FACTS
• Indications: saphenous vein stripping or harvesting; supplementation for medial foot/ankle surgery in combination with a sciatic nerve block, and analgesia for knee surgery in combination with multimodal analgesia.
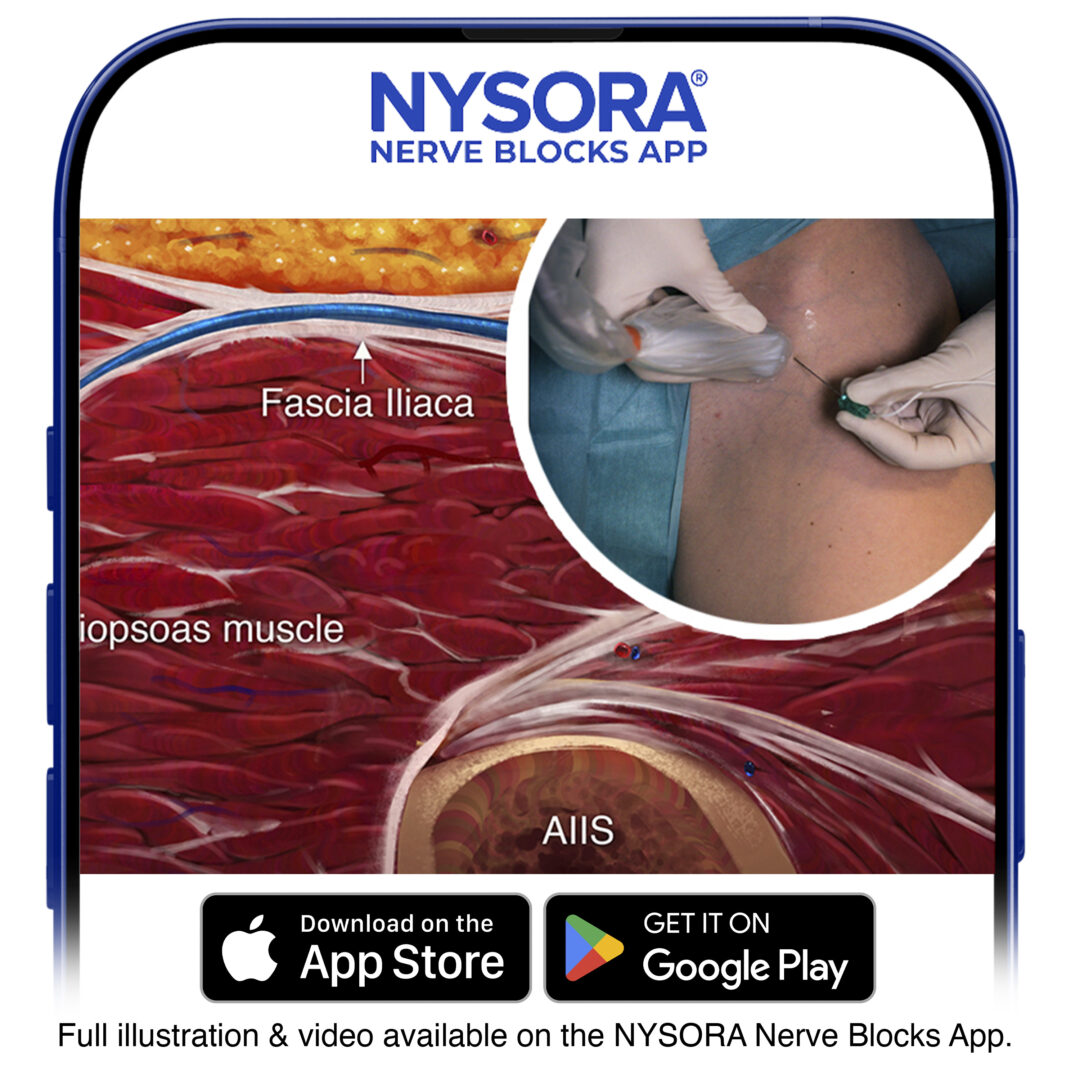
• Transducer position: transverse on the anteromedial thigh at the junction between the middle and distal third of the thigh or below the knee at the level of the tibial tuberosity, depending on the approach chosen (proximal or distal) (Figure 1)
• Goal: local anesthetic spread lateral to the femoral artery and deep to the sartorius muscle or more distal, below the knee, adjacent to the saphenous vein.
