New Insights into the Spread of Costoclavicular Brachial Plexus Block: A Cadaveric Study
A costoclavicular block anesthetizes the brachial plexus at the level of the cords (i.e., lateral, medial, and posterior cords) resulting in anesthesia of the arm below the shoulder. The technique is emerging as the preferred choice for upper extremity surgery when diaphragm function needs to be preserved and a complete brachial plexus block is needed.
Understanding the anatomical spread of injectate during a costoclavicular brachial plexus block is essential for improving the effectiveness and safety of this regional anesthesia technique. Despite its growing use, limited data exist on the anatomical spread of the injectate when performing a costoclavicular brachial plexus block. The study conducted by Koyyalamudi et al. in 2021 offers valuable insights into how this block spreads within the brachial plexus, thereby sparing the phrenic nerve, a common complication associated with interscalene blocks.
Methodology
- Five ultrasound-guided costoclavicular brachial plexus block injections were performed on three unembalmed human cadavers.
- Each block was executed using 20 mL of 0.1% methylene blue, allowing clear visualization of the spread within the brachial plexus.
- The cadavers were dissected from the level of C4 to the lower axilla to assess the extent of dye distribution, particularly focusing on the suprascapular nerve, the roots, trunks, divisions, and cords of the brachial plexus, as well as the phrenic nerve.
Key Findings
- The dye consistently spread cephalad to the supraclavicular space, staining all trunks, cords, and divisions of the brachial plexus. The suprascapular nerve was also consistently stained in all injections.
- The phrenic nerve was spared in all five injections, supporting the notion that costoclavicular brachial plexus block can be performed without the risk of causing hemidiaphragmatic paresis. This finding aligns with clinical observations that a costoclavicular brachial plexus block is associated with a significantly lower incidence of diaphragmatic paralysis than an interscalene brachial plexus block.
- While the axillary and radial nerves were stained in all injections, the staining of the ulnar, musculocutaneous, and median nerves varied. This variability suggests that while the costoclavicular brachial plexus block provides robust coverage for shoulder and upper limb analgesia, the extent of sensory blockade may vary depending on the specific nerve targets.
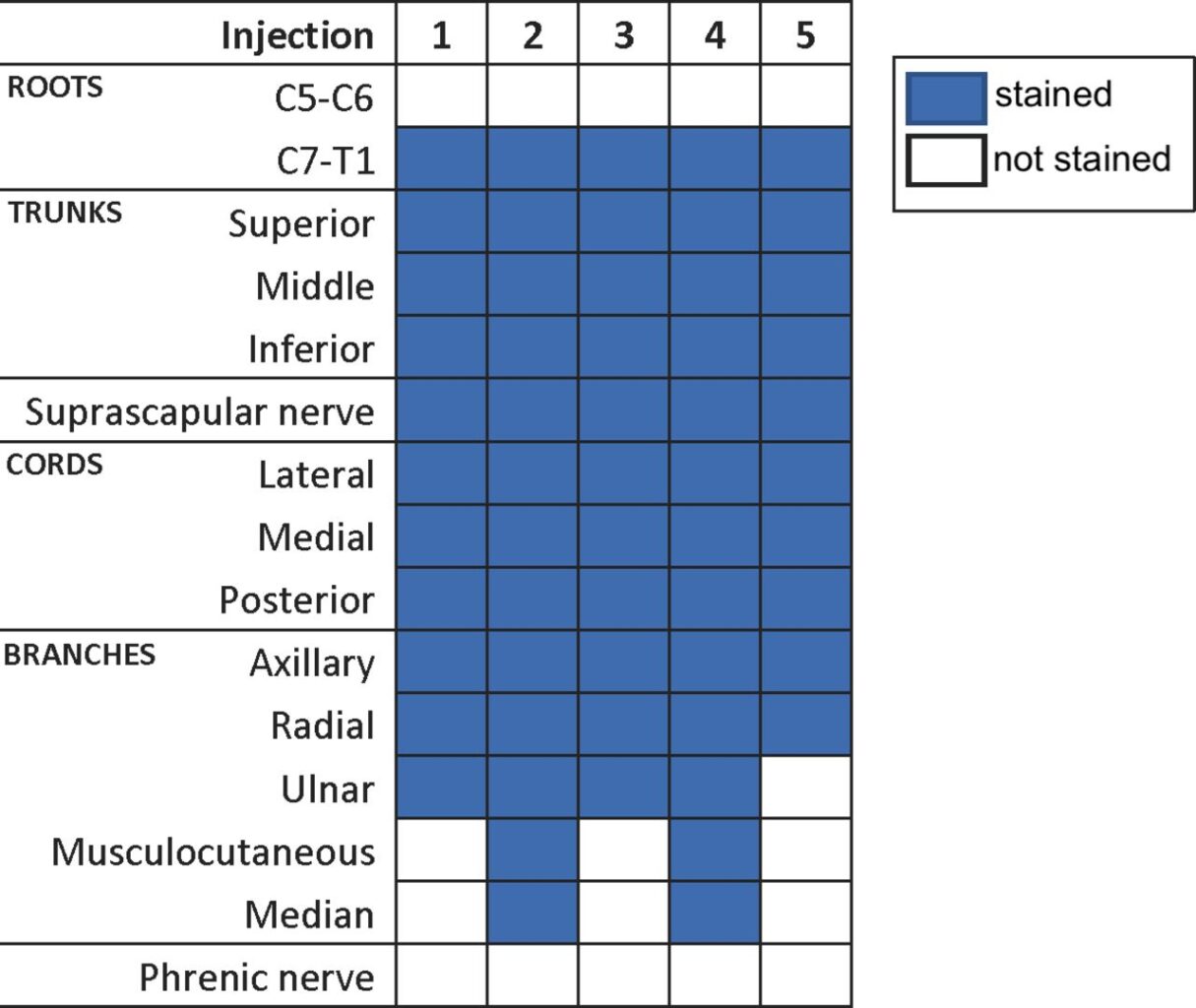
Brachial plexus structures were stained in each of the injections.
