Alain Borgeat, Matthew Levine, Malikah Latmore, Sam Van Boxstael, and Stephan Blumenthal
INTRODUCTION
The first brachial plexus blocks were performed by William Stewart Halsted, in 1885, at the Roosevelt Hospital in New York City. In 1902, George Washington Crile described an “open approach” to expose the (axillary) plexus facilitating direct application of cocaine. The need for surgical exposure of the brachial plexus led to limited clinical utility of this technique.
This changed in the early 1900s when percutaneous access to the brachial plexus was first described. In 1925, July Etienne1 reported the successful block of the brachial plexus by inserting a needle halfway between the lateral border of the sternocleidomastoid muscle and the anterior border of the trapezius muscle at the level of the cricothyroid membrane, making a single injection in the area around the scalene muscles.
This approach was most likely the first clinically useful interscalene block technique. In 1970, Alon Winnie described the first consistently effective and technically suitable percutaneous approach to the brachial plexus block. The technique involved palpating the interscalene groove at the level of the cricoid cartilage and injecting local anesthetic between the anterior and middle scalene muscles. Winnie’s approach was modified over the years to include slight variations to the technique such as perineural catheter placement. However, the success of this approach and the widespread adoption of the interscalene brachial plexus block as the “unilateral spinal anesthesia for the upper extremity,” should be credited solely to Alon Winnie.
More recently, the introduction of ultrasound-guided techniques has allowed for additional refinements and improved block consistency with reduced local anesthetic volumes.(see Ultrasound-Guided Interscalene Brachial Plexus Block)
Indications
The interscalene block is indicated for procedures on the shoulder and proximal humerus as well as the lateral two thirds of the clavicle. The interscalene block can also be utilized for surgery of the arm or forearm; however, the higher incidence of incomplete block of the inferior trunk with this technique may provide inadequate analgesia in the ulnar distribution. The patient’s positioning and comfort, the surgeon’s preferences, and the duration of surgery may necessitate coadministration of a general anesthetic. An interscalene catheter may be inserted for prolonged postoperative analgesia (Table 1).
TABLE 1. Single-injection vs the choice of technique: interscalene catheter according to surgery.
| Type of Surgery | Type of Block Single-Injection | Catheter |
|---|---|---|
| Open Surgery | ||
| Arthroplasty | + | + |
| Rotator cuff repair | + | + |
| Arthrolysis | + | + |
| Acromioplasty | + | + |
| Bankart’s repair | + | + |
| Latarjet | + | + |
| Proximal humerus osteosynthesis | + | ± |
| Acromioclavicular resection | + | – |
| Shoulder luxation | + | – |
| Clavicle osteosynthesis | + (± superficial cervical block) | – |
| Arthroscopic Surgery | ||
| Rotator cuff repair | + | + |
| Arthrolysis | + | + |
| Bankart’s repair | + | ± |
| Acromioplasty | + | ± |
NYSORA Tips
- Up to 70% of patients report severe pain on movement after open major shoulder surgery, which is more than after hysterectomy (60%), gastrectomy, or thoracotomy (60%).
- Major shoulder surgery entails massive nociceptive input from the richly innervated joint and periarticular tissues, which produce continuous deep somatic pain and bouts of reflex spasm of muscles.
- Periarticular structures exhibit not only C afferents, but also A alpha and A delta afferents, the latter being poorly blocked by opioids, which explains the relative inefficacy of opioids to control this type of postoperative pain.
Contraindications
Absolute contraindications include patient’s refusal, local infection, active bleeding in an anticoagulated patient, and proven allergy to local anesthetic. Relative contraindications include chronic obstructive airway disease, contralateral paresis of the phrenic or recurrent laryngeal nerves, and previous neurologic deficit of the involved arm. The risks and benefits of the chosen anesthetic technique should be discussed with the patient and the surgeon.
NYSORA Tips
- Skin infiltration of the posterior arthroscopic port site with local anesthetic is often necessary for arthroscopic shoulder surgery in addition to interscalene block.
Anatomy
The plexus is formed by the ventral rami of the fifth to eighth cervical nerves and the greater part of the ventral ramus of the first thoracic nerve (Figure 1). In addition, small contributions may be made by the fourth cervical and the second thoracic nerves. There are multiple complex interconnections between the neural elements of brachial plexus as they course from the interscalene groove to their endpoints in terminal nerves. However, most of what happens to these roots on their way to becoming peripheral nerves is not clinically essential information for the practitioner.
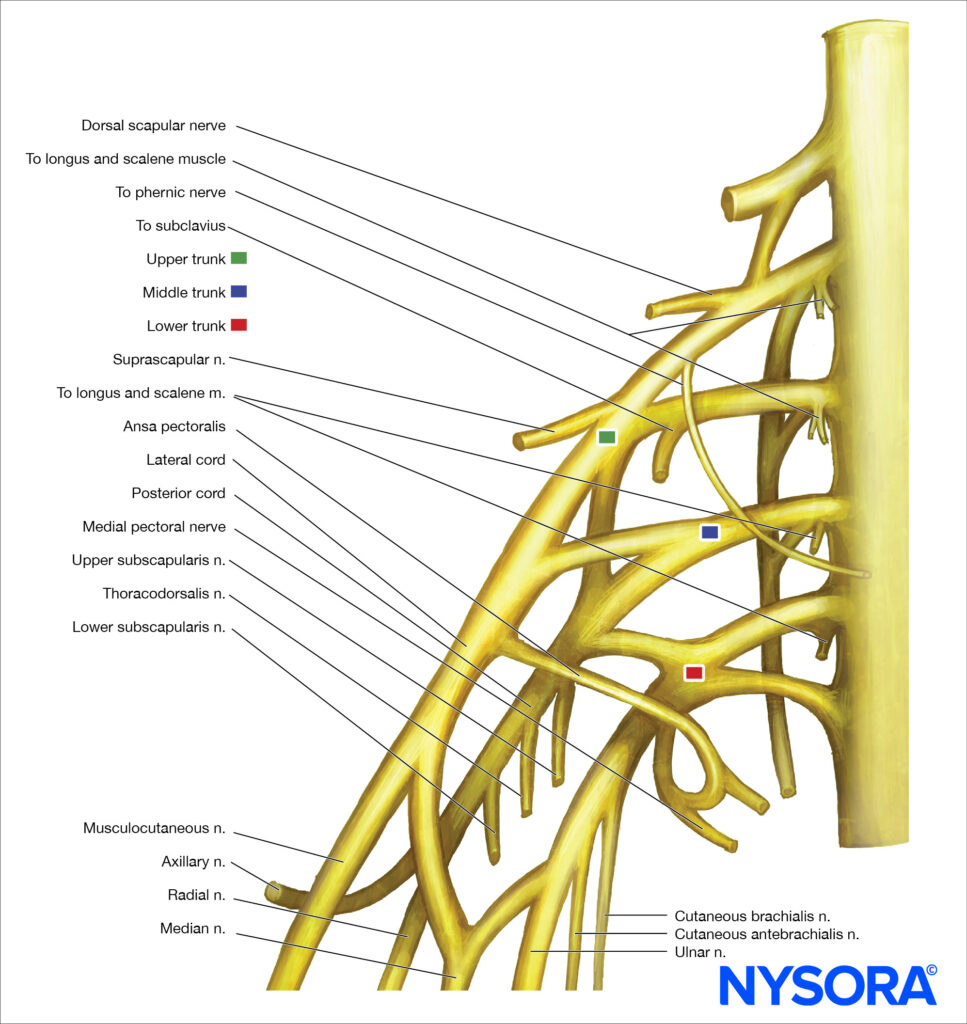
FIGURE 1. Organization of the brachial plexus. However, spatial arrangement of the trunks (superior, middle, and inferior) and interpretation of the motor response with nerve stimulation can be of importance. (Table 2).The brachial plexus supplies all the motor and most of the sensory functions of the shoulder except the cephalad cutaneous parts of the shoulder. These are innervated by the supraclavicular nerves originating from the lower part of the superficial cervical plexus (C3–4) (Figure 2) which supply sensation to the shoulder above the clavicle, the first two intercostal spaces anteriorly, the posterior cervical triangle and the upper thorax in this area as well as to the tip of the shoulder.
