FACTS
- Indications: Femur, patella, quadriceps tendon, and knee surgery; analgesia for hip fracture
- Transducer position: Transverse, femoral crease
- Goal: Local anesthetic spread adjacent to the femoral nerve
- Local anesthetic: 10–15 mL
GENERAL CONSIDERATIONS
The ultrasound (US)-guided technique of the femoral nerve block allows the practitioner to monitor the spread of local anesthetic and needle placement and make appropriate adjustments to accomplish the desired disposition of the local anesthetic. US also may reduce the risk of femoral artery puncture. Although nerve stimulation is not required for success, motor response observed during nerve stimulation often provides contributory safety information should the needle-nerve relationship be missed by US alone.
ULTRASOUND ANATOMY
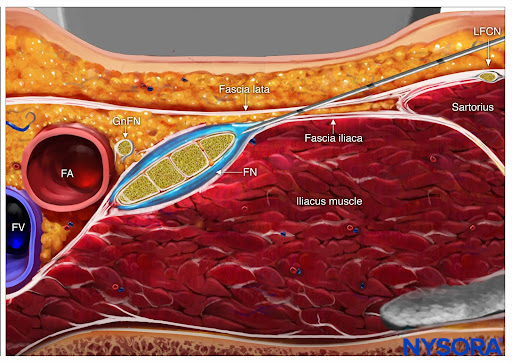
Orientation begins with the identification of the femoral artery at the level of the femoral crease. Commonly, the femoral artery and the deep artery of the thigh are both seen. In this case, the transducer should be moved proximally until only the femoral artery is seen (Figure 1a, b). The femoral nerve is lateral to the vessel and covered by the fascia iliaca; it is typically hyperechoic and roughly triangular or oval in shape (Figure 2a, b). The nerve is enveloped within two layers of the fascia iliaca. The femoral nerve typically is visualized at a depth of 2–4 cm.
