Arthur Atchabahian, Ine Leunen, Catherine Vandepitte, and Ana M. Lopez
FACTS
- Indications: Anterior thigh and knee surgery, analgesia following hip and knee procedures
- Transducer position: Transverse, close to the femoral crease and lateral to the femoral artery (Figure 1)
- Goal: A medial-lateral spread of local anesthetic underneath the fascia iliaca
- Local anesthetic: 20–40 mL of dilute local anesthetic (eg, 0.2% ropivacaine)

FIGURE 1. Needle insertion for the fascia iliaca nerve block. The blue dot indicates the position of the femoral artery. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
GENERAL CONSIDERATIONS
The fascia iliaca nerve block (also called the fascia iliaca compartment nerve block) is considered an alternative to a femoral nerve or a lumbar plexus nerve block. Since the femoral nerve and lateral femoral cutaneous nerve (LFCN) lie under the fascia of the iliacus muscle, a sufficient volume of local anesthetic deposited deep to the fascia iliaca may spread underneath the fascia in a medial and lateral direction to reach the femoral nerve and sometimes the LFCN. Although some authors suggest that the local anesthetic may also spread underneath fascia iliaca proximally toward the lumbosacral plexus, this has not been demonstrated consistently.
Before ultrasound (US), the technique involved needle placement at the lateral third of the distance from the anterior superior iliac spine to the pubic tubercle, using a “double-pop” technique as the needle passes through the fascia lata and fascia iliaca. However, nerve block success with this “feel” technique is sporadic because false “pops” can occur. In contrast, the US-guided technique allows monitoring of the needle placement and local anesthetic delivery and ensures delivery of the local anesthetic into the correct plane.
ULTRASOUND ANATOMY
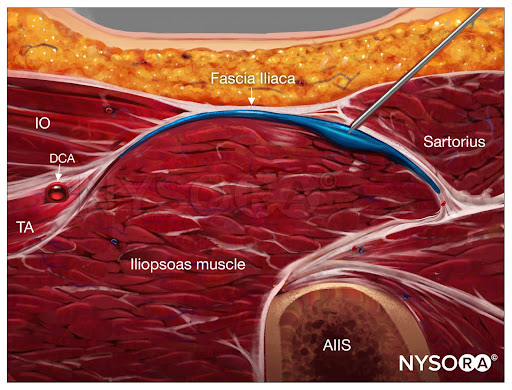
The fascia iliaca is located anterior to the iliacus muscle (on its surface) within the pelvis. It is bound superolaterally by the iliac crest and merges medially with the fascia overlying the psoas muscle. Both the femoral and lateral cutaneous nerves of the thigh lie under the fascia iliaca in their intrapelvic course. Anatomical orientation begins in the same manner as the femoral nerve block: identifying the femoral artery at the level of the inguinal crease. If it is not immediately visible, sliding the transducer medially and laterally will eventually bring the vessel into view. Immediately lateral and deep to the femoral artery and vein is a large hypoechoic structure, the iliopsoas muscle (Figure 2). It is covered by a hyperechoic fascia, which can be seen separating the muscle from the subcutaneous tissue superficial to it.
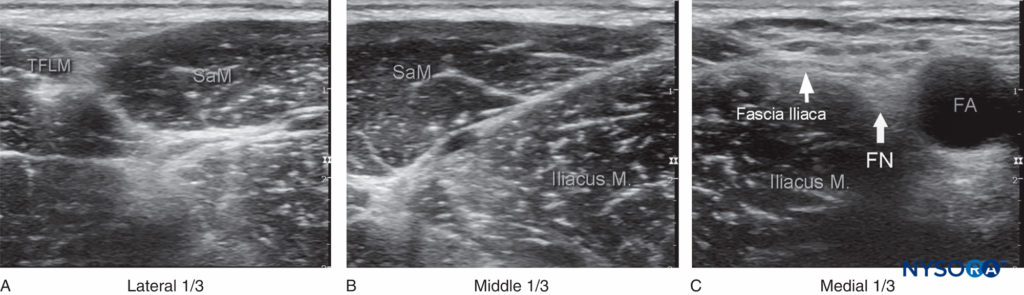
FIGURE 2. A panoramic view of the US anatomy of the femoral (inguinal) crease area. From lateral to medial, shown are the tensor fasciae latae muscle (TFLM), sartorius muscle (SaM), iliac muscle, fascia iliaca, femoral nerve (FN), and femoral artery (FA). The (A) lateral, (B) middle, and (C) medial thirds are derived by dividing the line between the FA and the anterior superior iliac spine in three equal sections. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
The hyperechoic femoral nerve should be seen wedged between the iliopsoas muscle and the fascia iliaca, lateral to the femoral artery. The fascia lata (superficial in the subcutaneous layer) is more superficial and may have more than one layer.