TABLE 2 Distribution of the brachial plexus.
| Nerve(s) | Spinal Segment(s) | Distribution |
|---|---|---|
| Subclavius nerve | C4 through C6 | Subclavius muscle |
| Dorsal scapular nerve | C4–C5 | Rhomboid muscles and levator scapulae muscle |
| Long thoracic nerve | C5 through C7 | Serratus anterior muscle |
| Suprascapular nerve | C4, C5, C6 | Supraspinatus and infraspinatus muscles |
| Pectoralis nerves (medial and lateral) | C5 through T1 | Pectoralis muscles |
| Subscapular nerves | C5, C6 | Subscapular and teres major muscles |
| Thoracodorsal nerve | C6 through C8 | Latissimus dorsi muscle |
| Axillary nerve | C5 and C6 | Deltoid and teres minor muscles; skin of shoulder |
| Radial nerve | C5 through T1 | Extensor muscles of the arm and forearm (triceps brachii, extensor carpi radialis, extensor carpi ulnaris) and brachioradialis muscle; digital extension and abductor pollicis muscle; skin over posterolateral surface of the arm |
| Musculocutaneous nerve | C5 through C7 | Flexor muscles of the arm (biceps brachii, brachialis, coracobrachialis); skin over lateral surface of the forearm |
| Median nerve | C6 through T1 | Flexor muscles of the forearm (flexor carpi radialis, palmaris longus); pronator quadratus, and pronator teres muscles; digital flexors (through the palmar interosseous nerve); skin over anterolateral surface of the hand |
| Ulnar nerve | C8, T1 | Flexor carpi ulnaris muscle, adductor pollicis muscle, and small digital muscles, skin over medial surface of the hand |
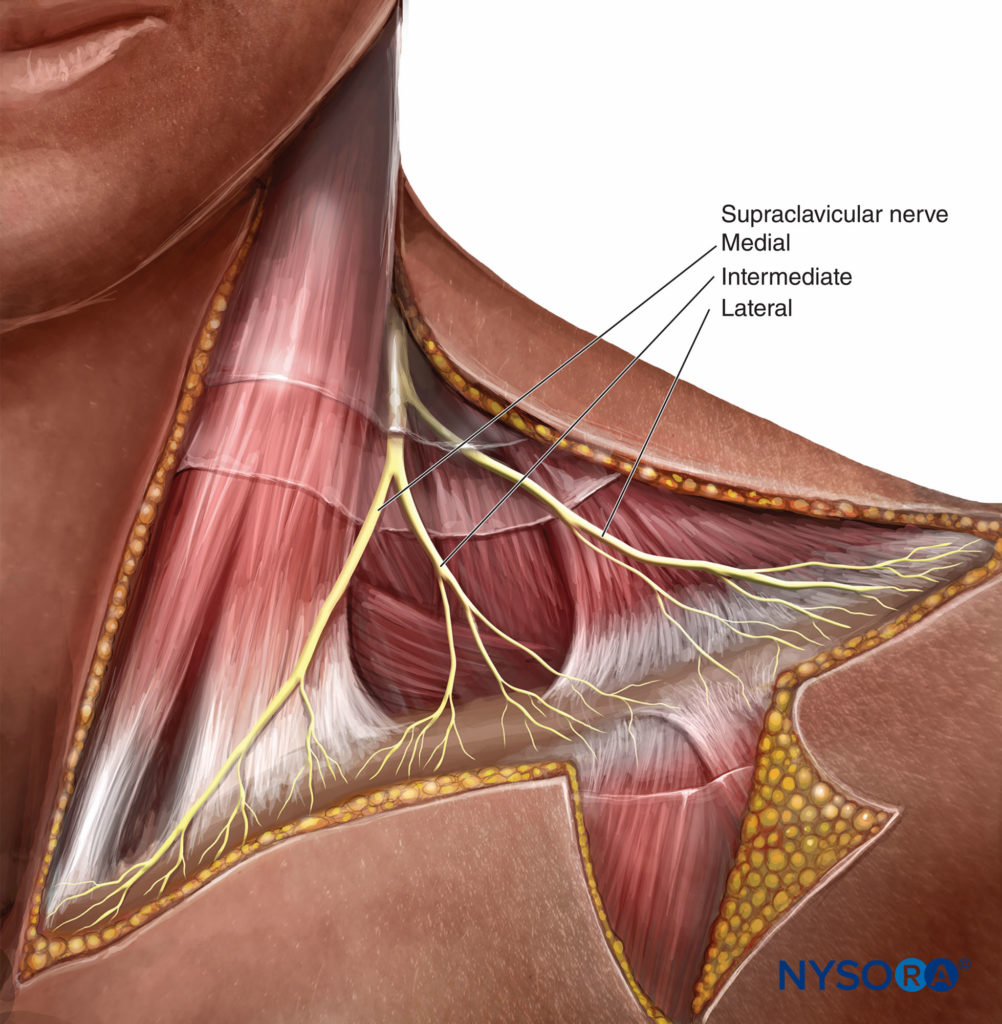
FIGURE 2. The innervation of the skin over the shoulder and clavicle.
Only three nerves of the brachial plexus innervate the shoulder. The most proximal of these is the upper lateral brachial cutaneous nerve, a branch of the axillary nerve that innervates the lateral side of the shoulder and the skin overlying the deltoid muscle. The upper medial side of the arm is innervated by both the medial brachial cutaneous and the intercostobrachial cutaneous nerves. In the anterior portion of the arm over the biceps muscle, the skin is innervated by the medial antebrachial cutaneous nerve.
Apart from the cutaneous nerve supply to the shoulder, the innervation of the joint deserves special consideration. In general, a nerve crossing a joint gives branches that innervate that joint. Therefore, the nerves supplying the ligaments, capsule, and synovial membrane of the shoulder derive from the axillary, suprascapular, subscapular, and musculocutaneous nerves.
The relative contributions of these nerves are not constant, and the supply from the musculocutaneus nerve may be very small or completely absent. Anteriorly, the axillary nerve and suprascapular nerve provide most of the nerve supply to the capsule and glenohumeral joint (Figure 3). In some instances, the musculocutaneous nerve may innervate the anterosuperior portion of the joint. In addition, the anterior capsule may be supplied by either the subscapular nerves or the posterior cord of the brachial plexus after piercing the subscapularis muscle.
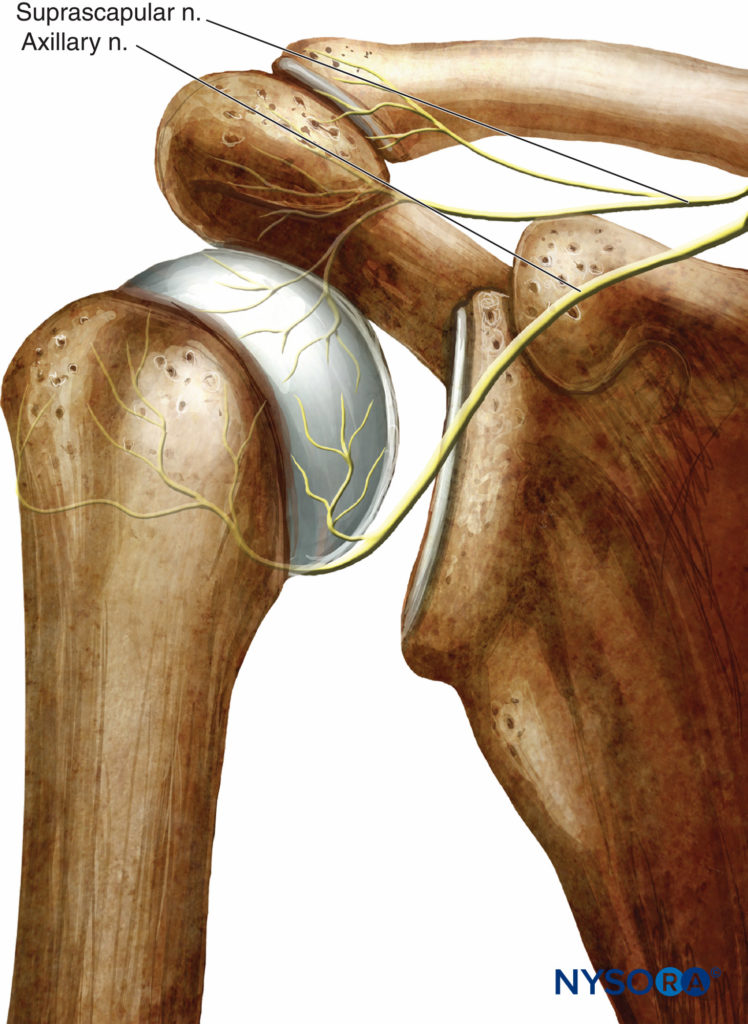
FIGURE 3. The innervation of the anterior portion of the shoulder. The axillary and suprascapular nerves form most of the nerve supply to the capsule and the glenohumeral joint.
