Explore NYSORA knowledge base for free:
This manual is the most up-to-date resource on best clinical practices and practical case management in anesthesiology. It is an essential guide for students, residents, and experienced practitioners to confidently manage complex clinical scenarios.
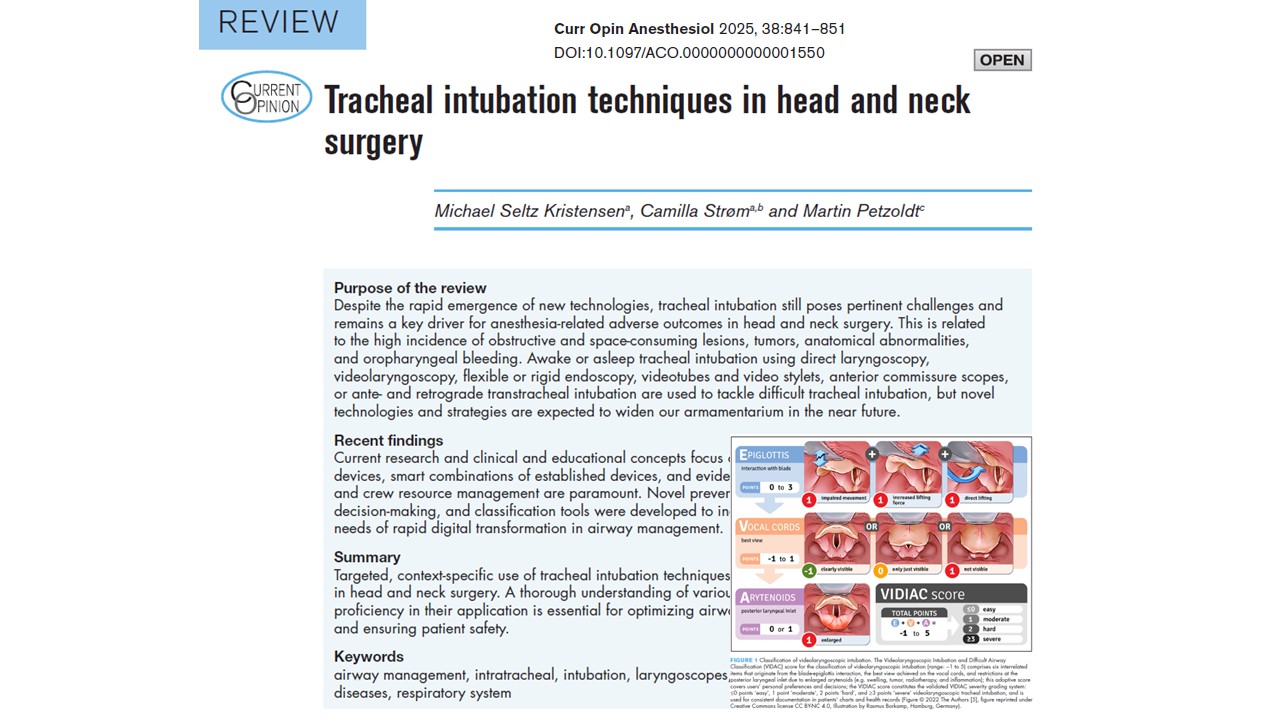
Head and neck surgeries pose significant airway management challenges due to anatomical distortions, tumor masses, prior radiation, and surgical scarring. The anesthesiologist’s role in these procedures extends far beyond induction—requiring vigilance, expertise in advanced airway techniques, and close collaboration with surgical teams. Given the complexity and frequency of difficult airways in this surgical subset, tracheal intubation must be approached with a thorough understanding of patient-specific risks, procedural implications, and available airway management strategies. This comprehensive article, based on the review by Kristensen et al. (2025), explores current best practices in tracheal intubation for head and neck surgery, detailing preoperative evaluation, intubation techniques, rescue strategies, and perioperative planning. It empowers anesthesiologists to navigate these high-stakes cases with confidence and precision. Understanding the unique challenges in head and neck airway management Head and neck pathology is often associated with: Obstructive tumors involving the oral cavity, pharynx, or larynx. Edema, fibrosis, or scarring from prior surgery or radiation therapy. Trismus, reduced neck mobility, or limited mouth opening. Airway deviation or distortion from masses, trauma, or congenital anomalies. These factors increase the likelihood of difficult mask ventilation, difficult laryngoscopy, and failed intubation, and may contraindicate conventional induction approaches. Key risks in this population: Complete airway obstruction on induction Limited options for rescue ventilation Higher rates of emergency tracheostomy Need for a shared airway between an anesthesiologist and the surgeon These realities demand meticulous preoperative airway assessment, anticipation of failure, and preparation for alternative plans, including awake techniques and front-of-neck access. Preoperative evaluation and planning Comprehensive airway assessment A thorough evaluation should include: Mallampati score Mouth opening (interincisor gap) Neck mobility and jaw protrusion Thyromental and sternomental distance Presence of tumors, prior surgery, or radiation Symptoms of airway compromise (dyspnea, stridor, positional breathing difficulty) When feasible, nasendoscopy offers invaluable information on vocal cord mobility, tumor […]
Pain remains one of the most common reasons patients seek medical care globally. As the complexity and diversity of pain presentations evolve—from acute musculoskeletal injuries to chronic inflammatory and neuropathic disorders—the need for targeted and well-tolerated pain management strategies has never been greater. While systemic analgesics, particularly oral medications, are widely used, their adverse effects and systemic absorption challenges limit their utility in certain patient populations. Topical analgesics represent a promising therapeutic alternative, as shown by Sisignano et al. 2025 in Anesthesiology. These agents deliver localized pain relief with minimal systemic involvement, offering significant benefits in conditions like osteoarthritis, diabetic peripheral neuropathy, and postherpetic neuralgia. Their ability to bypass gastrointestinal absorption and reduce systemic toxicity enhances their appeal, particularly in multimodal analgesia regimens. In this article, we examine the pharmacological basis, clinical efficacy, delivery challenges, and future directions of topical analgesics, offering anesthesiologists and pain management specialists a comprehensive overview of this crucial domain in contemporary pain care. Challenges of drug transport across the skin The skin, the body’s largest organ, poses significant barriers to drug delivery, particularly through its outermost layer, the stratum corneum. Comprising multiple layers of cornified keratinocytes (corneocytes), this structure is both lipophilic and dense, restricting drug penetration. Key absorption pathways: Intercellular route: Passage through the lipid–protein matrix. Intracellular route: Movement through corneocytes, hindered by the differing lipophilic and hydrophilic properties. Transappendageal route: Via sweat glands, sebaceous glands, and hair follicles. To overcome these barriers, modern topical formulations often incorporate chemical permeation enhancers (e.g., ethanol, dimethyl sulfoxide), colloidal carriers (e.g., liposomes, nanoemulsions), and polymeric gels that increase solubility, optimize release kinetics, and minimize skin irritation. Topical NSAIDs: mechanism and efficacy Mechanism of action Topical nonsteroidal anti-inflammatory drugs (NSAIDs) work by inhibiting cyclooxygenase-2 (COX-2) enzymes, thereby reducing local prostaglandin production and peripheral sensitization. Common agents include: Diclofenac […]