• Local anesthetic: 5–10 mL
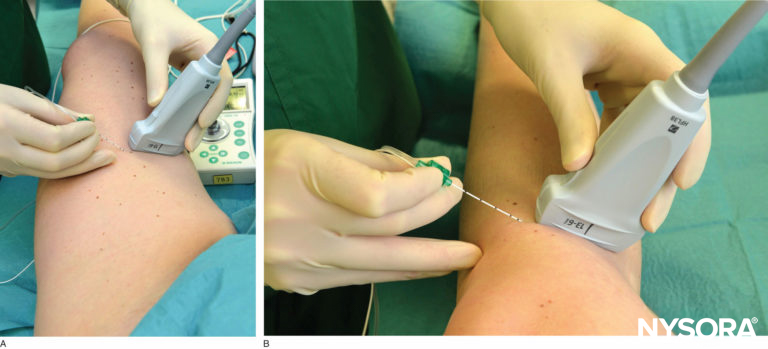
FIGURE 1. Transducer position and needle insertion to nerve block the saphenous nerve (A) at the level of the lower third of the thigh and (B) below the knee.
GENERAL CONSIDERATIONS
The saphenous nerve is a terminal sensory branch of the femoral nerve. It supplies innervation to the medial aspect of the leg down to the ankle and foot. It also sends infrapatellar branches to the knee joint. A saphenous nerve block is useful as a supplement to sciatic nerve block for foot and ankle procedures that involve the medial aspect of the malleolus and the foot. The nerve block has also been reported as a supplement to multimodal analgesia protocols in patients having knee arthroplasty. Typically, a more proximal (mid-thigh) approach and a larger volume of local anesthetic is used for this “adductor canal nerve block”. Several approaches have been described to nerve block the saphenous nerve along its route from the inguinal area to the medial malleolus (Figure 2). The use of ultrasound (US) guidance has improved the success rates of the saphenous nerve blocks compared with field nerve blocks below the knee and blind trans-sartorial approaches.
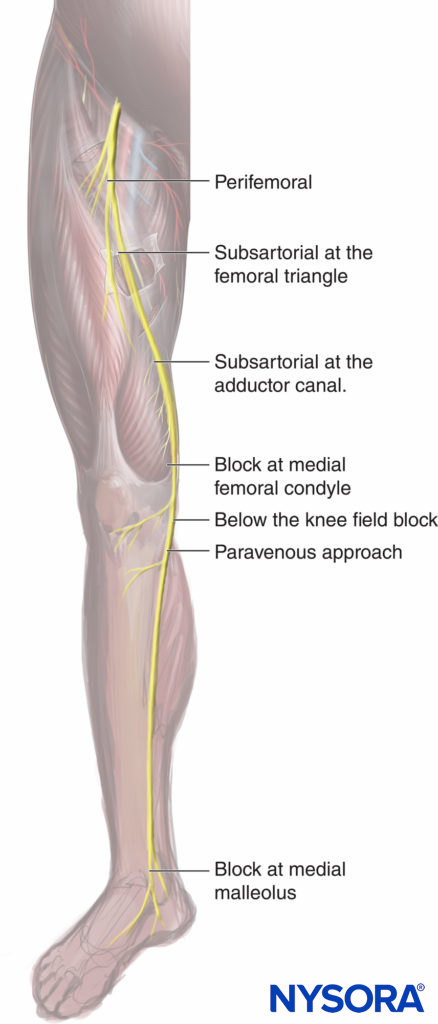
FIGURE 2. Various approaches to the saphenous nerve block: the perifemoral typically targets the nerve to the vastus medialis muscle with nerve stimulation; the subsartorial at the femoral riangle; subsartorial at the adductor canal; at the medial femoral condyle, between the tendons of the sartorius and the gracilis muscle; once the femoral vessels have crossed the adductor hiatus to become the popliteal vessels; the paravenous approach using the saphenous vein as a landmark at the level of the tibial tuberosity; and at the level of the medial malleolus.