Moving the transducer laterally several centimeters brings into view the sartorius muscle covered by its own fascia as well as the fascia iliaca. Further lateral movement of the transducer reveals the anterior superior iliac spine (see Figure 2). Additional anatomical detail can be seen in the cross-sectional anatomy. Since the anatomy is essentially identical to that described for the femoral nerve block, it is not repeated here.
From the Compendium of Regional Anesthesia: Cognitive priming for an infrainguinal fascia iliaca block.
NYSORA Tips
The transducer can be placed anywhere between the level of the femoral crease and inguinal ligament.
DISTRIBUTION OF ANESTHESIA
The distribution of anesthesia and analgesia depends on the extent of local anesthetic spread and the nerves blocked. block of the femoral nerve results in anesthesia of the anterior and medial thigh (down to and including the knee) and anesthesia of the variable strip of skin on the medial leg and foot (saphenous nerve). The femoral nerve also contributes to articular fibers to both the hip and knee. The lateral femoral cutaneous nerve confers cutaneous innervation to the anterolateral thigh (Figure 3).
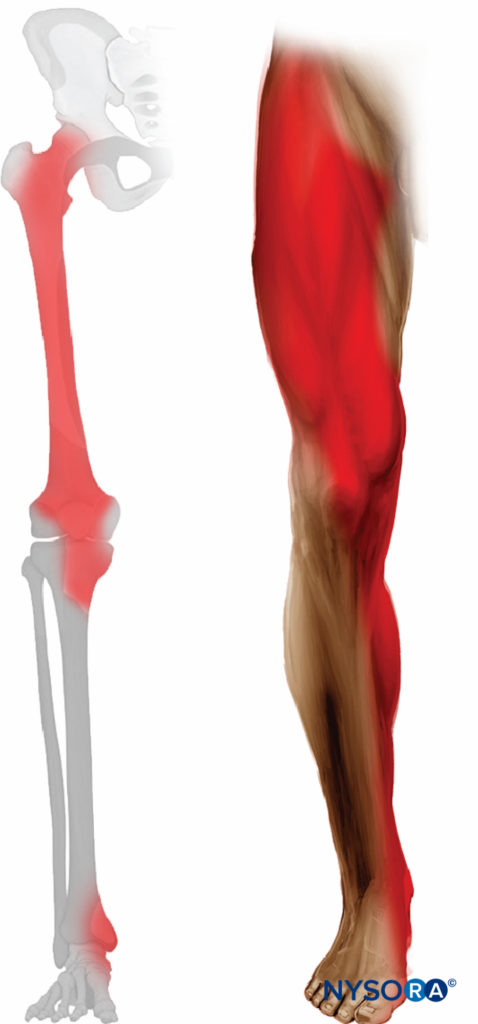
FIGURE 3. Expected distribution of fascia iliaca sensory block (lateral femorocutaneous and femoral nerves blocks).
EQUIPMENT
The equipment needed for a fascia iliaca nerve block includes the following:
- Ultrasound machine with linear transducer (6–14 MHz), sterile sleeve, and gel
- Standard nerve block tray
- Two 20-mL syringes containing local anesthetic
- 80- to 100-mm, 22-gauge needle (a short bevel aids in eliciting the fascial “pop” if desired)
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
This nerve block is typically performed with the patient in the supine position, with the bed or table flattened to maximize access to the inguinal area (Figure 1). Although palpation of a femoral pulse is a useful landmark, it is not required because the artery is quickly visualized by placement of the transducer transversely on the inguinal crease, followed by slow movement laterally or medially. Tilting the probe while pressing helps to identify the hyperechoic fascia iliaca superficial to the hypoechoic iliopsoas muscle. Medially, the femoral nerve is visualized deep to the fascia and lateral to the artery (Figure 4). Laterally, the sartorius muscle is identified by its typical triangular shape when compressed by the transducer.