Superiorly, the primary contribution is from two branches of the suprascapular nerve, one branch supplying the acromioclavicular joint and proceeding anteriorly as far as the coracoid process and coracoacromial ligament and the other branch reaching the posterior aspect of the joint. Other nerves contributing to this region of the joint are the axillary nerve and musculocutaneous nerve. Posteriorly, the main nerves are the suprascapular nerve in the upper region and the axillary nerve in the lower region (Figure 4). Inferiorly, the anterior portion is primarily supplied by the axillary nerve, and the posterior portion is supplied by a combination of the axillary nerve and lower ramifications of the suprascapular nerve.
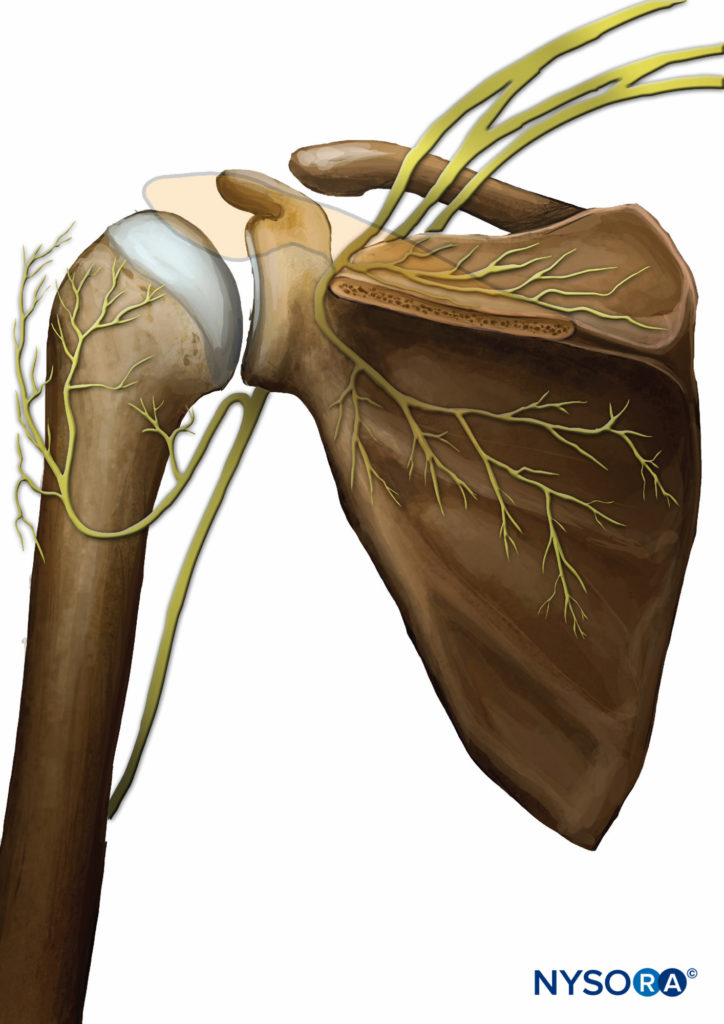
FIGURE 4. The posterior innervation of the shoulder joint. The primary nerves are the supra capsular and the axillary.
NYSORA Tips
- Arthroscopic shoulder surgery: Nerves of importance to anesthesia: supraclavicular, suprascapular, and axillary (radial) nerves.
- Open shoulder surgery: Knowledge of the surgical approach is important because surgery may also involve the territories of the median cutaneous, intercostobrachial, and the median antebrachial cutaneous nerves.
Landmarks
The following surface anatomy landmarks are important in identifying the interscalene space:
- Sternal head of the sternocleidomastoid muscle
- Clavicular head of the sternocleidomastoid muscle
- Upper border of the cricoid cartilage
- Clavicle (Figure 5)

FIGURE 5. Continuous interscalene brachial plexus block. The needle is inserted between anterior and middle scalene muscles in the pictured direction. The needle should not be placed deeper than 2-3 cm in most patients.
Equipment for Single-Injection Technique
Standard regional anesthesia equipment for a single-shot block consists of the following items (Figure 6):
- Marking pen, ruler
- Sterile gloves
- Peripheral nerve stimulator, surface electrode
- Disinfection solution and sterile gauze packs 2- to 5-cm, short-bevel, 22-gauge insulated stimulating needle
- Syringes with local anesthetic
- Injection pressure monitor
Learn more about Equipment for Peripheral Nerve Blocks.
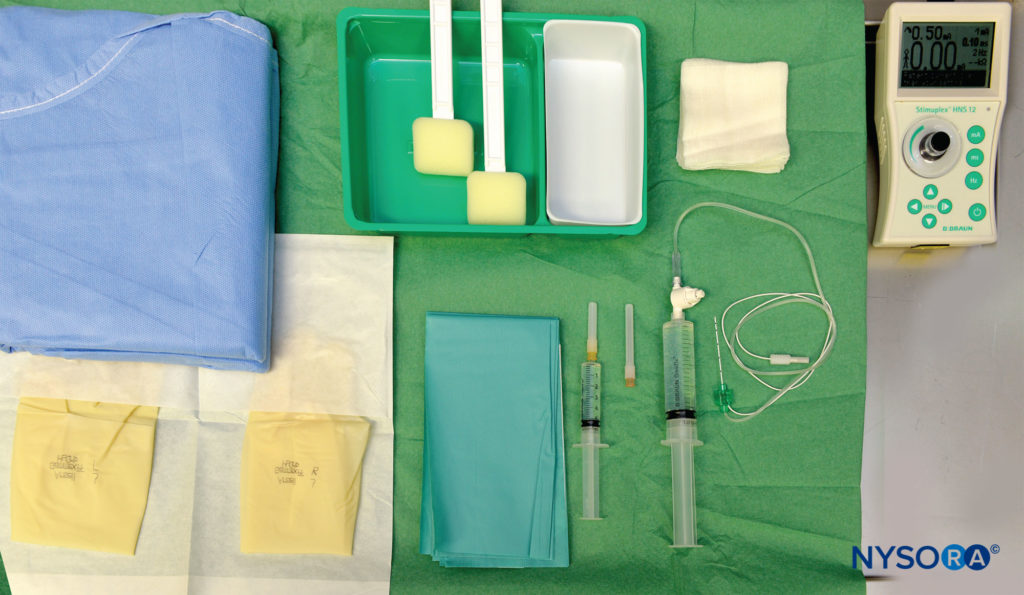
FIGURE 6. Equipment for single-injection interscalene block.
Equipment for Continuous Technique
Standard regional anesthesia equipment for a continuous nerve block consists of the following items (Figure 7).
- Marking pen, ruler
- Peripheral nerve stimulator, surface electrode
- Disinfection solution, sterile gauze packs
- Sterile transparent drapes
- Syringes with local anesthetic for skin infiltration and block injection
- 25-mm, 25-gauge needle for skin infiltration at puncture point and for tunneling
- A set with stimulating needle for continuous nerve block and catheter
- Adhesive material for securing the catheter
Learn more about Equipment for Continuous Peripheral Nerve Blocks.
