Learning objectives
- Manage a patient with obstructive sleep apnea (OSA) in the perioperative period
Definition and mechanisms
- Obstructive sleep apnea (OSA) is a disorder in which a person frequently stops breathing during their sleep due to obstruction of the upper airway
- This obstruction is caused by an inadequate motor tone of the tongue and/or airway dilator muscles and is exaggerated by excessive adipose tissue
- OSA accompanied by excessive daytime sleepiness is termed OSA syndrome (OSAS)
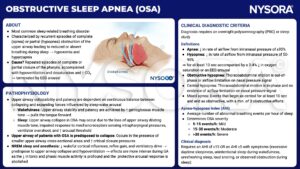
Background
- OSA affects 5-10% of the general population but is twice as prevalent in the population undergoing surgery
Predisposing factors
- Obesity
- Age 40-70
- Male gender
- Alcohol abuse
- Smoking
- Pregnancy
- Low physical activity
- Unemployment
- Neck circumference > 40 cm
- Tonsillar and adenoidal hypertrophy
- Craniofacial abnormalities (e.g., Pierre Robin, Down’s syndrome)
- Neuromuscular disease
Medical consequences
OSA is associated with
Neurocognitive
- Increased risk of cerebrovascular accidents with poorer outcomes
- Psychosocial problems
- Decreased cognitive function
- Depression
Endocrine
- Impaired glucose tolerance
- Dyslipidemia
- Increased adrenocorticotropic hormone and cortisol concentrations
- Testicular and ovarian dysfunction
Cardiovascular
- Hypertension
- Brady- and tachyarrhythmias
- Pulmonary hypertension
- Congestive heart failure
- Myocardial infarction
Treatment
- Weight loss is the preferred treatment for obese patients with OSA
- Continuous positive airway pressure (CPAP) therapy may reduce the risk of cardiac and cerebrovascular events, this effect is most pronounced in non-obese patients
- Surgical uvulo-palato-pharyngoplasty and various supportive airway devices promoting mandibular advancement can be offered to selected patients but have lower efficacy than weight loss and CPAP
Anesthesiologic implications
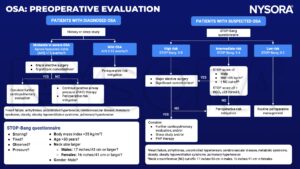
- Assess the patient preoperatively for conditions associated with OSA
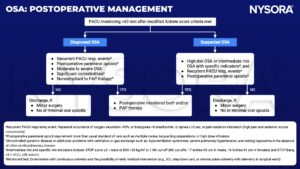
- Continue CPAP treatment during hospital admission and in the recovery room
- Avoid the administration of sedative medication unless the patient is properly monitored
- OSA is associated with difficult intubation so plan accordingly
- Use locoregional techniques where possible
Suggested reading
- Martinez G, Faber P. Obstructive sleep apnoea. Continuing Education in Anaesthesia Critical Care & Pain. 2011;11(1):5-8.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com