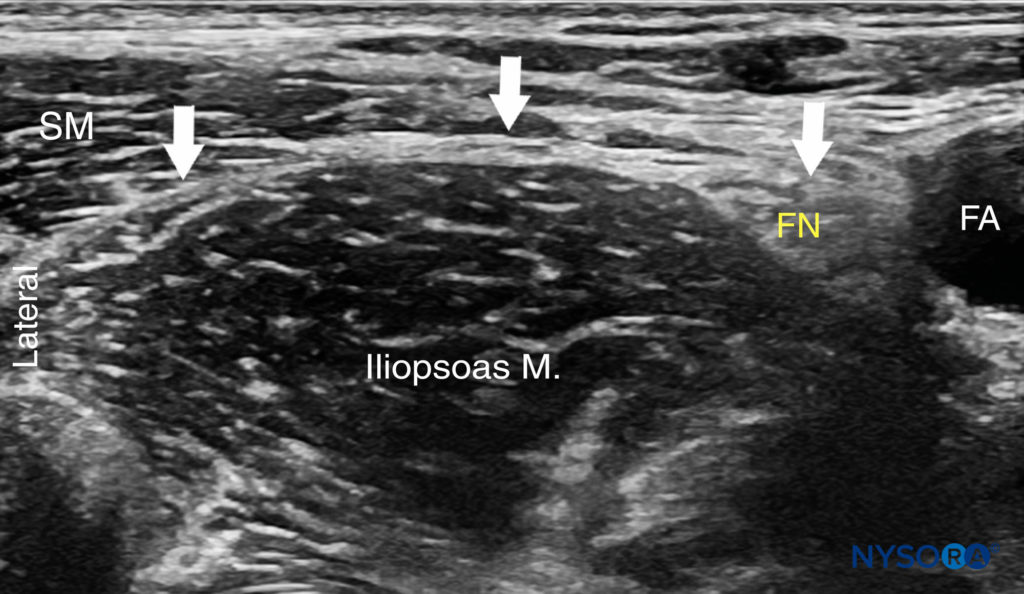
FIGURE 4. Ultrasound image of the fascia iliaca (white line and arrows) at the level of the inguinal ligament. The femoral nerve (FN) and femoral artery (FA) are visualized on the medial side and the sartorious muscle (SM) on the lateral side.
GOAL
The goal is to place the needle tip under the fascia iliaca approximately at a lateral third of the line connecting the anterior superior iliac spine to the pubic tubercle (the injection is made several centimeters lateral to the femoral artery) and to deposit a relatively large volume (20–40 mL) of local anesthetic until its spread laterally toward the iliac spine and medially toward the femoral nerve is observed with US visualization.
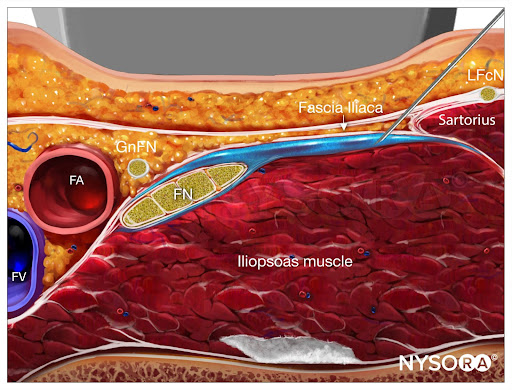
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for an infrainguinal fascia iliaca block with needle insertion in-plane and local anesthetic spread (blue). FA, femoral artery; FV, femoral vein; FN, femoral nerve; GnFN, genitofemoral nerve; LFcN, lateral femoral cutaneous nerve.
TECHNIQUE
With the patient in the proper position, the skin is disinfected and the transducer positioned to identify the femoral artery and the iliopsoas muscle and fascia iliaca. The transducer is moved laterally until the sartorius muscle is identified. After a skin wheal is made, the needle is inserted in-plane (see Figure 1). As the needle passes through fascia iliaca, the fascia is first seen indented by the needle.