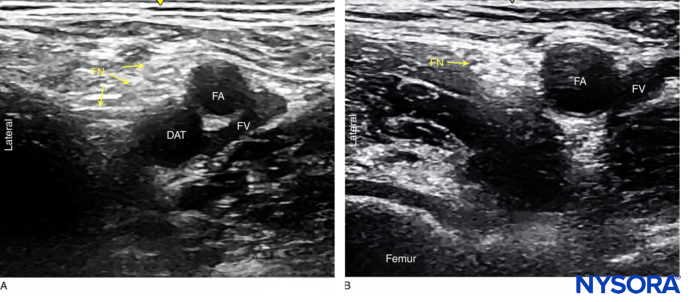
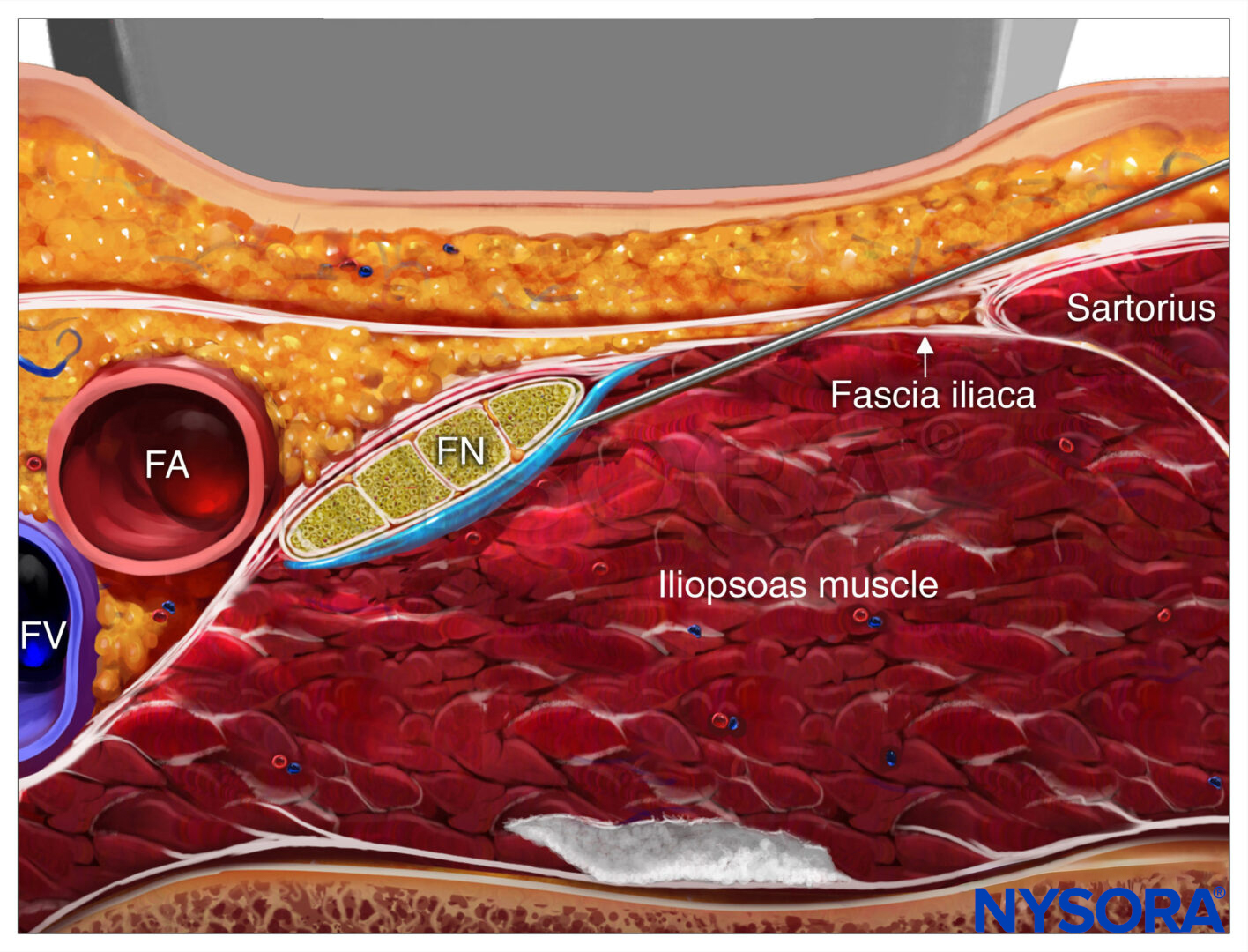
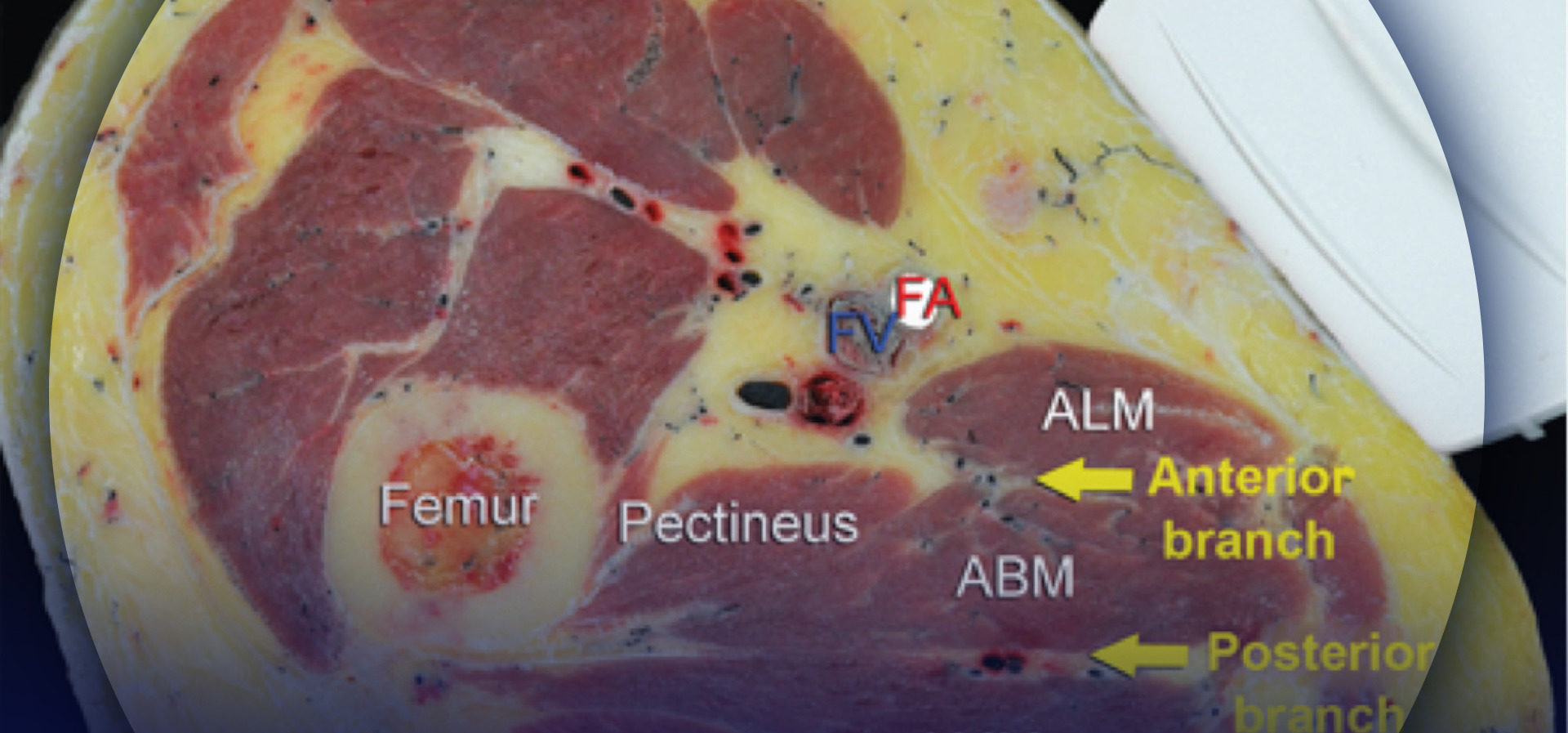
FIGURE 1. Femoral nerve (FN) as seen distally (A) and at the femoral crease (B) Note that FN is better visualized at B, before the take off the deep artery of the thigh (DAT). Femoral vein (FV) is medial to the artery.
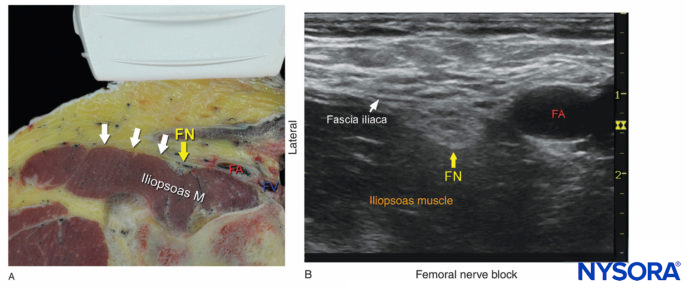
FIGURE 2. (A) Cross-sectional anatomy of the femoral nerve (FN) at the level of the femoral crease. The FN is seen on the surface of the iliopsoas muscle covered by fascia iliaca (white arrows). The femoral artery (FA) and femoral vein (FV) are seen enveloped within their own vascular fascial sheath created by one of the layers of fascia lata. (B) Sonoanatomy of the FN at the femoral triangle. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, Inc.; 2011.)
3D ANATOMY
TIPS
- Identification of the femoral nerve often is made easier by slightly tilting the transducer cranially or caudally. This adjustment helps bring out the image of the nerve, making it distinct from the background.
- Applying pressure to the transducer often optimizes the image of the femoral nerve but may collapse veins, obscuring them from the examiner’s eye. The transducer pressure also may compress the interfacial space and interfere with the adequate spread of the local anesthetic. Therefore, the transducer pressure should be released and vasculature re-ascertained before injection.
Read more about Optimizing an Ultrasound Image.
DISTRIBUTION OF ANESTHESIA
Femoral nerve block results in anesthesia of the anterior and medial thigh down to and including the knee, as well as a variable strip of skin on the medial leg and foot. It also innervates the hip, knee, and ankle joints (Figure 3).

FIGURE 3. Expected distribution of the femoral nerve block. Left -Osteotomal distribution, Right -Dermatomal distribution.
EQUIPMENT
The equipment recommended for a femoral nerve block includes the following:
- Ultrasound machine with linear transducer (8–18 MHz), sterile sleeve, and gel
- Standard nerve block tray
- One 20-mL syringe containing local anesthetic
- A 50- to 100-mm, 22-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Injection pressure monitor
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
This nerve block typically is performed with the patient in the supine position, with the bed or table flattened to maximize operator access to the inguinal area. The transducer is placed transversely on the femoral crease, over the pulse of the femoral artery, and moved slowly in a lateral-to-medial direction to identify the artery.
