INTRODUCTION
Continuous peripheral nerve blocks are accomplished by infusion or intermittent boluses of local anesthetic solutions. Overwhelming plethora of options are available for nearly every aspect of continuous infusion administration, from the choice of infusate to choice of infusion rate and bolus regimen, to infusion pump selection. An ideal perineural local anesthetic solution would provide analgesia while minimizing sensory, motor, and proprioception deficits. In addition, desirable attributes include a favorable toxicity profile and costefficacy. The optimal infusion strategy may be modified for the large number of clinical scenarios that the regional anesthesiologist will encounter in daily practice. Considerations include the indication for perineural catheter placement, the number and location of catheters, patient weight, and ambulatory versus inpatient status.
INFUSATES AND LOCAL ANESTHETIC CONCENTRATION
Local anesthetics were described in continuous perineural infusions as early as 1946. Intermediate-duration local anesthetics such as mepivacaine have been used, but long-acting local anesthetics such as ropivacaine, bupivacaine, and levobupivacaine are most frequently described. These long-acting agents provide a favorable differential sensory-to-motor block. At the termination of an infusion, it is desirable for sensory and motor block to resolve quickly and predictably. Studies have suggested that sensory-and-motor block regresses faster with ropivacaine than with bupivacaine. It is currently unclear if local anesthetic concentration—or simply the total delivered dose—influences continuous block effects. While the evidence suggests that for infusions involving the femoral nerve, local anesthetic concentration is of minimal importance compared with total dose, data for the sciatic nerve are lacking, and the brachial plexus information is conflicting. Therefore, at this time it remains unknown if there is an “optimal” concentration of local anesthetic. Commonly described concentrations include ropivacaine 0.1%–0.4%, bupivacaine 0.125%–0.15%, and levobupivacaine 0.1%–0.125%.
NYSORA Tips
An infusion with ropivacaine 0.1%–0.2% is easier to titrate due to faster resolution of an insensate extremity but bupivacaine 0.1%–0.125% provides the same degree of analgesia and costs less in most regions and hospitals.
LOCAL ANESTHETIC DELIVERY STRATEGIES
Infusates are typically delivered using an infusion pump with a basal infusion, bolus dose, or combination of the two modalities. Regimens are often reported as basal rate (mL/hour)/bolus volume (mL)/bolus lockout time (minutes). The delivery regimen should minimize total local anesthetic consumption, supplemental opioid requirements, and disturbance of daily functioning/sleep. No single delivery regimen has proven ideal for all anatomic locations and clinical situations. In many cases, providing a basal infusion minimizes breakthrough pain and supplemental analgesic requirements. Adding a patient-controlled bolus usually decreases the required basal infusion rate incidence of an insensate extremity, and local anesthetic consumption, the last allowing for a longer infusion duration in the ambulatory setting. For example, in the upper extremity, an interscalene infusion that includes a basal infusion has been found superior to a bolus-only regimen. Regarding specific basal infusion rates, the evidence is mixed, with many studies reporting few differences among various rates. One study involving interscalene catheters suggested that a relatively large basal rate with small-volume bolus doses (8 mL/h basal, 2-mL bolus, 60-minute lockout) provides improved analgesia and functioning, but with higher overall local anesthetic consumption compared with a slower basal rate and larger bolus doses. At the infraclavicular location, utilizing a basal infusion with bolus (in comparison to basal only or bolus only) also has been found to provide improved analgesia with decreased severity and incidence of breakthrough pain, sleep disturbances, as well as higher patient satisfaction. Studies of axillary catheters are mixed. In the lower extremity, some differences in dosing effects have been found in randomized controlled trials (RCTs) examining femoral versus popliteal sciatic locations. Findings of RCTs at the femoral or fascia iliaca location have not demonstrated an overwhelming preference for a specific regimen. Sensory and motor effects are similar when comparing repeated, scheduled hourly bolus doses to a continuous basal infusion of the same hourly volume and dose. Nearly all studies reported the total local anesthetic dose reduced with bolus-only dosing.
NYSORA Tips
Analgesia is optimized with an infusion pump that delivers both an adjustable basal rate and patient-controlled bolus doses.
INFUSATE ADDITIVES AND ADJUVANTS
Adjuvant pharmaceuticals have been added to the local anesthetic infusate in an attempt to improve analgesia quality, spare local anesthetic consumption, and minimize motor block. Many substances have been described with single-injection regional techniques. However, no analogous, clinically relevant benefits have been demonstrated for continuous peripheral nerve blocks. In addition, no additive medications are currently approved for continuous perineural administration, and some additives that have been reported in clinical trials have unacceptable side effects.