As the needle eventually pierces the fascia, a “pop” may be felt, and the fascia may be seen to “snap” back on the US image. After negative aspiration, 1–2 mL of local anesthetic is injected to confirm the proper injection plane between the fascia and the iliopsoas muscle (Figure 5a, b).
If local anesthetic spread occurs above the fascia or within the substance of the muscle itself, additional needle repositions and injections may be necessary. A proper injection will result in the separation of the fascia iliaca by the local anesthetic in the medial–lateral direction from the point of injection as described.
Releasing the pressure of the transducer may reduce the resistance to injection and improve the distribution of local anesthetic. If the spread is deemed inadequate, additional injections laterally or medially to the original needle insertion or injection can be made to facilitate the medial–lateral spread. In an adult patient, 20–40 mL of local anesthetic is usually required for successful block. In children, 0.7 mL/kg is commonly used. The success of the nerve block is best predicted by documenting the spread of local anesthetic toward the femoral nerve medially and underneath the sartorius muscle laterally (Figure 5b). In obese patients, an out-of-plane technique may be favored.
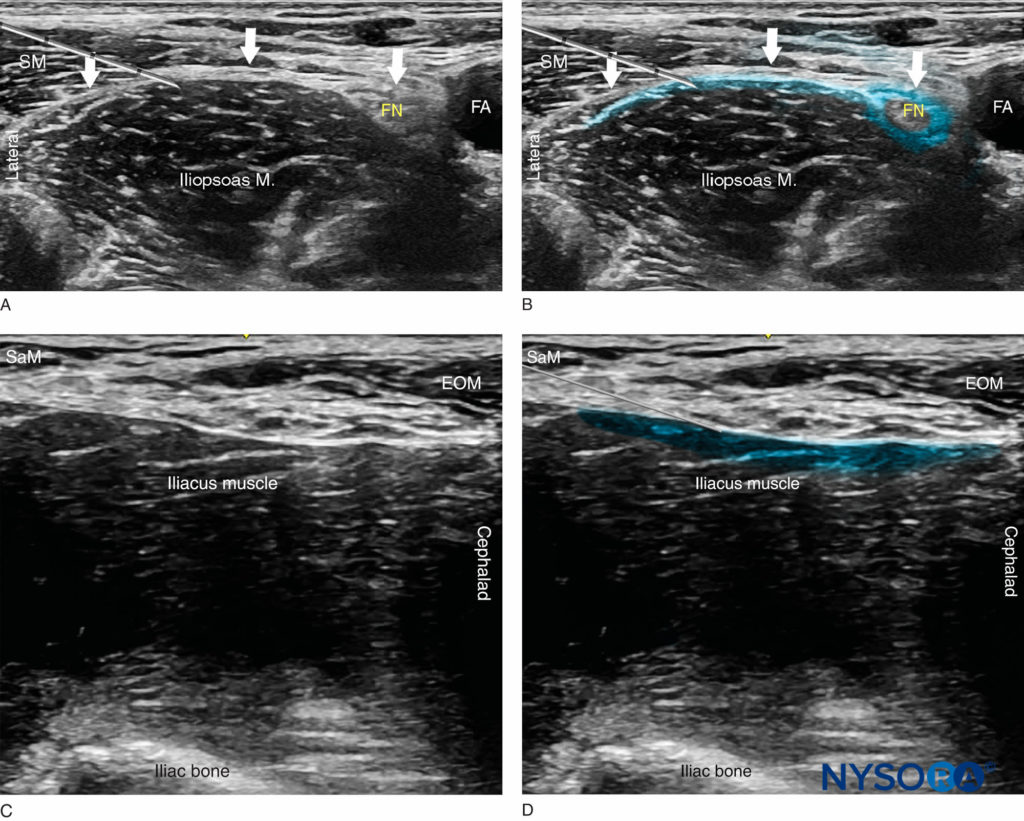
FIGURE 5. (A) Position of the needle tip for the fascia iliaca nerve block. The needle is shown underneath the fascia iliaca lateral to the femoral artery but not deep enough to be lodged in the iliac muscle. (B) A simulated spread (blue-shaded area) of local anesthetic to accomplish a fascia iliaca nerve block. (C) Ultrasound view of the supra-inguinal approach with the probe oriented in a sagittal plane along the iliacus muscle. (D) Needle path and simulated local anesthetic spread (blue-shaded area) just deep to the fascia iliaca and the external oblique muscle (EOM). SaM, sartorius muscle.