NYSORA Tips
In such cases, using a wide silk tape to retract the abdomen is a useful maneuver prior to skin preparation and scanning (Figure 4).

FIGURE 4. Obesity is common in patients who present with an indication for femoral nerve block. Taping the adipose tissue away helps optimize exposure to the femoral crease in patients with morbid obesity.
GOAL
The goal is to place the needle tip immediately adjacent to the lateral aspect of the femoral nerve, below the fascia iliaca or between the two layers of the fascia iliaca, that surround the femoral nerve. Proper deposition of local anesthetic is confirmed either by observation of the femoral nerve being displaced by the injectate or by the spread of the local anesthetic above or below the nerve, surrounding and separating it from the fascia iliaca layers.
TECHNIQUE
With the patient in the supine position, the skin over the femoral crease is disinfected and the transducer is positioned to identify the femoral artery and nerve. If the nerve is not immediately apparent lateral to the artery, tilting the transducer proximally or distally often helps to image and highlight the nerve from the iliacus muscle and the more superficial adipose tissue. In doing so, an effort should be made to identify the iliacus muscle and its fascia, as well as the fascia lata, because injection underneath a wrong fascial sheath may result in nerve block failure. Once the femoral nerve is identified, a skin wheal of local anesthetic is made 1 cm away from the lateral edge of the transducer. The needle is inserted in-plane in a lateral to medial orientation and advanced toward the femoral nerve (Figure 5).
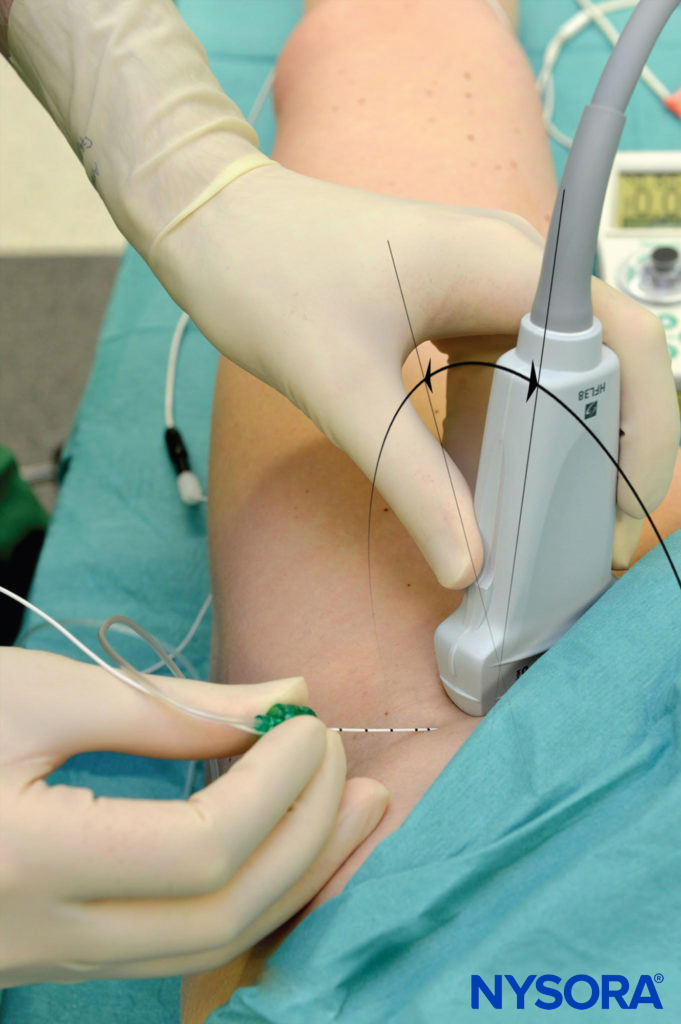
FIGURE 5. Transducer position and needle insertion using an in-plane technique to nerve block the femoral nerve at the femoral crease.
