Pediatric Atlas of Ultrasound and Nerve Stimulation-Guided Regional Anesthesia
Editors: Tsui, Suresh
Publisher: Springer
- The probe is positioned in a coronal oblique plane at the midpoint to medial aspect of the upper border of the clavicle.
- The pulsating subclavian artery becomes visible. (The probe may have to be moved laterally while maintaining contact with the clavicle). Doppler ultrasound can greatly assist with identification of this structure.
- The probe is adjusted to place the subclavian artery in the center of the image. The brachial plexus (trunks/divisions) can be seen in short axis as a tightly enclosed cluster (i.e., a honeycomb-like arrangement), superior and lateral to the subclavian artery.
- The image can be optimized by tilting the probe anteriorly or posteriorly.
- The scanning angle is maintained as the plexus is traced in a cephalad direction along the interscalene groove to the level of the cricoid cartilage (C6) to reveal a transverse view of the neural structures located deep to the sternocleidomastoid muscle between the anterior and middle scalene muscles (Fig. 7).
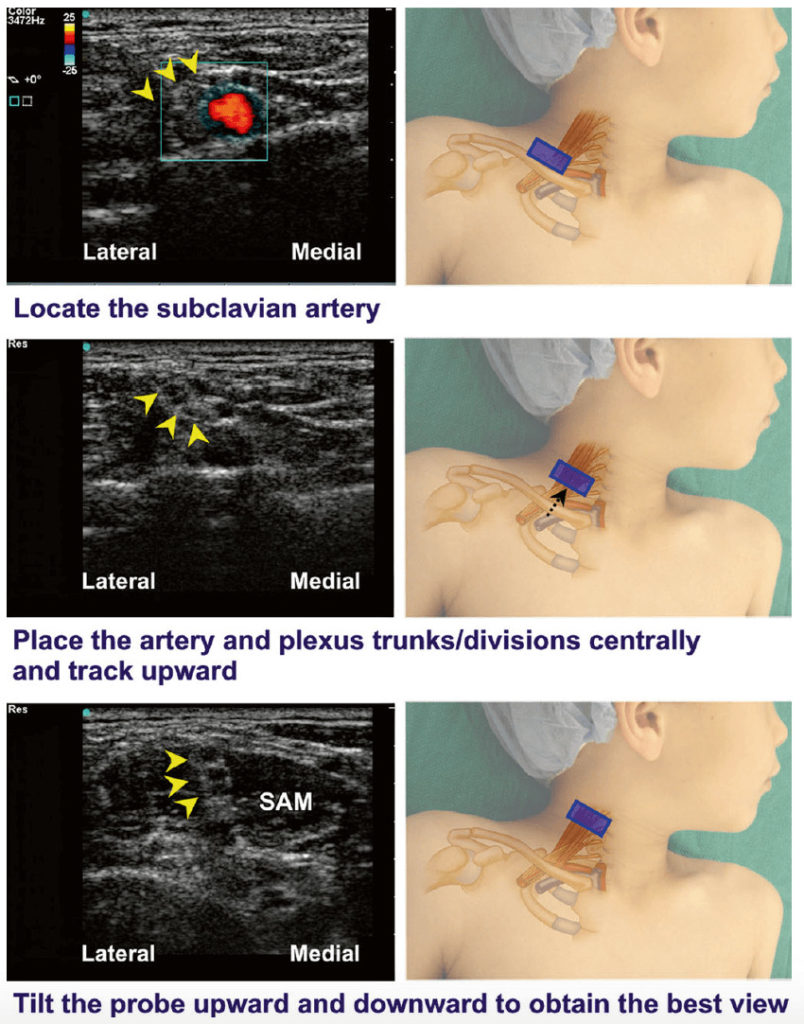
Fig. 7 Ultrasound traceback approach for interscalene block.
Pediatric Atlas of Ultrasound and Nerve Stimulation-Guided Regional Anesthesia
Enriched with NextLevel CME™ technology:
– Make notes in seconds and never lose them
– Insert your own images, infographics
– Add and watch videos inside your notes
– Attach PDFs, articles, website links
– Listen to the audio