From the Compendium of Regional Anesthesia: Cognitive priming for a suprainguinal fascia iliaca block.
The nerve block should result in block of the femoral nerve in all instances (100%) and the lateral femoral nerve in most instances (80–100%). block of the anterior branch of the obturator nerve may not occur with the fascia iliaca nerve block. When required, this nerve should be blocked as described in Ultrasound-Guided Obturator Nerve block. An alternative suprainguinal technique may result in a more proximal spread and possibly more efficacious analgesia after hip surgery (Figures 5c, 5d, and 6).
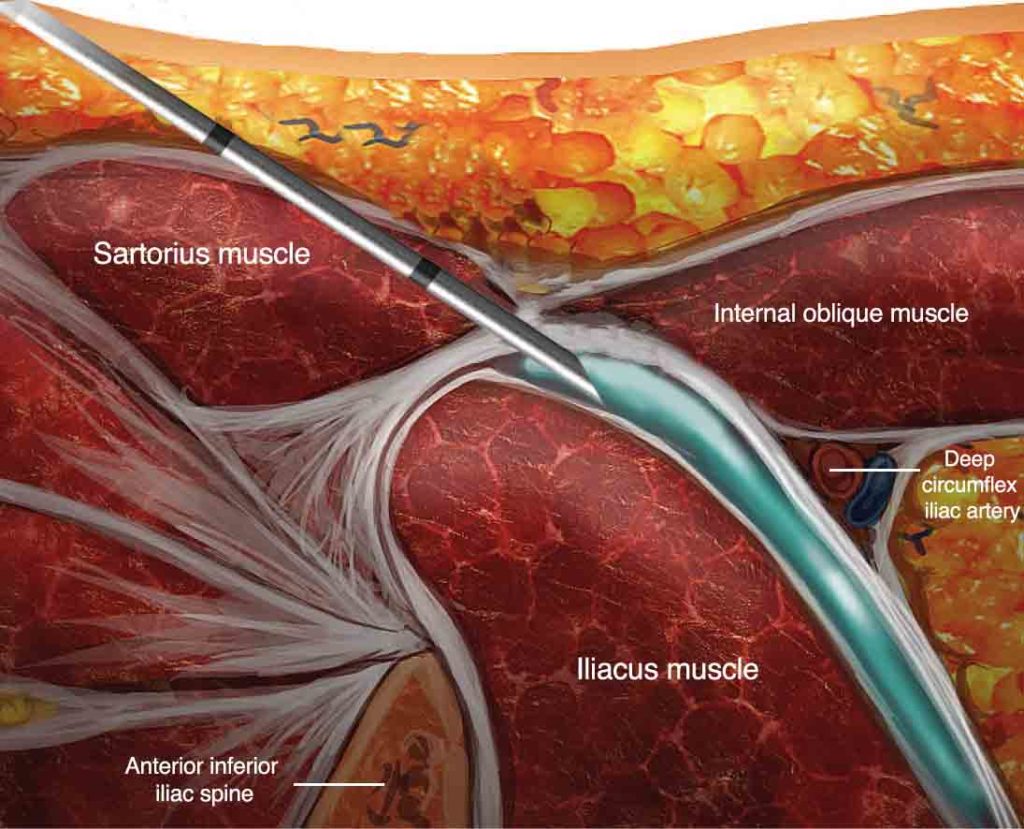
FIGURE 6. Alternative suprainguinal method to perform the fascia iliaca compartment nerve block: anatomical section in the parasagittal plane.
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for a suprainguinal fascia iliaca block with needle insertion in-plane and local anesthetic spread (blue). FN, femoral nerve; IO, internal oblique; TA, transversus abdominis; AIIS, anterior inferior iliac spine; DCA, deep circumflex artery.
TIPS
- The fascia iliaca nerve block is a large-volume nerve block. Its success depends on the spread of local anesthetic underneath the fascia iliaca. A volume of 30–40 mL of injectate is necessary to accomplish the nerve block.