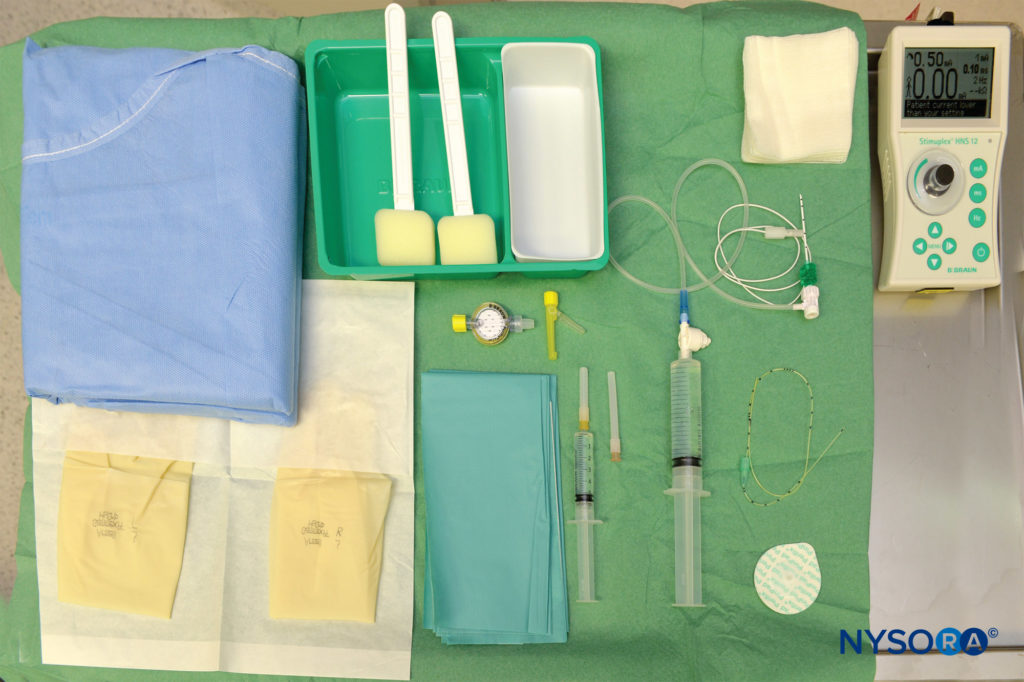
FIGURE 7. Equipment for continuous interscalene block.
APPROACHES TO AND TECHNIQUES FOR BRACHIAL PLEXUS BLOCK AT THE LEVEL OF THE NECK
Several approaches to the interscalene brachial plexus block have been described with the use of a nerve stimulator. In this chapter, we describe the classic (Winnie) technique and common modifications, including the low interscalene approach. The posterior (paravertebral) approach and its modifications have been largely abandoned for safety reasons and will be omitted from this volume.
Classic Technique (Winnie)
The classic approach of Winnie is performed at the level of the sixth cervical vertebra. Winnie originally used a paresthesia technique; however, most practitioners eventually adopted nerve stimulation.
- The patient is placed in a semisitting or supine position with the head turned away from the side to be blocked.
- The patient is asked to elevate the head slightly to bring the clavicular head of the sternocleidomastoid muscle into prominence.
- The index and middle fingers of the nondominant hand are placed immediately behind the lateral edge of the sternocleidomastoid muscle. The patient is instructed to relax so that the palpating fingers can be moved medially behind this muscle and finally lie on the belly of the anterior scalene muscle.
- The palpating fingers are then rolled laterally across the belly of the anterior scalene muscle until they fall into the interscalene groove (formed by scalene anterior and posterior muscles).
- With both fingers in the interscalene groove, a 1.5-in., 22- gauge, short-bevel needle is inserted between the fingers at the level of C6 in a direction that is perpendicular to the skin in every plane.
- After a motor response is obtained, aspiration is carried out to rule out intravascular or intrathecal placement. While the patient is monitored closely for signs of local anaesthetic toxicity or inadvertent subarachnoid injection, 15–20 mL of local anesthetic is slowly injected.
NYSORA Tips
- In Winnie’s original description, the needle is advanced slowly until a paresthesia is elicited or until the transverse process is encountered.
- Paresthesia below the level of the shoulder is sought because a paresthesia to the shoulder could result from stimulation of the suprascapular nerve inside or outside the interscalene space.
- If bone is contacted without producing a paresthesia, this is likely the transverse process and the needle should be gently “walked off “ anteriorly millimeter by millimeter until a paresthesia or motor response is evoked.
Reported complications with this technique are total spinal anesthesia, epidural anesthesia, cervical spinal cord injection with resultant paraplegia, as well as injections into the vertebral artery. These complications are more likely to occur with the classic technique than its modifications because the needle is directed perpendicularly towards the spinal cord. Although an infrequent complication, pneumothorax can also occur. This technique is not well suited for the placement of an interscalene catheter because of the perpendicular approach to the trunks.
Low Interscalene Brachial Plexus Block
The low interscalene technique of brachial plexus block differs in three important aspects from the classic approach and its modifications (Figure 5).
- Insertion of the needle is significantly lower than with the classic approach, which should reduce the risk of the needle entering the cervical cord or vertebral artery.
- The brachial plexus is very superficial at this location; the skin to brachial plexus block distance is often less than 1 cm and rarely deeper than 2 cm.
- The block can be considered a cross between a classic interscalene block (the plexus is approached in the distal interscalene groove) and a supraclavicular block (the needle insertion is slightly above the clavicle).
In contrast to the other approaches, the low interscalene approach provides reliable anesthesia for shoulder, elbow, and forearm surgeries alike.
Landmarks
The landmarks for the low interscalene approach are as follows (Figure 8):
- Clavicle
- Posterior border of the clavicular head of the sternocleidomastoid muscle
- External jugular vein
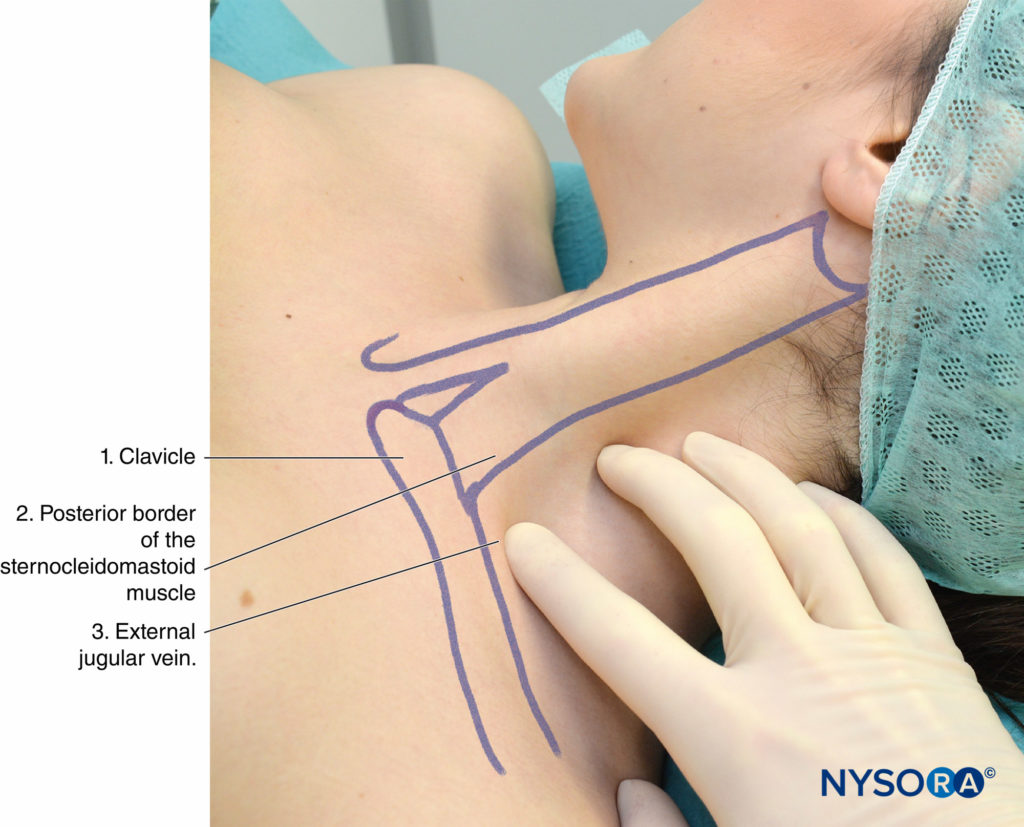
FIGURE 8. Landmarks for low interscalene approach to brachial plexus block: (1) Clavicle. (2) Posterior border of the sternocleidomastoid muscle. (3) External jugular vein. The palpating fingers are positioned in the scalene “groove” between anterior and middle scalene muscles.