ULTRASOUND ANATOMY
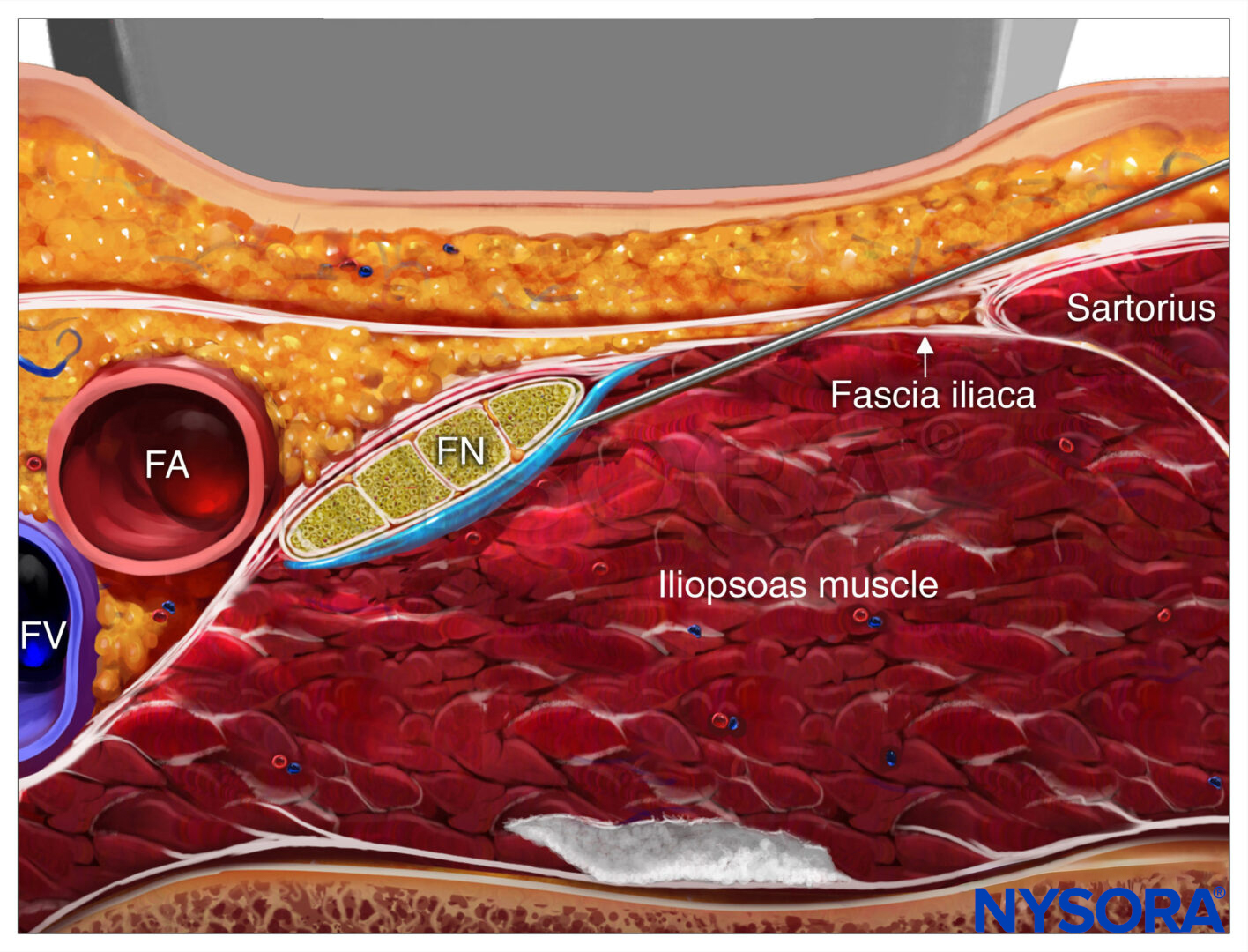
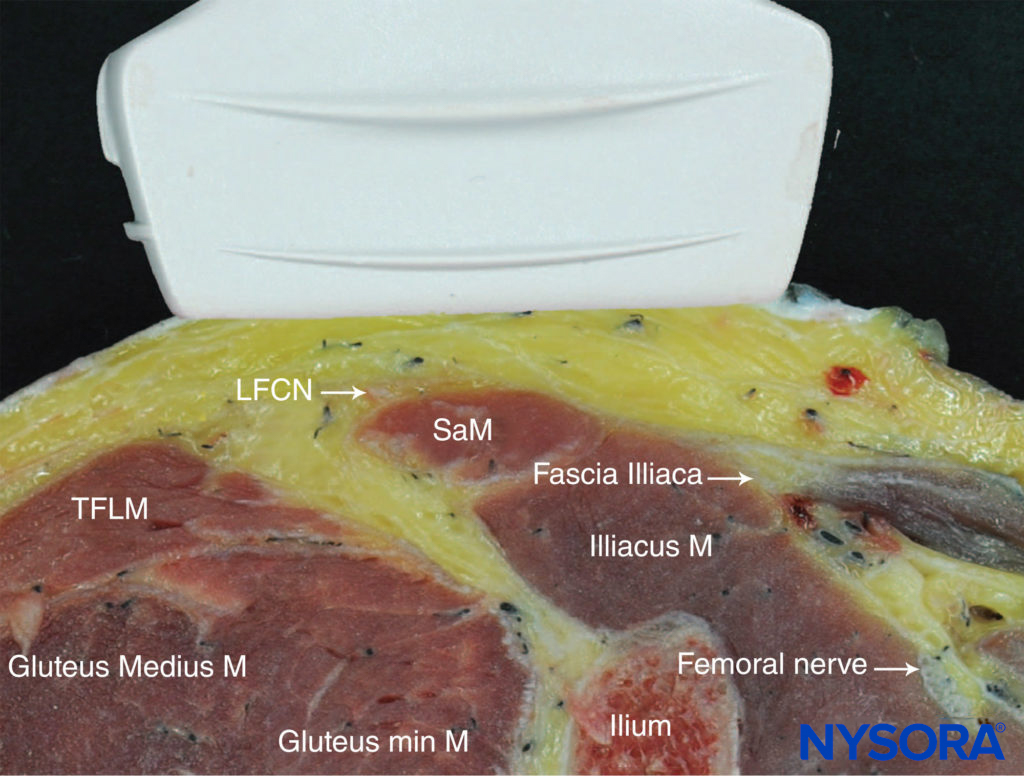
The sartorius muscle descends in a lateral to the medial direction across the anterior thigh and forms a “roof ” over the adductor canal in the lower half of the thigh. The muscle appears as a trapezoid shape beneath the subcutaneous layer of adipose tissue.