- The spread of local anesthetic is monitored with ultrasonography. If the pattern of spread is not adequate (eg, the local anesthetic is collecting in one location and not “layering out”), the injection is stopped and the needle repositioned before continuing. Additional injections may be made to ensure adequate spread.
Continue reading Ultrasound-Guided Femoral Nerve Block
This text was a sample of content from the Compendium of Regional Anesthesia on the NYSORA LMS.
NYSORA’s Compendium of Regional Anesthesia is simply the most comprehensive, and practical curriculum on Regional Anesthesia from A to Z, featuring NYSORA’s Premium content. As opposed to textbooks and e-books, the Compendium is continuously updated and features NYSORA’s newest videos, animations, and visual content.
The Compendium is one of several gold-standard educational courses on NYSORA’s Learning System (the NYSORA LMS), and registration to NYSORALMS.com is free. The FULL access to the Compendium, however, is based on an annual subscription, as it requires an army of illustrators, video editors, and an educational team to continue making it the BEST tool for education on everything regional anesthesia. While you can think of the compendium as an ebook on steroids, a quick test drive will give you a real-time feel of how incredible the Compendium really is. Your subscription will transform the way you read about regional anesthesia:
- Learn visually: Everything regional, including spinal, epidural, and nerve block procedures and management protocols
- Review step-by-step techniques instructions for over 60 nerve blocks
- Access NYSORA’s fabled illustrations, animations, and videos (such as Reverse Ultrasound Anatomy)
- Access RA info on any device via the desktop platform and mobile app
- Get real-time updates
- Review infographics for exam preparation (e.g. EDRA)
- Use the Community feed with real case discussions, images and videos are posted and discussed by subscribers and world’s top experts alike.
Even if you do not wish to subscribe to the Compendium, do register to the NYSORA LMS, be the first to know what’s new in regional anesthesia, and get involved in case discussions.
Here’s what the activity feed on NYSORA LMS looks like:
We are convinced that once you experience the Compendium on the NYSORA LMS, and you’ll never go back to your old books, and your subscription will support keeping NYSORA.com free for the rest of the world.
Additional Reading
- Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d’Athis F: Comparison of the three-in-one and fascia iliaca compartment nerve blocks in adults: clinical and radiographic analysis. Anesth Analg 1998;86:1039–1044.
- Dolan J, Williams A, Murney E, Smith M, Kenny GN: Ultrasound guided fascia iliaca nerve block: a comparison with the loss of resistance technique. Reg Anesth Pain Med 2008;33:526–531.
- Weller RS: Does fascia iliaca nerve block result in obturator nerve block? Reg Anesth Pain Med 2009;34:524.
- Hebbard P, Ivanusic J, Sha S: Ultrasound-guided supra-inguinal fascia iliaca nerve block: a cadaveric evaluation of a novel approach. Anaesthesia 2011;66:300–305.
- Miller BR: Ultrasound-guided fascia iliaca compartment nerve block in pediatric patients using a long-axis, in-plane needle technique: a report of three cases. Paediatr Anaesth 2011;21:1261–1264.
- Foss NB, Kristensen BB, Bundgaard M, et al: Fascia iliaca compartment block for acute pain control in hip fracture patients: a randomized, placebo-controlled study. Anesthesiology 2007;106:773–778.
- Minville V, Gozlan C, Asehnoune K, et al: Fascia-iliaca compartment nerve block for femoral bone fracture in prehospital medicine in a 6-yr-old child. Eur J Anaesthesiol 2006;23:715–716.
- Mouzopolous G, Vasiliadis G, Lasanianos N, et al: Fascia iliaca nerve block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol 2009;10:127–133.
- Swenson JD, Bay N, Loose E, et al: Outpatient management of continuous peripheral nerve catheters placed using ultrasound guidance: an experience in 620 patients. Anesth Analg 2006;103:1436–1443.
- Wambold D, Carter C, Rosenberg AD: The fascia iliaca nerve block for postoperative pain relief after knee surgery. Pain Pract 2001;1:274–277.
- Yun MJ, Kim YH, Han MK, et al: Analgesia before a spinal nerve block for femoral neck fracture: fascia iliaca compartment nerve block. Acta Anaesthesiol Scand 2009;53:1282–1287.