NYSORA Tips
At this time, there are few data to support adding additives (adjuvants) to local anesthetic for perineural infusions.
INFUSION PUMPS
While intermittent clinician-administered boluses are theoretically possible, simply logistical considerations explain why most local anesthetic is administered using an infusion pump. The device used for administering a continuous infusion should be accurate, reliable, portable, and programmable. It is desirable for the pump to be quiet, inexpensive, and easy to refill. In the ambulatory setting, the local anesthetic reservoir should accommodate enough infusate for 2 to 3 days. Pumps can be arbitrarily categorized as nonelectronic and electronic (Figure 1). Examples of nonelectronic mechanisms include spring- and vacuum-powered devices, as well as elastomeric pumps.
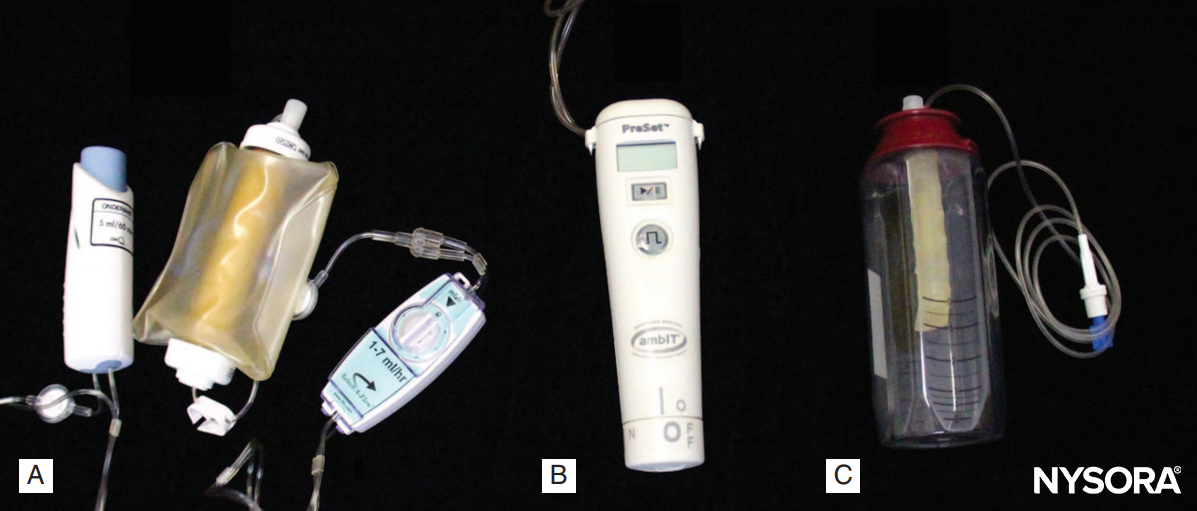
FIGURE 1. Examples of three infusion pumps designed for perineural local anesthetic infusion. A: An elastomeric device with adjustable basal infusion rate and 5-mL patient-controlled bolus function (ON-Q* C-bloc with ONDEMAND* and Select-A-Flow*, I-Flow/Kimberly-Clark, Lake Forest, CA). B: an electronic device with programmable basal infusion rate, patient-controlled bolus, lockout duration, and maximum total infused volume (ambIT Preset, Summit Medical Products, Sandy, UT). C: An elastomeric device with a manufacturer-determined/fixed basal infusion rate without a patient-controlled bolus function (LV5 Infusor, Baxter Healthcare International, Deerfield, IL).