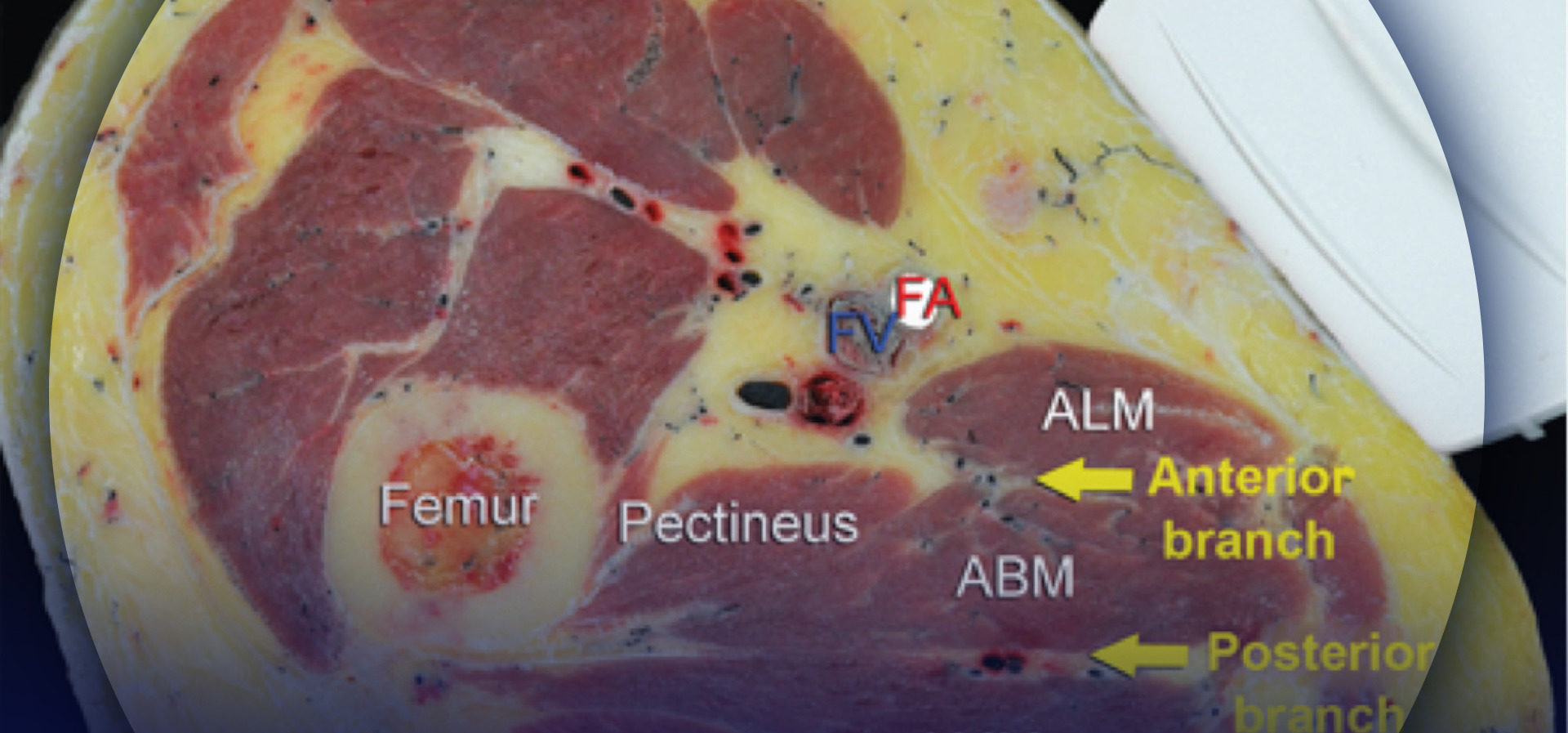
The sides of the triangular canal are formed by the vastus medialis laterally and the adductor longus or magnus medially (depending on how proximal or distal the scan is). The saphenous nerve is typically imaged by ultrasound as a small, round, hyperechoic structure anterior to the artery. The femoral vein accompanies the artery and saphenous nerve, which all can be identified at a depth of 2–3 cm (Figure 3).