The landmarks for the low interscalene approach are accentuated by the following maneuvers, which should be routinely performed:
- Ask the patient to face slightly away from the side to be blocked. This tenses the sternocleidomastoid muscle.
- Ask the patient to reach the ipsilateral knee on the side to be blocked or pull the patient’s wrist toward their knee. This flattens the skin of the neck and helps to identify both the scalene muscles and the external jugular vein.
- Ask the patient to lift the head off the table while facing away. This tenses the sternocleidomastoid muscle and helps to identify the posterior border of the clavicular head.
Technique
The fingers of the palpating hand should be gently pressed between the anterior and middle scalene muscles to reduce the distance between the skin and brachial plexus (Figure 9).

FIGURE 9. Fingers of the palpating hand are positioned in front of the external jugular vein and in the interscalene groove made up of anterior and middle scalene muscles. Interscalene groove is the widest and easiest to palpate in this position.
The palpating hand should not be moved during the entire procedure to allow for precise redirections of the needle. A needle connected to a nerve stimulator is inserted between the palpating fingers and advanced at an angle almost perpendicular to the skin and in a slight caudad direction (Figure 10). The nerve stimulator should be initially set to deliver 1 mA (2 Hz, 100 μsec). The needle is advanced slowly. Once any motor response of the brachial plexus is elicited, 15–20 mL of local anesthetic is injected slowly, with intermittent aspiration.

FIGURE 10. Low interscalene block. Proper angle of the needle direction is medial with a slight caudad angulation.
Some common responses to nerve stimulation and the course of action to obtain the proper response are shown in Table 3. The following motor responses can all be accepted as successful localization of the brachial plexus with a similar success rate:
- Pectoralis muscle
- Deltoid muscle
- Triceps muscles
- Any twitch of the hand or forearm
- Biceps muscle
3. Guide to troubleshooting interscalene block.
| Response Obtained | Interpretation | Problem | Action |
|---|---|---|---|
| Local twitch of the neck muscles | Direct stimulation of the anterior scalene or sternocleoidomastoid muscles | Needle pass is in the wrong plane; usually anterior and medial to the plexus | Withdraw the needle to the skin and reinsert 15 degrees posterior |
| Needle contacts bone at 1–2 cm depth; no twitches seen | The needle is stopped by the transverse process | The needle is inserted too posterior; the needle contacts anterior tubercles of the transverse process | Withdraw the needle to the skin and reinsert 15 degrees anterior |
| Twitches of the diaphragm | The result of stimulation of the phrenic nerve | The needle is inserted too anterior and medial | Withdraw the needle and reinsert 15 degrees posterior and lateral |
| Arterial blood noticed in the tubing | Puncture of the carotid artery (most likely) | The needle insertion and angulation are too anterior | Withdraw the needle and apply pressure for 5 min; reinsert 1–2 cm posterior |
| Pectoralis muscle twitch | Brachial plexus stimulation (C4–C5) | Accept and inject local anesthetic | |
| Twitch of the scapula | Twitch of the serratus anterior muscle; stimulation of the thoracodorsal nerve | Needle position is posterior/deep to the brachial plexus | Withdraw the needle to the skin, and reinsert the needle anterior |
| Trapezius muscle twitches | Accessory nerve stimulation | Needle posterior to the brachial plexus | Withdraw the needle and insert more anteriorly |
| Twitch of pectorals, deltoid, triceps, biceps, forearm, and hand muscles | Stimulation of the brachial plexus | None | Accept and inject local anesthetic |
Continuous Interscalene Brachial Plexus Block
The continuous interscalene brachial plexus block is an advanced technique. Paradoxically, although the single-shot interscalene block is one of the easiest intermediate techniques to perform and master, placement of the catheter in the interscalene groove is much more challenging. This is partially due to the shallow position of the brachial plexus and difficulties in stabilizing the needle during catheter advancement. This technique provides excellent analgesia in patients after shoulder, arm, and elbow surgery.
Technique
The patient is positioned in the same position as in the single- injection technique. After local anesthesia, a 5-cm long needle attached to a nerve stimulator (1.0 mA) is inserted at a slightly caudal angle and advanced until the brachial plexus twitch is elicited at 0.2–0.5 mA (Figure 11). While paying meticulous attention to the position of the needle, the catheter is inserted some 3 cm beyond the tip of the needle and secured to the skin.
The catheter must be carefully checked for intravascular placement before administering large volumes or an infusion of local anesthetics. Before initiating the infusion of local anesthetic, the catheter is first checked for patency, and intravascular placement is ruled out by administering a small volume (2–3 mL of 1% lidocaine with epinephrine 1:300,000). The management of the continuous infusion of local anesthetic is discussed in the section about intraoperative management below.

FIGURE 11. Continuous interscalene block. Note the low angle of needle insertion, which is necessary to facilitate insertion of the catheter.
Clinical Pearl
The following maneuvers help to localize the interscalene groove:
- Ask the patient to turn the head away from the side to be blocked and then to lift the head off the table. This maneuver tenses the sternocleidomastoid muscle and helps to identify the lateral border of the clavicular head of the sternocleidomastoid muscle.
- In some patients, the clavicular head of the sternocleidomastoid
and anterior scalene muscles are packed together. The practitioner can ask the to sniff as the practitioner places the fingers firmly on the muscles. The anterior and middle scalene muscles contract during this maneuver, making their palpation and recognition of the scalene space easier
INTRAOPERATIVE MANAGEMENT OF AN INTERSCALENE BLOCK DURING SHOULDER SURGERY
Sedation is almost always useful to improve patient comfort and satisfaction. This is in keeping with the preference of most surgeons for their patients to be ‘asleep’ during surgery, as is also the preference of most patients.
Drugs most commonly used to accomplish this are propofol, midazolam, and an intravenous opioid. A face mask with oxygen (4–6 L/min) should be routinely applied. Patients should be kept warm by using forced air or warm blankets.
The onset of shivering can turn a successful regional anesthetic into a significant intraoperative challenge. Intraoperative use of pneumatic equipment close to the patient’s ear can result in noise levels over 100 dB. A significant amount of sedation is needed to mask this noise. The use of earplugs, headphones with or without music, or blankets to protect the patient’s ears can make a substantial difference in their comfort, and reduce the amount of sedative drugs required. Hyperhydration should be avoided because the patients are typically not given a urinary catheter, and the sensation of a full bladder can cause considerable discomfort for the patient. It is a good idea to ask patients to empty their bladder before administering any drugs.
Choice of Local Anesthetic
For single-shot techniques, a variety of local anesthetics can be used (Table 4), depending on the desired duration and density of block. The typical volume of local anesthetic used for interscalene blocks is 15–20 mL of ropivacaine 0.5% or 0.75%. Clonidine, but not opioids, can prolong the duration of both anesthesia and analgesia with intermediateacting local anesthetics. The addition of epinephrine also prolongs the duration of action of most local anesthetics.
Continuous infusion of local anesthetics through an interscalene catheter compared with traditional patient-controlled analgesia (PCA) with opioids provides significantly better control of pain, with a lower incidence of side effects and greater patient satisfaction. Catheters are typically left in place for 2–3 days. A typical regimen for continuous infusion would be the use of ropivacaine 0.2% at a rate of 5 mL/h with a 5 mL q60min patient controlled bolus.
TABLE 4. Local anesthetic mixtures used for single-injection techniques.
| Onset (min) | Anesthesia (h) | Analgesia (h) | |
|---|---|---|---|
| 3% 2-Chloroprocaine (+ HCO3 + epinephine) | 5–10 | 1.5 | 2 |
| 1.5% Mepivacaine (+ HCO3) | 10–20 | 2–3 | 2–4 |
| 1.5% Mepivacaine (+ HCO3 + epinephrine) | 5–15 | 2.5–4 | 3–6 |
| 2% Lidocaine (+ HCO3) | 10–20 | 2.5–3 | 2–5 |
| 2% Lidocaine (+ HCO3 + epinephrine) | 5–15 | 3–6 | 5–8 |
| 0.5% Ropivacaine | 15–20 | 6–8 | 8–12 |
| 0.75% Ropivacaine | 5–15 | 8–10 | 12–18 |
| 0.5% Bupivacaine (+ epinephrine) | 20–30 | 8–10 | 16–18 |
SIDE EFFECTS AND COMPLICATIONS AND HOW TO AVOID THEM
Complications associated with the different techniques of interscalene block are summarized in (Table 5).
