Explore NYSORA knowledge base for free:

Chronic postsurgical pain (CPSP) is a serious yet often underestimated consequence of surgery. Affecting up to 60% of adults, depending on the type of operation, CPSP significantly impairs quality of life, functional recovery, and psychological health. In response to this pressing issue, the concept of transitional pain services (TPS) emerged in 2014. TPS is a comprehensive, multidisciplinary strategy designed to bridge acute postoperative care and long-term recovery, aiming to prevent the development of chronic pain. A recent scoping review published in Anesthesiology assessed the global implementation and effectiveness of TPS programs. It offers a detailed analysis of existing research, highlighting the promise and challenges of TPS in clinical practice. What is a transitional pain service (TPS)? TPS is a multicomponent, patient-centered perioperative program that integrates care across the surgical timeline; before, during, and after surgery. The primary objectives are: To prevent the progression from acute to chronic pain To reduce prolonged opioid use To improve postoperative recovery and psychological outcomes Core components of TPS include: Patient education and expectation setting Psychological support (e.g., cognitive behavioral therapy, mindfulness, acceptance and commitment therapy) Multimodal analgesia Opioid tapering strategies Longitudinal follow-up, often beyond hospital discharge TPS teams typically consist of anesthesiologists, pain specialists, psychologists, nurses, physiotherapists, and coordinators, ensuring a holistic approach. Key findings from the scoping review This review analyzed 15 studies involving 7,981 patients across various countries and surgical specialties. Study characteristics: 7 retrospective chart reviews 5 prospective cohort studies 1 randomized controlled trial (RCT) 2 mixed design studies Most studies focused on orthopedic, transplant, and spine surgeries Major outcomes assessed: Postoperative opioid consumption Pain intensity and interference CPSP incidence (only 1 study assessed this as a secondary outcome) What did the review reveal? 1. Evidence on CPSP prevention is very limited Only one RCT assessed CPSP directly and found no […]
Can a modified anesthesia regimen reduce neurodevelopmental risks in young children? A 2025 randomized clinical trial by Ji et al. explores whether adding dexmedetomidine and remifentanil to sevoflurane can protect brain development during surgery in infants and toddlers. Background: why neurodevelopment and anesthesia matter Preclinical animal studies show that volatile anesthetics (like sevoflurane) can cause neuronal damage and cognitive impairments when administered during critical periods of brain development. Human studies such as GAS, PANDA, and MASK found no substantial cognitive deficits from short-term anesthesia exposure, but concerns persist. Dexmedetomidine, a sedative with minimal neurotoxic effects, and remifentanil, a short-acting opioid, are proposed as safer adjuncts to reduce sevoflurane exposure. Study overview: randomized, double-blind, controlled design Population: 400 Korean children under age 2 undergoing elective, non-repetitive surgery. Intervention groups: Control group: Sevoflurane alone. DEX-R group: Low-dose sevoflurane plus dexmedetomidine and remifentanil. Primary aim: Assess neurodevelopmental outcomes at 28–30 months using: Korean Leiter International Performance Scale (nonverbal IQ) Child Behavior Checklist (CBCL) (behavioral/emotional development) Follow-up planned: Full-Scale IQ assessment at 5 years (not yet reported). Key results Sample size analyzed: 343 children (169 control, 176 DEX-R). Anesthesia duration: ~73–77 minutes, comparable between groups. Sevoflurane exposure: Significantly lower in the DEX-R group (1.8% vs. 2.6%; P < 0.001). IQ and behavior outcomes: No significant differences in: Full-scale IQ (102.5 vs. 103.6; P = 0.442) Behavioral outcomes (CBCL total score: 46.8 vs. 47.6; P = 0.469) No increase in behavioral disorders (ADHD, internalizing/externalizing problems). Conclusion: cautious optimism with balanced anesthesia The dexmedetomidine–remifentanil combination reduced anesthetic exposure but did not improve developmental outcomes at 30 months. No evidence of harm was found from a single short-duration general anesthesia session. Future results at age 5 will be crucial to determine long-term cognitive effects. Reference: Ji SH et al. Effects of Dexmedetomidine-Remifentanil on Neurodevelopment of Children after […]
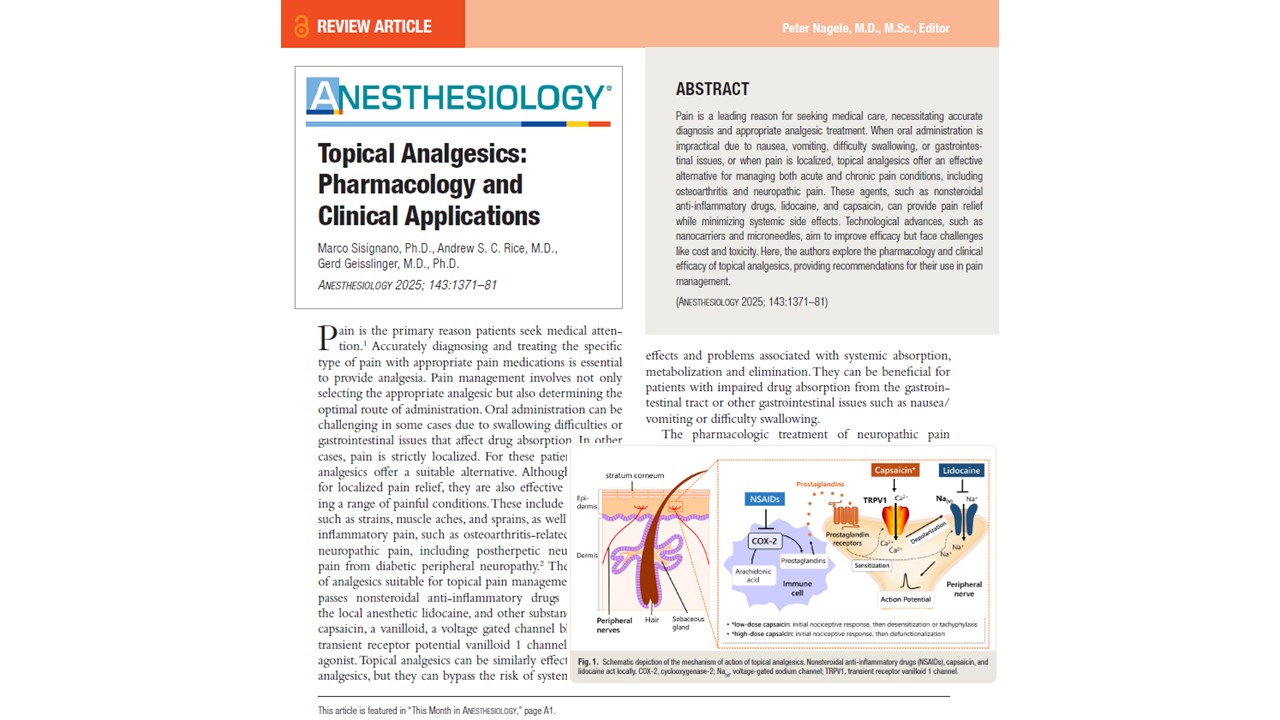
Pain remains one of the most common reasons patients seek medical care globally. As the complexity and diversity of pain presentations evolve—from acute musculoskeletal injuries to chronic inflammatory and neuropathic disorders—the need for targeted and well-tolerated pain management strategies has never been greater. While systemic analgesics, particularly oral medications, are widely used, their adverse effects and systemic absorption challenges limit their utility in certain patient populations. Topical analgesics represent a promising therapeutic alternative, as shown by Sisignano et al. 2025 in Anesthesiology. These agents deliver localized pain relief with minimal systemic involvement, offering significant benefits in conditions like osteoarthritis, diabetic peripheral neuropathy, and postherpetic neuralgia. Their ability to bypass gastrointestinal absorption and reduce systemic toxicity enhances their appeal, particularly in multimodal analgesia regimens. In this article, we examine the pharmacological basis, clinical efficacy, delivery challenges, and future directions of topical analgesics, offering anesthesiologists and pain management specialists a comprehensive overview of this crucial domain in contemporary pain care. Challenges of drug transport across the skin The skin, the body’s largest organ, poses significant barriers to drug delivery, particularly through its outermost layer, the stratum corneum. Comprising multiple layers of cornified keratinocytes (corneocytes), this structure is both lipophilic and dense, restricting drug penetration. Key absorption pathways: Intercellular route: Passage through the lipid–protein matrix. Intracellular route: Movement through corneocytes, hindered by the differing lipophilic and hydrophilic properties. Transappendageal route: Via sweat glands, sebaceous glands, and hair follicles. To overcome these barriers, modern topical formulations often incorporate chemical permeation enhancers (e.g., ethanol, dimethyl sulfoxide), colloidal carriers (e.g., liposomes, nanoemulsions), and polymeric gels that increase solubility, optimize release kinetics, and minimize skin irritation. Topical NSAIDs: mechanism and efficacy Mechanism of action Topical nonsteroidal anti-inflammatory drugs (NSAIDs) work by inhibiting cyclooxygenase-2 (COX-2) enzymes, thereby reducing local prostaglandin production and peripheral sensitization. Common agents include: Diclofenac […]