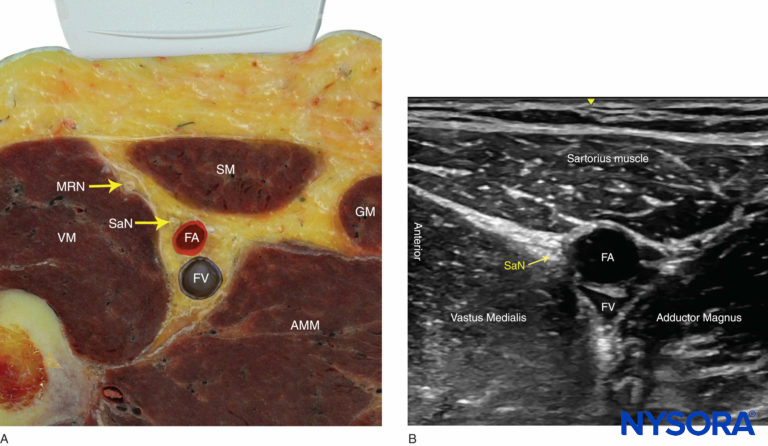
FIGURE 3. (A) Cross-sectional anatomy of the saphenous nerve at the level of the thigh. The saphenous nerve (SaN) is positioned between the sartorius muscle (SM) and the vastus medialis muscle (VM), anterolateral to the femoral artery (FA) and vein (FV). AMM, adductor magnus muscles; GM, gracilis muscle; MRN, medial retinacular nerve. (B) US anatomy of the subsartorial space at the midthigh.
When attempting to identify the saphenous nerve on US image, the following anatomical considerations should be kept in mind:
- Above the knee: The saphenous nerve pierces the fascia lata between the tendons of the sartorius and gracilis muscles before becoming a subcutaneous nerve.
- The saphenous nerve lies in close proximity to several vessels along its trajectory: the femoral artery above the knee, the descending genicular artery and its saphenous branch at the knee, and the great saphenous vein in the lower leg and ankle.
- Below the knee, the saphenous nerve passes along the tibial side of the leg, adjacent to the great saphenous vein subcutaneously (Figure 4).
- At the ankle, branches of the saphenous nerve are located medially, next to the subcutaneously positioned saphenous vein.
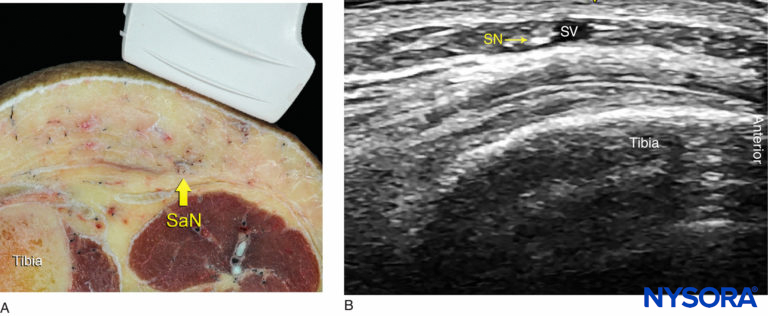
FIGURE 4. (A) Cross-sectional anatomy of the saphenous nerve (SaN) at the level of the tibial tuberosity. (B) US image of the SaN below the knee. The SaN is seen within the immediate vicinity of the great saphenous vein (SV). The transducer should be applied lightly to avoid compression of the SV because the vein serves as an important landmark for the technique.
DISTRIBUTION OF ANESTHESIA
The saphenous nerve block results in anesthesia of the skin on the medial leg and foot (Figure 5). For a more comprehensive review of the femoral and saphenous nerve distributions, see Functional Regional Anesthesia Anatomy. Of note, although the saphenous nerve block is a sensory nerve block, an injection of a large volume of local anesthetic into the subsartorial space can result in a partial motor nerve block of the vastus medialis due to the nerve block of the femoral nerve branch to this muscle, often contained in the canal. For this reason, caution must be taken when advising patients regarding the safety of unsupported ambulation after undergoing a proximal saphenous nerve block.