TABLE 5. Complications of interscalene block according to approach.
| Winnie | Posterior | Modified Lateral | |
|---|---|---|---|
| Spinal injection | ++ | ++ | – |
| Epidural injection | ++ | ++ | – |
| Vertebral artery injection | + | (+) | – |
| Intravenous injection | + | + | + |
| Pneumothorax | + | + | + |
| Discomfort | (+) | ++ | (+) |
| Conditions for catheter placement | – | + | ++ |
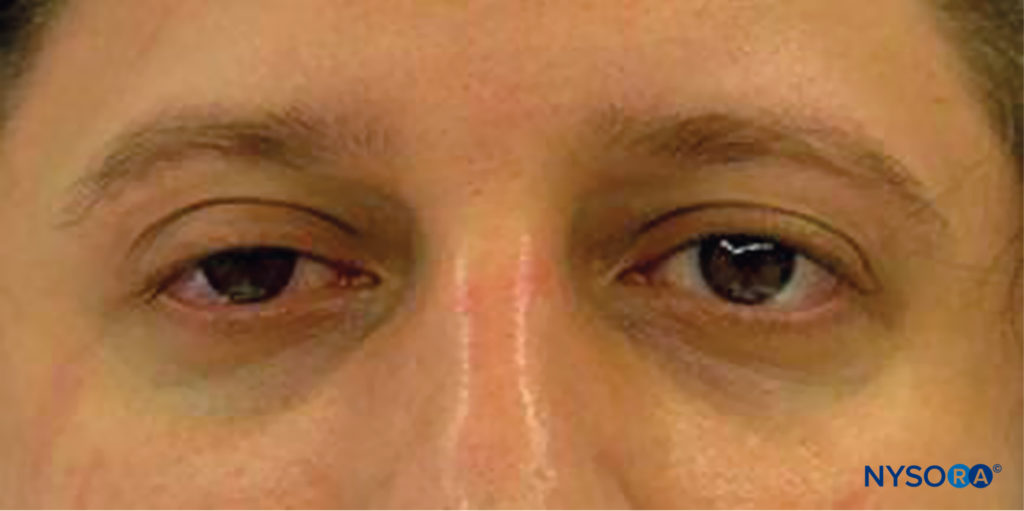
FIGURE 12. Horner syndrome is common after interscalene block and consists of ptosis, myosis, and enophthalmia.
The most common side effects encountered after interscalene block are hoarseness (10%–20%) due to the block of the recurrent laryngeal nerve, which occurs more frequently on the right side. Horner syndrome is characterized by ptosis, myosis, and enopthalmia due to the diffusion of the local anesthetic solution on the sympathetic cervical ganglion chain (including the stellatum ganglion) (Figure 12). The reason for this complication is the spread of the local anesthetic around the anterior scalene muscle behind the carotid artery and internal jugular vein toward the longus colli muscle (Figure 13). This results in block of the cervical ganglion (Horner syndrome) and phrenic nerve, which are located in this area.
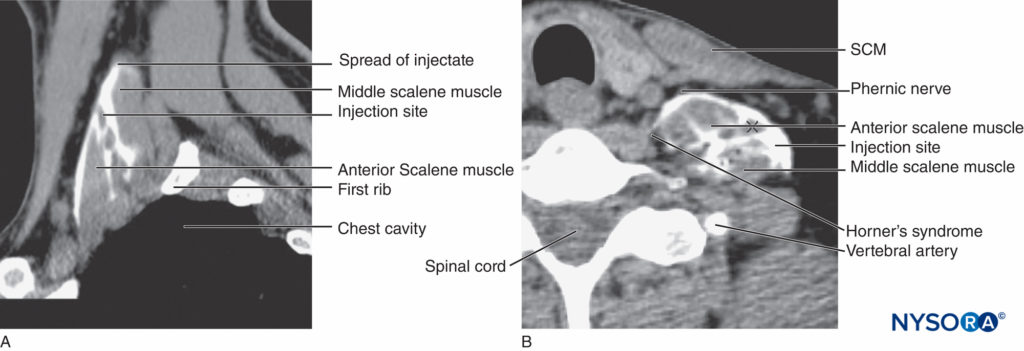
FIGURE 13. Spread of the solution after injection into interscalane space. The contrast is seen in the scalene space around brachial plexus as well as dispersing underneath cervical fascia over anterior and middle scalene muscles. This spread helps explain the common occurrence of phrenic block and Horner’s syndrome after ISBPB.
In addition, the superior laryngeal nerve (Figure 14) can be affected. It occurs in 40%–60% of patients and resolves with resolution of the block; patient reassurance is all that is needed for management. Ipsilateral hemidiaphragmatic paresis is a common finding and may be present in nearly 100% of patients (Figure 15). However, this rarely presents a problem clinically, and most patients are not aware of it. The paradoxical Bezold-Jarisch reflex (occurrence of bradycardia and hypotension; incidence 15%–30%), can occur when the patient is placed in the sitting position for shoulder surgery and can be prevented by avoiding hypovolemia. It is easily treated by atropine and ephedrine administration.
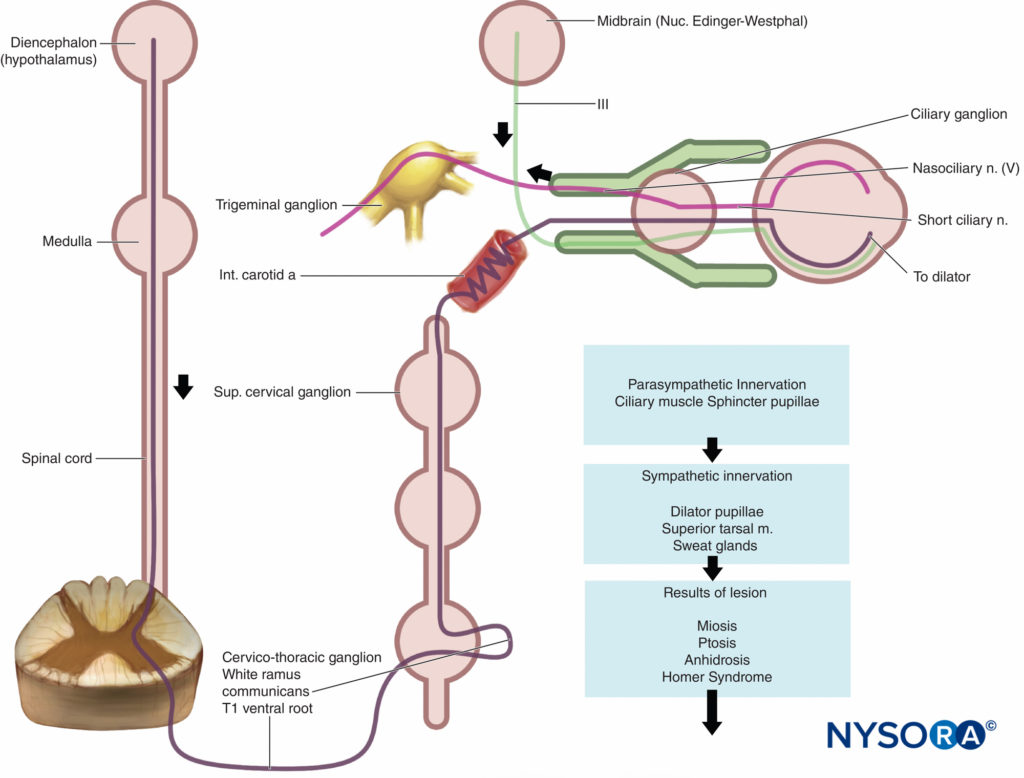
FIGURE 14. Horner syndrome results from interruption of the sympathetic pathway anywhere from the hypothalamus (diencephalon) to the eye.