If nerve stimulation is used (0.5 mA, 0.1 msec), the passage of the needle through the fascia iliaca and contact of the needle tip with the femoral nerve usually is associated with a motor response of the quadriceps muscle group. In addition, a needle passage through the fascia iliaca is often felt. Once the needle tip is adjacent (either above, below, or lateral) to the nerve (Figure 6), and after careful aspiration, 1–2 mL of local anesthetic is injected to confirm proper needle placement (Figures 7 and 8). Proper injection will push the femoral nerve away from the injection.
Additional needle repositions and injections are done only when necessary. Anatomic variations have been described with aberrant positions of the femoral nerve. In an adult patient, 10–15 mL of local anesthetic is adequate for a successful nerve block.
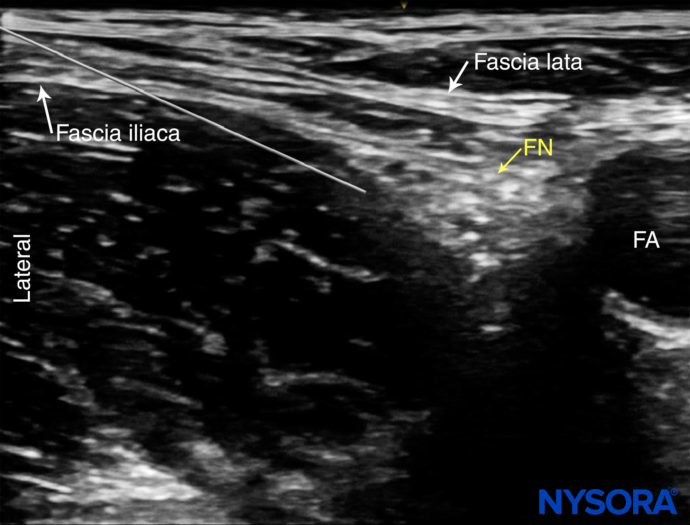
FIGURE 6. Ultrasound image of the needle path to nerve block the femoral nerve. The needle pierces the fascia iliaca lateral to the femoral nerve (FN) and the needle tip is advanced along the deep border of the nerve. FA, femoral artery.
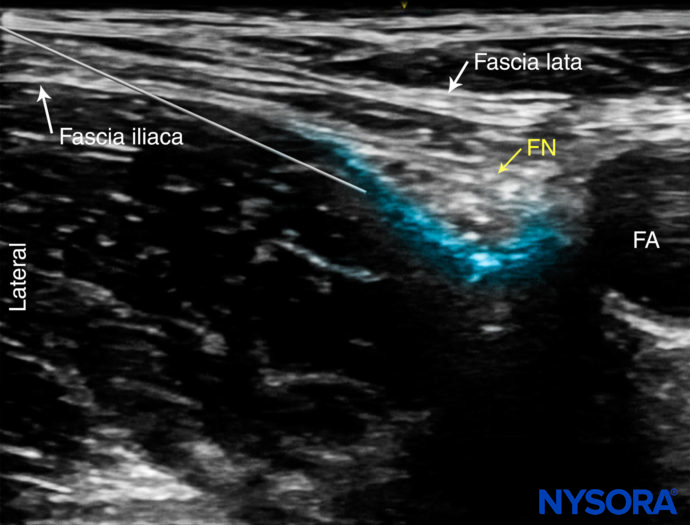
FIGURE 7. Simulated needle path and spread of local anesthetic (blue-shaded area) to nerve block the femoral nerve (FN). FA, femoral artery.
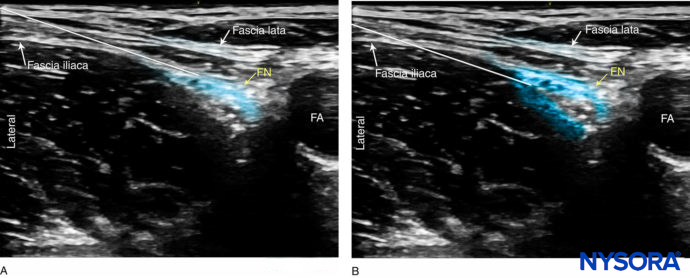
FIGURE 8. Simulated needle paths and local anesthetic spread to nerve block the femoral nerve (FN). (A) The needle tip is advanced in between the fascia iliaca and the nerve and the local anesthetic deposited superficially to the nerve. (B) The tip is located just lateral to the femoral nerve nerve, in between the two layers surrounding the nerve. FA, femoral artery.