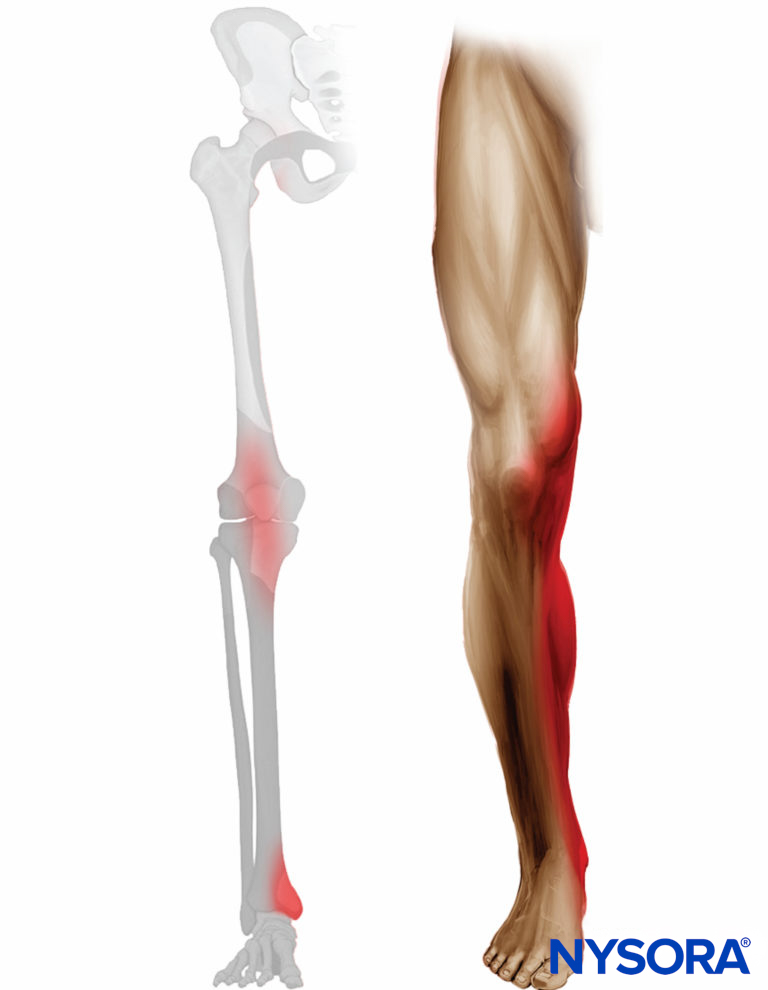
FIGURE 5. Expected distribution of analgesia after saphenous nerve block at the level of midthigh.
EQUIPMENT
- Ultrasound machine with a linear transducer (8–14 MHz), sterile sleeve, and gel
- Standard nerve block tray
- One 10-mL syringe containing local anesthetic
- An 80 mm 22-25 gauge needle
- Peripheral nerve stimulator to elicit paresthesia
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks here.
LANDMARKS AND PATIENT POSITIONING FOR THE PROXIMAL APPROACH
The patient is placed in any position that allows for comfortable placement of the US transducer and needle advancement. This nerve block typically is performed with the patient in the supine position, with the thigh abducted and externally rotated to allow access to the medial thigh (see Figure 1a).
GOAL
The goal is to place the needle tip just anterior to the femoral artery, deep to the sartorius muscle, and to deposit 5–10 mL (or up to 20 mL for the adductor canal nerve block) of local anesthetic until its spread around the artery is confirmed with US visualization. Nerve Block of the nerve at other, more distal and superficial locations consists of a simple subcutaneous infiltration of the tissues within the immediate vicinity of the nerve under US guidance.
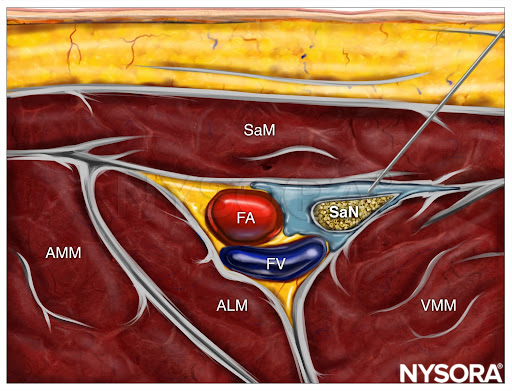
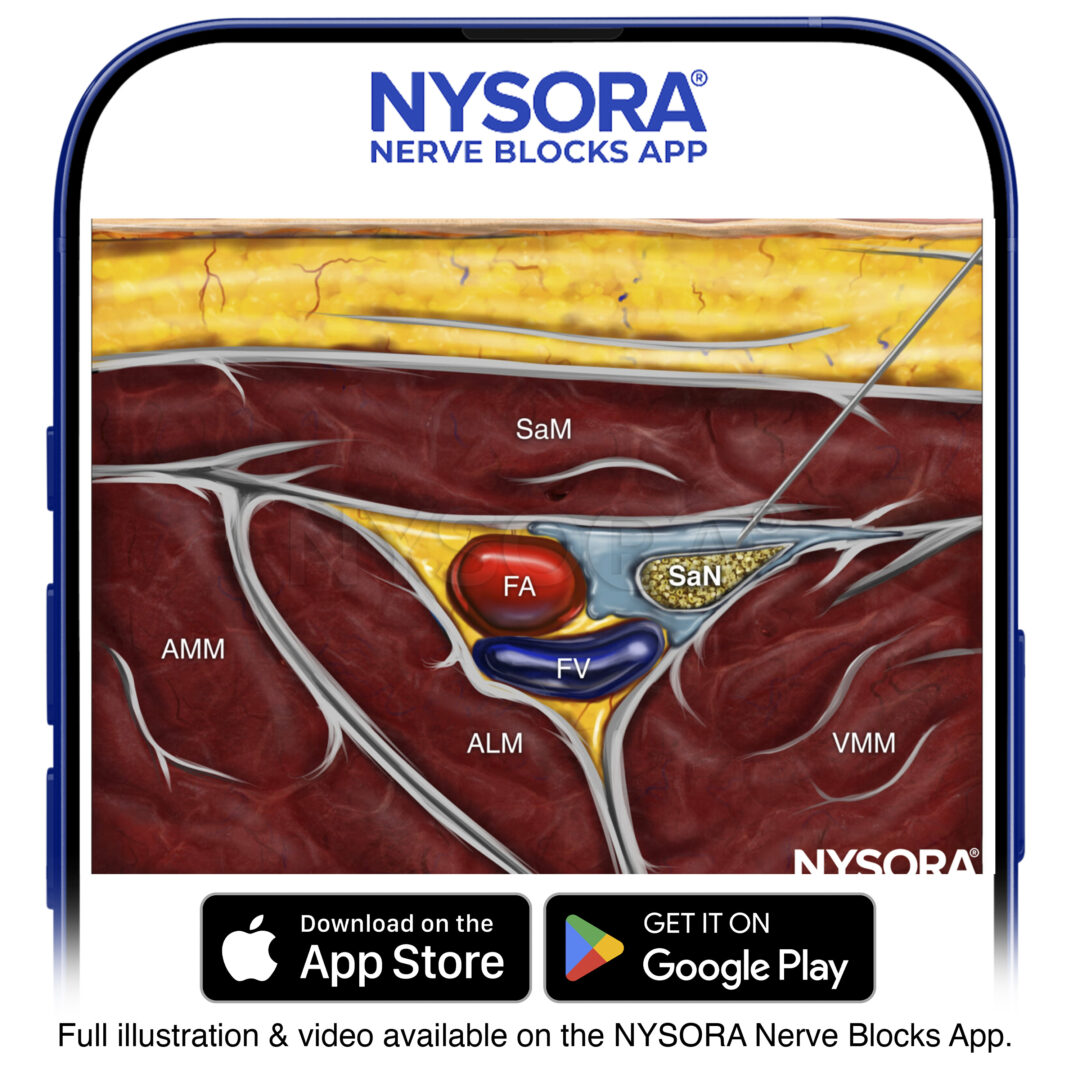
From the Regional Anesthesia Manual: Reverse Ultrasound Anatomy for an adductor canal block with needle insertion in-plane and local anesthetic spread (blue). FA, femoral artery; FV, femoral vein; AMM, adductor magnus muscle; ALM, adductor longus muscle; VMM, vastus medialis muscle; SaM, sartorius muscle; SaN, saphenous nerve.
TECHNIQUE
The skin is disinfected and the transducer is placed anteromedially, approximately at the junction between the middle and distal third of the thigh or somewhat lower. If the artery is not immediately obvious, several maneuvers can be used to identify it, including color Doppler scanning to trace the femoral artery caudally from the inguinal crease. Once the femoral artery has been identified, the probe is moved distally to trace the artery until it passes through the adductor hiatus to become the popliteal artery.
The saphenous nerve block should be performed at the most distal level where the artery still lies immediately deep to the sartorius muscle, thus minimizing the amount of motor nerve block of the vastus medialis; an adductor canal nerve block is typically performed more proximally, around the mid-thigh level. The needle is inserted in-plane in a lateral-to-medial orientation and advanced toward the femoral artery (Figure 1a and 6). If nerve stimulation is used (1 mA, 1 msec), the passage of the needle through the sartorius and/or adductor muscles and into the adductor canal is usually associated with paresthesia in the saphenous nerve distribution. Once the needle tip is visualized anterior to the artery and after careful aspiration, 1–2 mL of local anesthetic is injected to confirm the proper injection site (Figure 6). When injection of local anesthetic does not appear to result in its spread around the femoral artery, additional needle repositions and injections may be necessary.