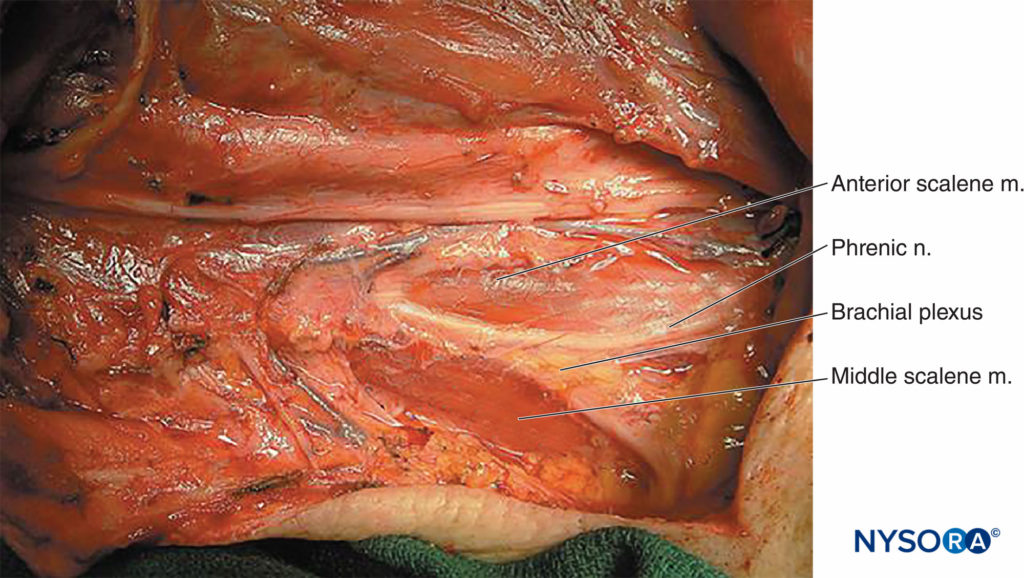
FIGURE 15. Neck dissection reveals the relationship of the phrenic nerve, which leaves the brachial plexus anteriorly, and the rest of the brachial plexus, which remains sandwiched between the anterior and middle scalene muscles.
Early complications (soon after block administration), such as epidural, spinal, or intravascular injection are primarily related to the approach chosen (see Table 5). Late complications include neuropathy, mechanical plexus injury, and infection.
Nerve injuries are a well-recognized complication of anesthesia, although nerve injury directly attributable to interscalene block is extremely rare.
Factors related to patient position, such as the use of shoulder braces and the head position, malposition of the arms, and sustained neck extension may increase the risk of injury. Little data are available on the rate of complications related to the use of the continuous interscalene catheters. Table 6 lists reported complications of interscalene blocks and suggestions on how to avoid them.
TABLE 6. Complications and how to avoid them.
| Infection | • A strict aseptic technique is used |
| Hematoma | • Avoid multiple needle insertions, particularly in anticoagulated patients • Apply steady pressure for 5 min when carotid artery is inadvertently punctured • Use a smaller gauge needle to localize the brachial plexus in patients with difficult anatomy • In the absence of spontaneous bleeding, the use of anticoagulant therapy should not be regarded as a contraindication for this block |
| Vascular puncture | • Vascular puncture is not common with this technique • Apply steady pressure for 5 min when the carotid artery is punctured |
| Local anesthetic toxicity | • Systemic toxicity due to absorption of local anesthetic after interscalene block is rare • Systemic toxicity most commonly occurs during or shortly after injection of local anesthetic; this is most commonly caused by an inadvertent intravascular injection or channeling of forcefully injected local anesthetic into small veins or lymphatic channels cut during needle manipulation • Large volumes of long-acting anesthetic should be reconsidered in older and frail patients. • Careful and frequent aspiration should be performed during the injection • Avoid forceful, fast injection of local anesthetic |
| Nerve injury | • Never inject local anesthetic when abnormal pressure on injection is encountered (opening pressure >15 psi) • Local anesthetic should never be injected when patient complains of severe pain or exhibits a withdrawal reaction on injection |
| Total spinal anesthesia | • When stimulation is obtained with current intensity of <0.2 mA, the needle should be pulled back to obtain the same response with current >0.2 mA before injecting local anesthetic to avoid injection into the dural sleeves and the consequent epidural or spinal spread • Never inject local anesthetic when abnormal pressure on injection is encountered |
| Horner syndrome | • Occurrence of ipsilateral ptosis, hyperemia of the conjunctiva, and nasal congestion is common, and it is dependent on the site of injection (less common with the low interscalene approach) and total volume of local anesthetic injected; patients should be instructed on the occurrence of this syndrome and reassured about its benign nature |
| Diaphragmatic paralysis | • Commonly present; avoid interscalene block or a large volume of local anesthetic in patients |
SUMMARY
Interscalene nerve block is one of the most clinically applicable nerve block techniques. With proper training, equipment, and monitoring precautions the technique results in a predictable success rate, excellent anesthesia, and superb postoperative analgesia.
This text is a sample of content from the Compendium of Regional Anesthesia on the NYSORA LMS.
NYSORA’s Compendium of Regional Anesthesia is simply the most comprehensive, and practical curriculum on Regional Anesthesia from A to Z, featuring NYSORA’s Premium content. As opposed to textbooks and e-books, the Compendium is continuously updated and features NYSORA’s newest videos, animations, and visual content.
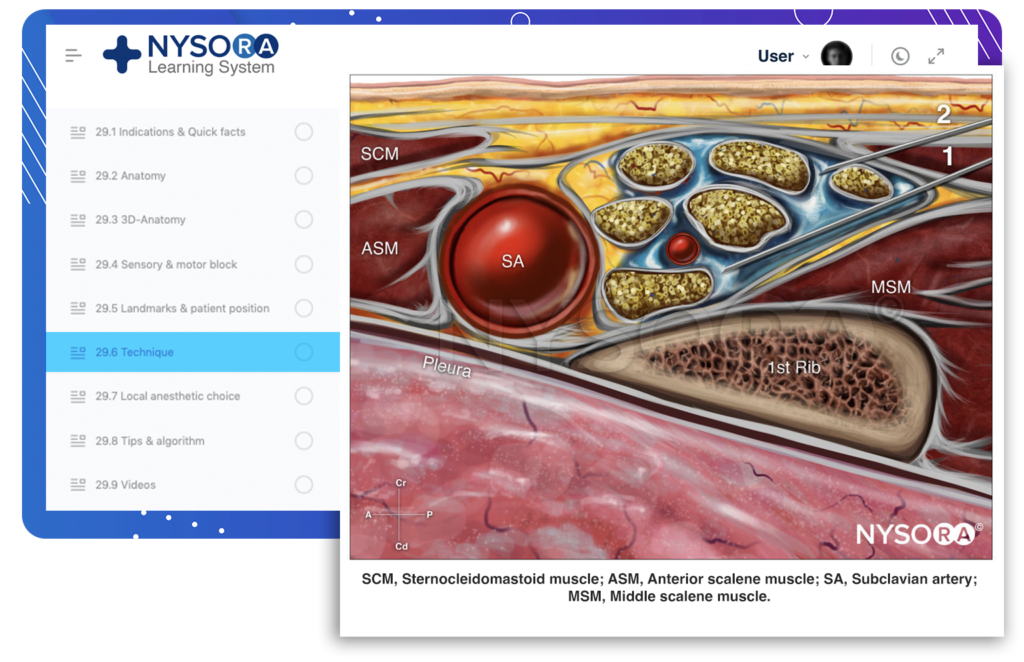
The Compendium is one of several gold-standard educational courses on NYSORA’s Learning System (the NYSORA LMS), and registration to NYSORALMS.com is free. The FULL access to the Compendium, however, is based on an annual subscription, as it requires an army of illustrators, video editors, and an educational team to continue making it the BEST tool for education on everything regional anesthesia. While you can think of the compendium as an ebook on steroids, a quick test drive will give you a real-time feel of how incredible the Compendium really is. Your subscription will transform the way you read about regional anesthesia:
- Learn visually: Everything regional, including spinal, epidural, and nerve block procedures and management protocols
- Review step-by-step techniques instructions for over 60 nerve blocks
- Access NYSORA’s fabled illustrations, animations, and videos (such as Reverse Ultrasound Anatomy)
- Access RA info on any device via the desktop platform and mobile app
- Get real-time updates
- Review infographics for exam preparation (e.g. EDRA)
- Use the Community feed with real case discussions, images and videos are posted and discussed by subscribers and world’s top experts alike.