Due to issues with accuracy/consistency and reservoir volume, spring- and vacuum-powered models are not typically used for the purposes of continuous peripheral nerve blocks. Elastomeric pumps have been studied in depth for the pur pose of continuous regional anesthesia. The acoustic silence of this modality may be desirable to many patients to minimize sleep disturbances. With regard to accuracy, these devices will infuse 110%–130% of the set basal rate in the first 3–8 hours and repeat this high rate in the final hours before pump emptying. Some models allow for an adjustable basal rate as well as patient-controlled bolus dosing. The physics of the internal reservoir of the elastomeric devices limit ability to refill the pump, and even when technically possible, it is neither recommended by manufacturers nor approved by regulatory bodies. Electronic pumps are reported to be the most accurate and consistent over the length of an infusion, usually within 5% of the programmed basal rate. There are multiple models that are highly programmable, with various basal, patient controlled regional analgesia (PCRA) bolus, and lockout options. These pumps may emit noise during regular basal infusion and if/when an alarm is triggered. For models with an external reservoir, replacing the local anesthetic reservoir is easy to provide prolonged infusions. National pharmacologic guidelines have been developed for the preparing of regional anesthesia local anesthetic solutions. These guidelines require that the pump reservoir must be filled in an “ISO (International Organization for Standardization) class 5” environment. This entails compounding by a pharmacy using a “clean room” laminar flow workbench. Regardless of equipment type, it is important to educate patients both preoperatively and postoperatively regarding appropriate use of the pump functions. Preoperative counseling is desirable before any sedation is administered, and ideally a caretaker should be present in addition to the patient. Education should include the basic details and duration of the perineural infusion. Instructions should be given regarding when and how to use a patient-controlled bolus function. Patients are shown where the bolus button is located and how to deploy the button. They are counseled to use the bolus button whenever they have breakthrough pain and to expect a lag between bolus and local anesthetic effect. There is a risk for patients to have confusion about the roles of continuous perineural infusions and opioids as part of their multimodal analgesic plan. Patients may be instructed to use their bolus button, and if their pain is not at an acceptable level after 20 minutes, to add an oral opioid (or increase the basal infusion rate, depending on the pump capabilities). For ambulatory patients, written instructions are given with on-call contact information, as well as instructions for using the bolus button for pain, pausing the infusion in the event of an insensate extremity, or increasing/decreasing the basal rate, if necessary.
NYSORA Tips
Electronic pumps provide a more stable basal infusion rate over the course of the infusion relative to elastomeric devices.
POSTOPERATIVE MANAGEMENT AND INFUSION STRATEGIES
The local anesthetic infusion strategy may be modified to manage common postoperative issues, such as breakthrough pain or an insensate extremity. To tailor the infusion strategy to a specific patient, the overall analgesic goals must be addressed. For example, a patient having major orthopedic surgery may require steady, around-the-clock analgesia, best provided with a continuous basal infusion in addition to patient-controlled bolus doses. In contrast, a patient following surgery for burns may primarily require the benefits of a larger bolus dose for daily bedside dressing changes and very low—if any—basal infusion. Because local anesthetics are bacteriostatic or toxic, a continuous basal infusion rate is theoretically beneficial in reducing the risk of infection. Duration of local anesthetic infusion is an important postoperative consideration. While numerous infusion benefits have been demonstrated by RCT, longer duration of infusion (greater than 48 hours) has been associated with increased infection risk. However, case reports of prolonged infusions have been described (34–85 days) without identified infection.
NYSORA Tips
An adjustable basal infusion rate allows an increase in the case of inadequate analgesia and a decrease in the case of an insensate extremity.
SUMMARY
An ideal continuous regional anesthesia infusate and administration strategy should provide reliable analgesia with minimal adverse effects. At this time, long-acting local anesthetics are favored due to the desire to minimize motor block. No pharmacologic additives or adjuvants have demonstrated additional benefits. Numerous administration strategies have been described, most combining a basal infusion with a patient-controlled bolus option. Both electronic and nonelectronic pumps are capable of providing these regimens. Optimal patient use of the infusion and pump bolus function requires appropriate perioperative counseling and support. Finally, infusion duration must balance analgesic and functional benefits with the risk of infection.
Clinical updates
Johnstone et al. (Curr Opin Anaesthesiol, 2024) summarize recent strategies to optimize single-shot and continuous regional anesthesia, emphasizing standardized nomenclature, “Plan A” core block training, and international consensus on essential sonographic anatomy to improve safety and reproducibility. They report that perineural dexamethasone prolongs block duration with a plateau effect at 4 mg (8 mg IV), discuss refinement of minimum effective local anesthetic volumes, and highlight emerging technologies—such as artificial intelligence–assisted ultrasound (e.g., ScanNav) and needle-tracking systems—to enhance block accuracy and educational outcomes.
- Read more about the study HERE.
Finneran et al. (Curr Opin Anaesthesiol, 2023) review advances in ambulatory continuous peripheral nerve blocks (cPNB), highlighting that replacing basal continuous infusions with automated boluses—particularly for popliteal-sciatic catheters—reduces local anesthetic consumption while unexpectedly improving analgesia and lowering opioid use during active infusion. They also describe the use of start-delay timers after initial long-acting local anesthetic dosing to prolong the effective infusion duration and outline emerging alternatives, such as percutaneous peripheral nerve stimulation and cryoneurolysis, for extended analgesia.
- Read more about the study HERE.