Case study: Cancer-related lower abdominal and pelvic pain
Cancer-related chronic pain is a debilitating condition that can significantly impact a patient’s quality of life. In this article, we will explore the case of a 55-year-old woman with cervical uterine malignancy and severe lower abdominal and pelvic pain. We will focus on her diagnosis, pain management, and the use of a superior hypogastric plexus neurolytic block to alleviate her chronic pain. This procedure offers a targeted approach for managing pain associated with pelvic malignancies.
Case presentation
A 55-year-old woman presented with persistent lower abdominal and pelvic pain. She had been diagnosed with moderately differentiated non-keratinizing squamous cell carcinoma of the uterine cervix six months prior. Despite receiving extensive chemotherapy and radiotherapy, her pain had escalated, becoming a significant challenge in her treatment journey.
- Diagnosis: Cervical uterine malignancy.
- Previous treatments:
- 5 sessions of chemotherapy
- 20 sessions of radiotherapy
Pain characteristics
- Type: Severe, constant, with episodes of shooting, stabbing, and pressure-like sensations.
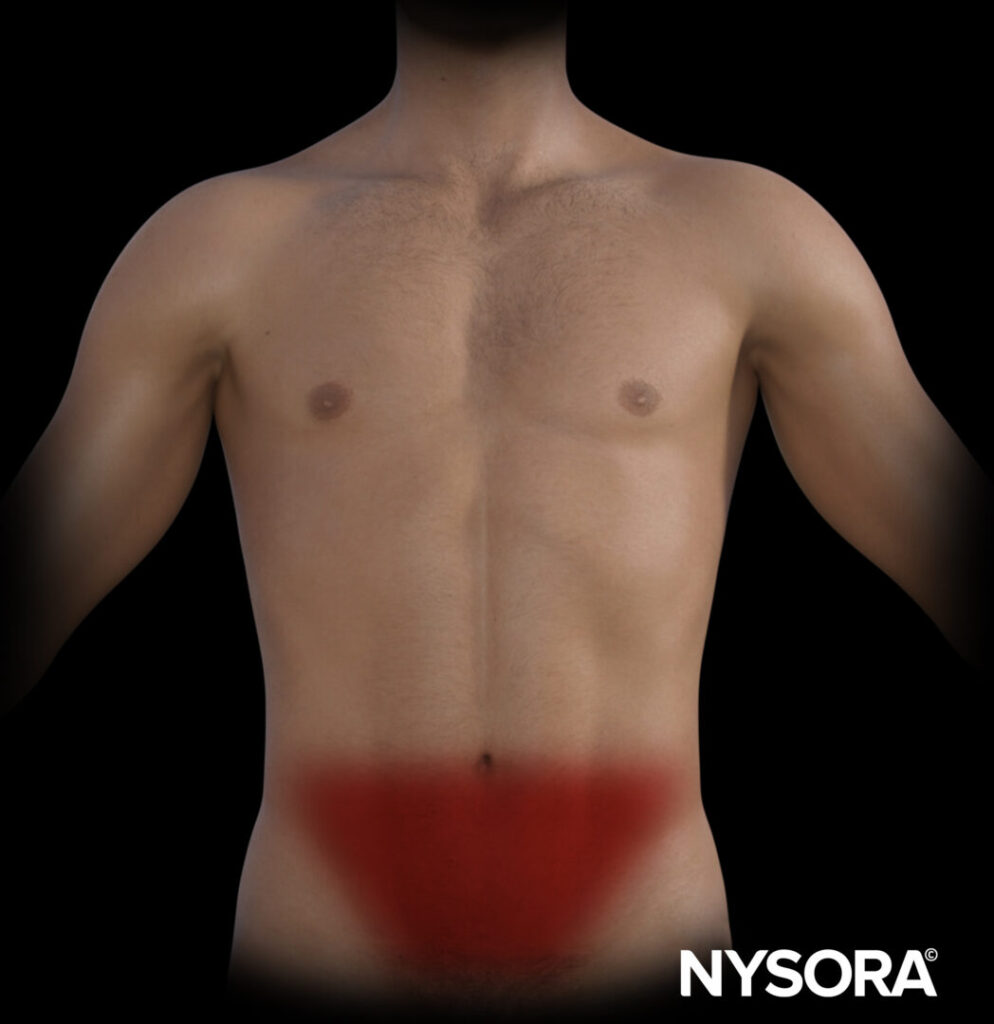
- Location: Lower abdomen and pelvis.
- Intensity: Baseline pain was rated at 7-8/10 on the Numerical Rating Scale (NRS), with peaks reaching 10/10 during episodes of excruciating pain.
- Duration: Episodes lasting for several seconds occurred multiple times per day, severely impacting her quality of life.
Current pain management
The patient’s pain was being managed with a multimodal approach, including:
- Gabapentin: 600 mg orally every eight hours.
- Duloxetine: 60 mg orally once daily.
- Methadone: 5 mg orally every eight hours.
- Paracetamol: 1000 mg orally every eight hours.
Despite this regimen, her pain remained challenging to control, particularly the breakthrough episodes, which were unresponsive to conventional pain medications.
Physical examination and imaging
- Physical exam: Revealed deep tenderness in the lower abdomen with organomegaly. Neurological examination of the legs was normal.