TIPS
- Never inject against high resistance to injection because this may signal an intrafascicular needle placement or needle tip position in a wrong fascial plane.
- Circumferential spread of local anesthetic around the nerve is not necessary for this nerve block. A pool of local anesthetic immediately adjacent to either the posterolateral or the anterior aspects is sufficient.
- Locate the femoral vein, releasing pressure on the transducer, using color Doppler if needed. The femoral vein is typically medial to the artery, but it can occasionally lie deep or even lateral to it. It is often compressed by the probe during nerve block performance; being aware of the position of the vein helps decrease the risk of inadvertent intravascular injection.
- Applying forceful pressure to the transducer will compress the tissue below it, making injection more difficult and possibly interfering with the spread between the fascial layers.
- Following hip arthroscopy, landmarks might be displaced by fluid extravasation, with the artery and the nerve significantly deeper than their preoperative position.
CONTINUOUS ULTRASOUND-GUIDED FEMORAL NERVE BLOCK
The goal of the continuous femoral nerve block is the placement of the catheter within the vicinity of the femoral nerve just deep to the fascia iliaca. The procedure consists of five steps: (1) needle placement; (2) injection through the needle to confirm needle placement in the proper tissue plane; (3) catheter advancement; (4) injection through the catheter to assure its therapeutic position; (5) securing the catheter. For the first two phases of the procedure, US can be used to ensure accuracy in most patients. The in-line approach from the lateral-to-medial direction is the most common method because the out-of-plane approach holds greater risk for puncture of the femoral nerve if the needle is introduced directly above the nerve (Figure 9). Alternative approaches, such as the oblique approach, have also been suggested.

FIGURE 9. Continuous femoral nerve block. The needle is seen inserted in plane approaching the nerve in a lateral-to-medial direction. Although it would seem intuitive that a longitudinal needle insertion would have advantages, the technique demonstrated here is simpler and commonly used. The catheter should be inserted 2–4 cm past the needle tip.
NYSORA Tips
• With US guidance, nonstimulating catheters are used for continuous femoral nerve block. Stimulating catheters require a longer insertion time, without improvement in analgesia. Stimulating catheters also may lead to unnecessary needle and catheter manipulation to obtain the motor response, when in fact the catheter is often in the proper place even when there is no motor response.
• Adequate catheter placement with US guidance is confirmed by disposition of the local anesthetic in the proper anatomical space rather than by motor stimulation.
For a detailed description, please refer to “Continuous US-guided nerve block”.
In general, the inguinal area is quite mobile, and the femoral nerve is shallow, both of which predispose to catheter dislodgment. The more lateral the starting point for needle insertion for continuous femoral nerve block, the longer the catheter would be within the iliacus muscle, which may help prevent dislodgment because muscle tends to stabilize a catheter better than adipose tissue. A common empirical infusion regimen for femoral nerve block in an adult patient is ropivacaine 0.2% at an infusion rate of 5 mL/h with a 5 mL/h patient-controlled bolus.
Read more about Ultrasound-Guided Adductor Canal Nerve Block
Supplementary video related to this block can be found at Ultrasound-Guided Femoral Nerve Block Video
Clinical updates
Tsai et al. (Journal of Clinical Medicine, 2022) report in a retrospective cohort of 607 geriatric ED patients with hip fracture that a lidocaine-based single-shot ultrasound-guided femoral nerve block (USFNB) reduced opioid use by ~80% compared with standard care and achieved meaningful pain relief 2.37× faster. Despite faster and opioid-sparing analgesia, ED and hospital length of stay were unchanged, and no block-related complications were observed, supporting USFNB as a safe, rapid, non-opioid analgesic strategy for early hip fracture pain control in older adults.
- Read more about the study HERE.
Ogawa et al. (Injury, 2021) report in a propensity score–matched pilot study of 78 elderly hip fracture patients (mean age 87 years, ~40% with dementia) that a single-shot femoral nerve block (FNB) performed intraoperatively under spinal anesthesia was associated with better early functional recovery, and improved mobility on postoperative day 2. The benefit was most evident among patients without dementia and those with femoral neck fractures; however, hospital length of stay was unchanged, suggesting that FNB may enhance early mobility rather than accelerate discharge.
- Read more about the study HERE.