Clavicle fractures—particularly midshaft fractures—are among the most frequently encountered injuries in emergency and orthopedic care. They are typically associated with significant pain, prompting the need for effective and localized regional anesthesia. While techniques such as the supraclavicular brachial plexus block are widely used, they carry inherent risks, including phrenic nerve palsy, hemidiaphragmatic paresis, and potential motor block of the upper limb.
The recently developed midclavicle block (MCB) aims to address these limitations by providing a more anatomically targeted approach. By focusing specifically on the anterosuperior and posteroinferior surfaces of the clavicle—particularly at the fracture site—this block avoids involvement of deeper neurovascular structures, offering both efficacy and safety.
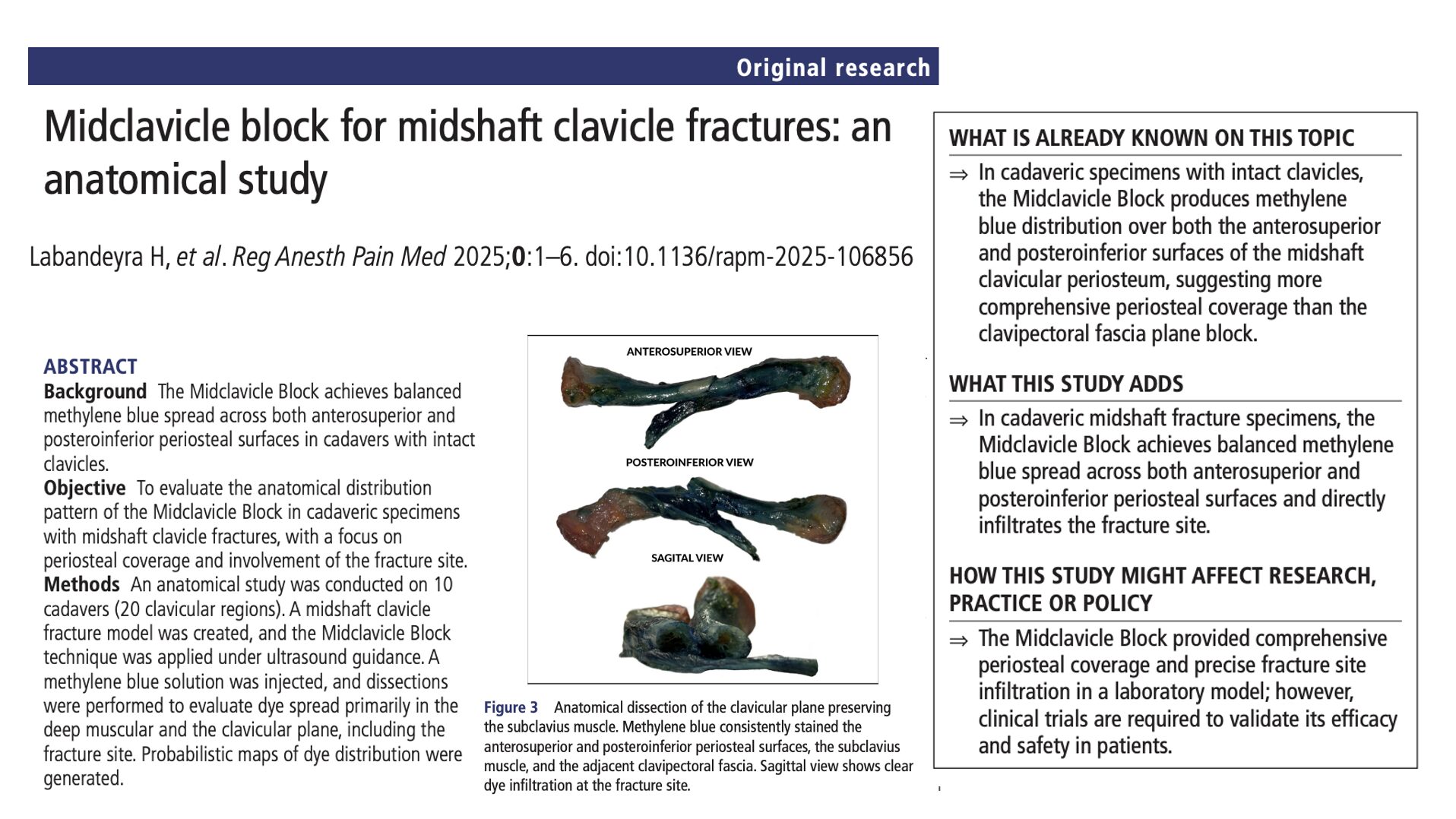
A new anatomical study published in Regional Anesthesia & Pain Medicine evaluated the distribution pattern of this innovative block in a cadaveric model designed to simulate midshaft clavicle fractures. The findings highlight the MCB’s potential to revolutionize pain management strategies for clavicular trauma.
Study objective and methods
The primary goal of this study was to assess whether the MCB provides consistent and balanced coverage of the clavicular periosteum—including the fracture site—without involving surrounding vital structures. Specifically, the researchers aimed to map dye distribution on the anterosuperior and posteroinferior surfaces of the clavicle to validate the block’s anatomical precision.