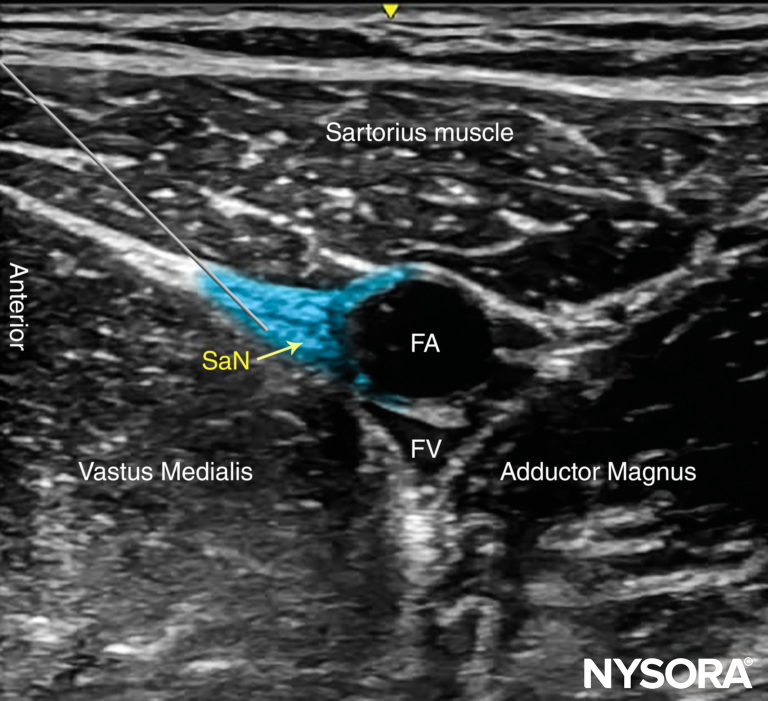
FIGURE 6. Simulated needle path, needle tip position and local anesthetic initial distribution (blue-shaded area) to anesthetize the Saphenous nerve (SaN) at the level of the thigh. FA, femoral artery: FV, femoral vein.
Color Doppler can be used to locate the peri-saphenous branch of the descending geniculate artery in order to avoid puncturing it. Because the saphenous nerve is a purely sensory nerve, high concentrations of local anesthetic are not required and in fact may delay patient ambulation should local anesthetic spread to one of the motor branches of the femoral nerve innervating the quadriceps muscle.
TIPS
- An out-of-plane technique can also be used through the belly of the sartorius muscle. Because the needle tip may not be seen throughout the procedure, small boluses of local anesthetic are administered (0.5–1 mL) as the needle is advanced toward the adductor canal to confirm the location of the needle tip.
- Visualization of the nerve is not necessary for this nerve block, as the saphenous nerve is not always well imaged. Administration of 5–10 mL of local anesthetic next to the artery in the plane between the sartorius and vastus medialis muscles should suffice without confirming nerve position.
- Practitioners should be aware of the potential for partial quadriceps weakness following a more proximal approach along the subsartorial space and/or injection of a large volume (20-30 mL) of local anesthetic. Patient education and assistance with ambulation should be encouraged. For that reason, it is recommended to perform this nerve block as distally as practically possible.
Additional reading Ultrasound-Guided Femoral Nerve Block.
Clinical updates
Gleicher et al. (Regional Anesthesia & Pain Medicine, 2025) report in a double-blinded randomized controlled trial of 60 outpatient or short-stay TKA patients that continuous adductor canal block (CACB) significantly improves early recovery compared with single-injection ACB, with ~20-point higher QoR-15 scores on postoperative days 1–3—well above the minimal clinically important difference. CACB also reduced pain scores and opioid consumption through postoperative day 3 without increasing complications, catheter-related adverse events, or length of stay. These findings support outpatient CACB, when performed with validated catheter techniques, as a superior strategy to mitigate rebound pain and enhance recovery in fast-track TKA pathways.
- Read more about the study HERE.
Kampitak et al. (Regional Anesthesia & Pain Medicine, 2025) report in a randomized non-inferiority trial of 140 total knee arthroplasty patients that a low-dose CACB bolus (10 mL 0.15% bupivacaine) provides noninferior analgesia to a traditional 20 mL 0.25% bolus at 6 and 12 hours postoperatively when combined with local infiltration analgesia and an iPACK block. Pain scores, opioid consumption, time to rescue analgesia, functional recovery, and length of stay were comparable through postoperative day 10, with slightly higher quadriceps strength on POD1 and higher patient satisfaction on POD10 in the low-dose group. These findings support reducing bolus dose and concentration for CACB to limit local anesthetic exposure without compromising analgesic efficacy in multimodal TKA pathways.
- Read more about the study HERE.
Gleicher et al. (Regional Anesthesia & Pain Medicine, 2024) report in a randomized trial of 98 total knee arthroplasty patients that placing a continuous adductor canal catheter using the ISAFE approach (interfascial space between the sartorius muscle and femoral artery) significantly reduces catheter migration toward the saphenous nerve compared with a conventional technique. Despite improved catheter stability, pain scores, opioid consumption, quadriceps weakness, and length of stay were similar between groups through postoperative day 2. These findings suggest ISAFE improves the technical reliability of catheter placement, though whether this translates into clinically meaningful outcome benefits remains uncertain.
- Read more about the study HERE.