Even if you do not wish to subscribe to the Compendium, do register to the NYSORA LMS, be the first to know what’s new in regional anesthesia, and get involved in case discussions.
Here’s what the activity feed on NYSORA LMS looks like:
We are convinced that once you experience the Compendium on the NYSORA LMS, and you’ll never go back to your old books, and your subscription will support keeping NYSORA.com free for the rest of the world.
Additional reading
- Etienne J: Regional anesthesia: Its application in the surgical treatment of cancer of the breast [French], Faculté de Médecin de Paris, 1925.
- Winnie AP: Interscalene brachial plexus block. Anesth Analg 1970;49:455–466.
- Borgeat A, Ekatodramis G: Anaesthesia for shoulder surgery. Best Pract Res Clin Anaesthesiol 2002;16:211–225.
- Kapral S, Greher M, Huber G, et al: Ultrasonographic guidance improves the success rate of interscalene brachial plexus block. Reg Anesth Pain Med 2008;33:253–258.
- McNaught A, Shastri U, Carmichael N, et al: Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth 2011;106: 124–130.
- Gautier P, Vandepitte C, Ramquet C, et al: The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg 2011;113:951–955.
- Bonica JJ: Anatomic and physiologic basis of nociception and pain. In Bonica JJ (ed). The Management of Pain, 2nd ed. Philadelphia, PA: Lea & Febiger, 1990, pp 28–94.
- Bonica JJ (ed): Postoperative pain. In The Management of Pain, 2nd ed. Philadephia, PA: Lea & Febiger, 1990, pp 461–480
- Hollinshead WH: Anatomy for Surgeons, 3rd ed. Philadelphia, PA: Harper & Row, 198
- DePalma AF: Surgery of the Shoulder, 3rd ed. Philadelphia, PA: Lippincott, 1983
- Gardner E: The innervation of the shoulder joint. Anat Rec 1948; 102:1–18
- Dutton RP, Eckhardt WF 3rd, Sunder N: Total spinal anesthesia after interscalene block of the brachial plexus. Anesthesiology 1994;80: 939–941
- Ross S, Scarborough CD: Total spinal anesthesia following brachialplexus block. Anesthesiology 1973;39:458.
- Scammell SJ: Case report: Inadvertent epidural anaesthesia as a complication of interscalene brachial plexus block. Anaesth Intensive Care 1979;7:56–57.
- Benumof JL: Permanent loss of cervical cord function associated with interscalene block performed under general anesthesia. Anesthesiology 2000;93:151–154.
- Pippa P, Cominelli E, Marinelli C, Aito S: Brachial plexus block using the posterior approach. Eur J Anaesthesiol 1990;7:411–420.
- Dagli G, Guzeldemir ME, Volkan Acar H: The effects and side effects of interscalene brachial plexus block by posterior approach. Reg Anesth Pain Med 1998;23:87–91.
- Rucci FS, Pippa P, Barbagli R, Doni L: How many interscalenic blocks are there? A comparison between the lateral and posterior approach. Eur J Anaesthesiol 1993;10:303–307.
- Boezaart AP, De Beer JF, Nell ML: Early experience with continuous cervical paravertebral block using a stimulating catheter. Reg Anesth Pain Med 2003;28:406–413.
- Meier G, Bauereis C, Heinrich C: [Interscalene brachial plexus catheter for anesthesia and postoperative pain therapy. Experience with a modified technique]. Anaesthesist 1997;46:715–719.
- Hadzic A, Vloka JD (eds): Interscalene brachial plexus block. In Peripheral Nerve Blocks: Principles and Practice. New York, NY: McGraw-Hill, 2003, pp 1009–1029.
- Low interscalene abstract from ASRA 2005 presentation.
- Dickerman D, Vloka JD, Koorn R, Hadzic A: Excessive noise levels during orthopedic surgery. Reg Anesth 1997;22:97.
- Brown AR, Weiss R, Greenberg C, et al: Interscalene block for shoulder arthroscopy: Comparison with general anesthesia. Arthroscopy 1993;9:295–300.
- Tetzlaff JE, Yoon HJ, O’Hara J, et al: Alkalinization of mepivacaine accelerates onset of interscalene block for shoulder surgery. Reg Anesth Pain Med 1990;15:242–244.
- Klein SM, Greengrass RA, Steele SM, et al: A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg 1998;87:1316–1319.
- Casati A, Borghi B, Fanelli G, et al: Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: A randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg 2003;96:253–259.
- Singelyn FJ, Gouverneur JM, Robert A: A minimum dose of clonidine added to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg 1996;83:1046–1050.
- Picard PR, Tramer MR, McQuay HJ, Moore RA: Analgesic efficacy of peripheral opioids (all except intra-articular): A qualitative systematic review of randomised controlled trials. Pain 1997;72:309–318.
- Bouaziz H, Kinirons BP, Macalou D, et al: Sufentanil does not prolong the duration of analgesia in a mepivacaine brachial plexus block: a dose response study. Anesth Analg 2000;90:383–387.
- Tetzlaff JE, Yoon HJ, Brems J, Javorsky T: Alkalinization of mepivacaine improves the quality of motor block associated with interscalene brachial plexus anesthesia for shoulder surgery. Reg Anesth Pain Med 1995;20:128–132.
- Hadzic A, Williams BA, Kraca PE, et al: For outpatient rotator cuff surgery, nerve block anesthesia provides superior same-day recovery over general anesthesia. Anesthesiology 2005;102:1001–1007.Klein SM, Grant SA, Greengrass RA, et al: Interscalene brachial plexus block with a continuous catheter insertion system and a disposable infusion pump. Anesth Analg 2000;91:1473–1478.
- Borgeat A, Schappi B, Biasca N, Gerber C: Patient-controlled analgesia after major shoulder surgery: patient-controlled interscalene analgesia versus patient-controlled analgesia. Anesthesiology 1997;87:1343–1347
- Singelyn FJ, Seguy S, Gouverneur JM: Interscalene brachial plexus analgesia after open shoulder surgery: Continuous versus patientcontrolled infusion. Anesth Analg 1999;89:1216–1220.
- Borgeat A, Tewes E, Biasca N, Gerber C: Patient-controlled interscalene analgesia with ropivacaine after major shoulder surgery: PCIA vs PCA. Br J Anaesth 1998;81:603–605.
- Borgeat A, Kalberer F, Jacob H, et al: Patient-controlled interscalene analgesia with ropivacaine 0.2% versus bupivacaine 0.15% after major open shoulder surgery: The effects on hand motor function. Anesth Analg 2001;92:218–223.
- Rosenberg PH, Heinonen E: Differential sensitivity of A and C nerve fibres to long-acting amide local anaesthetics. Br J Anaesth 1983;55:163–167.
- Wildsmith JA, Brown DT, Paul D, Johnson S: Structure-activity relationships in differential nerve block at high and low frequency
- Urmey WF, Talts KH, Shrarock NE: One hundred percent incidence of hemi-diaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991;72:498–503
- Todd MM, Brown DL: Regional anesthesia and postoperative pain management: long-term benefits from a short-term intervention. Anesthesiology 1999;91:1–2.
- Kroll DA, Caplan RA, Posner K, et al: Nerve injury associated with anesthesia. Anesthesiology 1990;73:202–207.
- Borgeat A, Ekatodramis G, Kalberer F, Benz C: Acute and nonacute complications associated with interscalene block and shoulder surgery: A prospective study. Anesthesiology 2001;95:875–880.
- Borgeat A, Dullenkopf A, Ekatodramis G, Nagy L: Evaluation of the lateral modified approach for continuous interscalene block after shoulder surgery. Anesthesiology 2003;99:436–442.