- Design: Anatomical cadaveric study.
- Sample: 10 cryopreserved cadavers (20 clavicular regions).
- Fracture model: A controlled midshaft clavicle fracture was created under ultrasound guidance to replicate the clinical setting.
- Injection technique: The MCB consisted of three ultrasound-guided injections:
- 15 mL of methylene blue dye injected anterosuperiorly medial to the fracture.
- 15 mL injected anterosuperiorly lateral to the fracture.
- 10 mL injected posteroinferiorly through the subclavius muscle.
- Dissection protocol: Specimens were carefully dissected in layers, allowing investigators to assess dye spread in the deep muscular and periosteal planes.
- Analysis tools: Researchers used photographic documentation and probabilistic mapping software to quantify dye coverage and assess anatomical boundaries.
Key findings
-
Consistent coverage at the fracture site
In all 20 specimens, methylene blue successfully reached the simulated fracture zone. This consistency supports the block’s ability to provide direct periosteal analgesia exactly where nociceptive input is greatest—at the fracture site itself.
-
Balanced anterosuperior and posteroinferior distribution
Quantitative analysis of periosteal staining revealed:
- Anterosuperior surface coverage: Mean 55.5% (95% CI: 50.6–60.4%).
- Posteroinferior surface coverage: Mean 53.8% (95% CI: 49.5–58.1%).
This dual-surface staining is clinically significant, as it reflects effective circumferential analgesic coverage of the bone, addressing both somatic and periosteal pain pathways.
-
Selective tissue infiltration without neural involvement
- The dye was consistently found in the subclavius muscle and clavipectoral fascia.
- No dye was observed in the pectoralis minor or in proximity to the infraclavicular brachial plexus.
- This pattern confirms the MCB’s safety, avoiding unintended spread to critical motor or sensory nerves.
Importantly, the block’s selective infiltration means a reduced risk of motor block—making it suitable for ambulatory care or trauma settings where preservation of limb function is essential.
-
High dye concentration localized to the midshaft
Probabilistic heat maps created from dissections indicated maximal staining intensity in the middle third of the clavicle, precisely correlating with the typical location of midshaft fractures. Lesser concentrations were observed in the medial and lateral thirds, aligning with the targeted nature of the MCB.
-
Comparison with clavipectoral fascia plane block (CPB)
The MCB demonstrated superior coverage of both anterior and posterior surfaces of the clavicle compared to previous anatomical studies of CPB. The CPB tends to result in anterior-only staining with poor diffusion to the posteroinferior periosteum and fracture site. These findings highlight the MCB’s anatomical advantage for periosteal and nociceptor targeting.
Limitations
While the anatomical insights provided are valuable, several limitations should be acknowledged:
- Cadaveric models lack the vascular dynamics, tissue compliance, and inflammatory responses present in living patients.
- Spread of injectate may differ in vivo due to factors such as bleeding, edema, or patient movement.
- Clinical effectiveness—including pain scores, duration of analgesia, and functional outcomes—remains untested.
These limitations underscore the need for clinical trials to validate the anatomical findings in a real-world patient population.
Conclusion
This anatomical study provides compelling evidence that the MCB offers precise and reliable periosteal coverage for midshaft clavicle fractures. Its three-point injection approach consistently delivers dye to both anterosuperior and posteroinferior surfaces of the clavicle, with direct involvement at the fracture site. Importantly, the MCB avoids critical structures such as the brachial plexus and phrenic nerve, reducing the risk of motor block and respiratory compromise.
By combining targeted analgesia with an improved safety profile, the MCB represents a promising advancement in regional anesthesia. Its anatomical precision, technical simplicity, and focused spread support its potential use in settings where traditional blocks may be contraindicated or pose unnecessary risk. Clinical validation through prospective trials will be essential to establish its role in standard pain management protocols for clavicle injuries.
Future research
This foundational anatomical work opens the door for several lines of clinical inquiry:
- In vivo trials: Prospective randomized studies are needed to evaluate MCB’s analgesic efficacy, onset time, duration, and opioid-sparing potential.
- Functional preservation studies: Assess whether the MCB indeed preserves upper limb motor function and diaphragmatic activity in patients compared to brachial plexus blocks.
- Expanded indications: Explore use of MCB in other clavicle-related procedures (e.g., surgery, post-dislocation pain).
- Comparison trials: Directly compare MCB with CPB, interscalene, and supraclavicular blocks in terms of efficacy, safety, and patient satisfaction.
- Prehospital feasibility: Investigate whether MCB can be safely and effectively performed in emergency department or ambulance settings for early pain control.
For more detailed information, refer to the full article in RAPM.
Labandeyra H. et al. Midclavicle block for midshaft clavicle fractures: an anatomical study. Reg Anesth Pain Med. Published online June 24, 2025.
Download the Nerve Blocks App HERE for in-depth insights on 60+ nerve block techniques from head to toe. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!