Source of the image: Koyyalamudi et al. Reg Anesth Pain Med. 2021 Jan;46(1):31-34.
Limitations
The study’s limitations include its small sample size and the fact that it was conducted on cadaveric specimens, which may not fully replicate in vivo conditions. Additionally, using a single injection site may not reflect the variations that could occur with different techniques or multiple injection sites.
Conclusion
The consistent sparing of the phrenic nerve confirms the safety of costoclavicular brachial plexus block in procedures where diaphragmatic function must be preserved, such as in patients with compromised pulmonary function. The variability in the staining of terminal branches indicates that anesthesiologists should be mindful of the potential need for additional blocks or higher anesthetic volumes in certain cases.
For more detailed information, refer to the full article in Regional Anesthesia & Pain Medicine.
Koyyalamudi V, Langley NR, Harbell MW, Kraus MB, Craner RC, Seamans DP. Evaluating the spread of costoclavicular brachial plexus block: an anatomical study. Reg Anesth Pain Med. 2021;46(1):31-34.
Here are the 3 steps we follow when performing a costoclavicular brachial plexus block
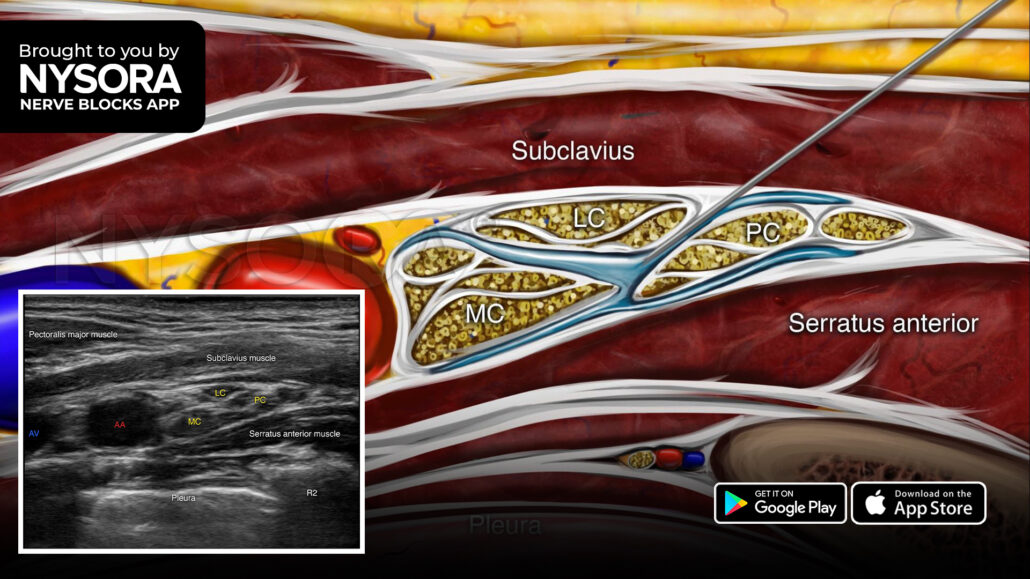
- Place the transducer in the medial infraclavicular fossa parallel and next to the clavicle to identify the axillary artery.
- Identify the brachial plexus cords (i.e., lateral, medial, and posterior cords) lateral to the axillary artery. The cords are visualized as hyperechoic oval structures arranged in a triangular shape.
- Insert the needle in-plane, from lateral to medial, between the three cords (ideally between the lateral and posterior cords) and inject 15-20 mL of local anesthetic.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!