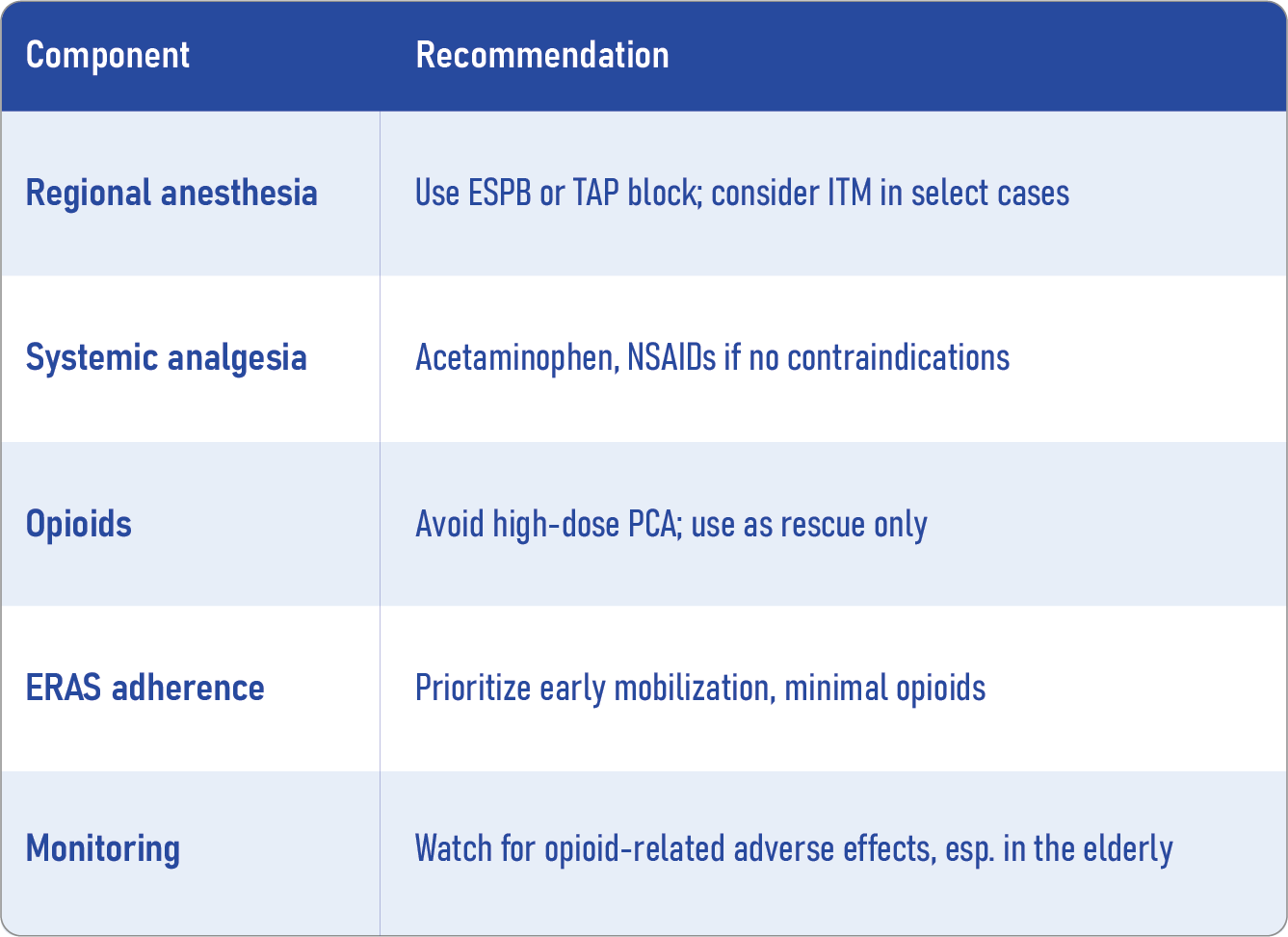
- High opioid reliance: Over 80% of LDLT patients still receive intravenous patient-controlled analgesia (PCA) with morphine—despite known risks such as delirium and gastrointestinal ileus.
- Limited guideline strength: ERAS guidelines (2022) suggest TAP blocks but discourage thoracic epidurals, based on low-quality evidence.
- Lack of comparative studies: Until now, few studies have directly compared the efficacy of different regional anesthesia techniques.
Recent evidence: what does the review say?
Saglietti et al. systematically analyzed studies published between 2022 and 2024. Out of 124 papers, only three studies met the inclusion criteria, each focusing on a distinct regional anesthesia technique.
Study: Assefi et al. (2023)
- Design: Before-and-after study
- Patients: 200 (73 received TAP block, 127 did not)
- Findings:
- 24 mg reduction in morphine milligram equivalents (MMEs)
- No significant difference in pain scores
- 24 mg reduction in morphine milligram equivalents (MMEs)
- Interpretation: TAP block may reduce opioid need, though pain relief benefits were unclear.
-
Intrathecal morphine (ITM)
Study: Kwon et al. (2023)
- Design: Retrospective study with propensity score matching
- Patients: 742 (336 included after matching)
- Dose: 400 mcg morphine intrathecally
- Key outcomes:
- Significantly lower pain scores and MME usage postoperatively
- Laparoscopic approach showed better results than open surgery
- Significantly lower pain scores and MME usage postoperatively
- Caveats:
- Long recruitment period (12 years)
- High ITM dose raises safety concerns
- Long recruitment period (12 years)
Study: Uludag Yanaral et al. (2024)
- Design: Randomized controlled trial
- Patients: 42 (20 received ESPB)
- Results:
- 40% less fentanyl consumption
- Reduced need for rescue opioids
- Less nausea
- Dynamic pain scores improved, though static scores did not
- Implication: ESPB appears safe, effective, and opioid-sparing
Key takeaways
- Regional blocks are underused despite their clear opioid-sparing benefits.
- ESPB appears most promising among the studied blocks.
- More high-quality RCTs are needed to refine analgesic protocols.
- Pain management must be individualized, balancing efficacy with safety.
The field of pain management in liver transplantation is slowly evolving. This latest review underscores the need for tailored, evidence-based approaches. Techniques like erector spinae plane blocks and intrathecal morphine (in lower doses) show promise in reducing opioid reliance and enhancing recovery. Future research will be pivotal in shaping robust guidelines and optimizing care for living liver donors and recipients alike.
Reference: Saglietti F et al. Analgesia for living donor liver transplant: a systematic review of recent trials. Curr Opin Anaesthesiol. 2025;38:452-456.
This content is also available in the NYSORA Anesthesia Assistant App — your smart, expert-reviewed tool for:
- Point-of-care decisions: Instant, evidence-based guidance
- AI support (MAIA): Tools like DoseCalc and Case Manager
- Weekly updates: Protocols, tips, and exam-ready knowledge
Built on science, reviewed by experts — smarter (and safer) than a web search.
Download the AA App now to put trusted anesthesia guidance in your pocket.