- MRI findings: Showed a large mass in the lower uterine cervix and upper vagina, with additional masses identified in the iliac, para-aortic, and adnexal regions, consistent with metastatic spread.
Diagnosis
The patient was diagnosed with cancer-related chronic lower abdominal and pelvic pain due to the malignancy. The pain was linked to tumor invasion and compression of surrounding pelvic structures.
Treatment: Superior hypogastric plexus neurolytic block
Given the inadequacy of pharmacological pain control, the decision was made to perform a superior hypogastric plexus neurolytic block, a procedure known for its efficacy in managing pelvic pain related to malignancies.
Indications
This procedure is indicated in patients with:
- Chronic pelvic pain due to cancer, particularly in cases involving cervical, ovarian, or colorectal malignancies.
- Pain refractory to medical management, as in this patient’s case, where conventional treatments failed to provide adequate relief.
Procedure
- Monitoring:
- The patient’s heart rate, blood pressure, and oxygen saturation are monitored throughout the procedure.
- Premedication:
- Midazolam: 0.1 mg/kg IV to provide mild sedation.
- Fentanyl: 1 µg/kg IV to manage any discomfort.
- Cephazolin: 2 g IV for antimicrobial prophylaxis to reduce infection risk.
- Patient positioning:
- The patient is placed in a prone position with a pillow under the abdomen to allow proper access to the lower spine.
- Fluoroscopic guidance:
- Fluoroscopy is used to identify the L5-S1 interdiscal space. The fluoroscope is angled obliquely (15°-25°) for the best view of the disc space.
- Needle insertion:
-
- A 22-gauge, 150 mm Quincke spinal needle is introduced 5-7 cm lateral to the midline using a coaxial (tunnel vision) technique.
- The needle is advanced through the disc space, and saline is injected to confirm the loss of resistance, ensuring the correct position.
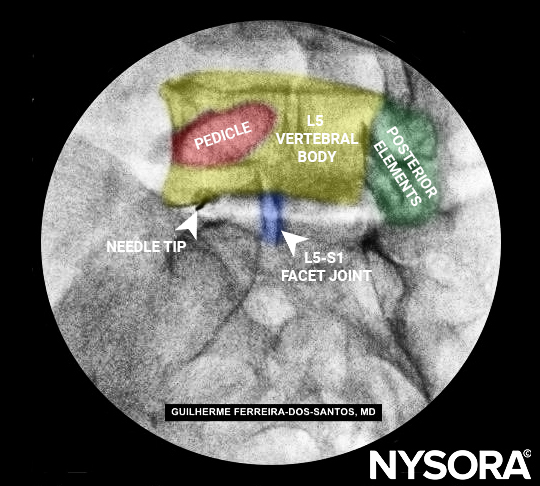
Tunnel vision (co-axial) introduction of the 22 gauge, 150 mm Quincke spinal needle lateral to the inferior aspect of the facet joint, approximately 5 to 7 cm lateral from the midline.
6. Contrast dye:
-
- 3 mL of contrast dye is injected to confirm the correct placement of the needle tip in the prevertebral space under direct fluoroscopic view.
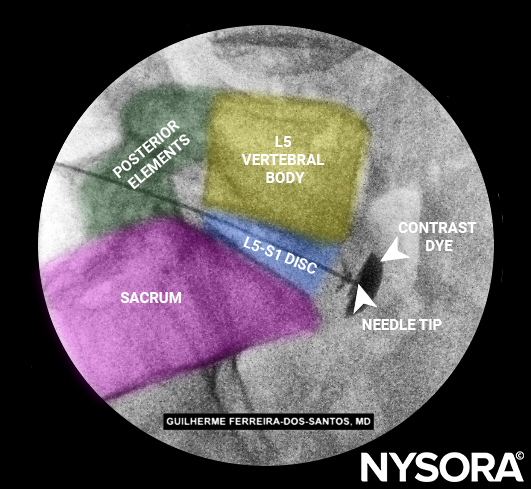
Contrast spread under direct fluoroscopy (lateral view), confirming adequate position of the needle tip in the prevertebral space, outside the L5-S1 disc.
7. Injection of neurolytic agent:
-
- 10 mL of 6% aqueous phenol is injected, followed by 1 mL of sterile saline to ensure proper distribution of the neurolytic agent.
Patient outcome
Immediate post-procedure results
- Within an hour of the procedure, the patient’s baseline pain reduced significantly from NRS 7-8 to NRS 4.
- The frequency and intensity of excruciating pain episodes decreased by 50%, offering significant relief.
Two-week follow-up
- The patient reported a stable baseline pain level of NRS 4.
- The breakthrough episodes had further decreased, improving her daily functioning and quality of life.
Conclusion
Cancer-related pelvic pain is a complex and challenging condition to manage. In this case, a 55-year-old woman with cervical uterine cancer experienced significant pain relief following a superior hypogastric plexus neurolytic block. This procedure offers an effective option for patients whose pain is unresponsive to medication. With proper technique and monitoring, the superior hypogastric plexus block can improve the quality of life for patients suffering from cancer-related pelvic pain.
Interested in more details about this procedure? Download NYSORA’s Pain Rx App to discover more!