Chrystelle Sola, Christophe Dadure, Olivier Choquet, and Xavier Capdevila
INTRODUCTION
Regional anesthesia is commonly used for postoperative pain management to decrease postoperative pain and opioid consumption following head and neck surgery. Myriad techniques can be used for both acute and chronic pain management either diagnostic or therapeutic procedures. Because of the vicinity of cranial and cervical nerves to many vital structures in a compact area, the efficacy and safety of cephalic nerve blocks are based on precise and detailed knowledge of the anatomical relationships of the selected nerve, its deep and superficial courses, and the final sensory territories.
Sensory innervation of the face and neck is supplied by the trigeminal nerve (fifth cranial or V) and the C2–C4 cervical nerve roots that constitute the superficial cervical plexus (Figure 1A).
This section outlines clinically applicable regional nerve blocks of the face that for perioperative and chronic pain management. For each nerve block, practical anatomy, indications, technique, and type of complications are specifically described.
TRIGEMINAL NERVE
The fifth cranial nerve carries both sensory and motor components. The trigeminal ganglion (semilunar or Gasserian ganglion) lies in Meckel’s cave, an invagination of the dura mater near the apex of the petrous part of the temporal bone in the posterior cranial fossa. Postganglionic fibers exit the ganglion to form three nerves:
• The ophthalmic nerve (V1), a sensory nerve, divides into three branches (lacrimal, frontal, and nasociliary nerves) before entering the orbit through the superior orbital fissure. It innervates the forehead, eyebrows, upper eyelids and anterior area of the nose (Figure 1B).
• The maxillary nerve (V2), a purely sensory nerve, exits the middle cranial fossa via the foramen rotundum, passes forward and laterally through the pterygopalatine fossa, and reaches the floor of the orbit by the infraorbital foramen. It innervates the lower eyelid, the upper lip, the lateral portion of the nose and nasal septum, cheek, roof of the mouth, bone, teeth and sinus of the maxilla, and the soft and hard palates (Figure 1B).
• The mandibular nerve (V3) is a mixed sensory and motor (for the mastication muscles) nerve. After exiting the cranium through the foramen ovale, it delivers sensory branches that supply the front of the ear, the temporal area, the anterior two-thirds of the tongue and the skin, mucosa, and teeth and bone of the mandible (Figure 1B).
These sensory nerves can be blocked either at their emergence point from the cranium (V2 and V3) or, more distally and superficially, at their exit from the facial bones (V1, V2, V3) (Figure 1).
NYSORA Tips
• Neural block of the trigeminal ganglion is reserved for patients with trigeminal neuralgia who do not respond to pharmacologic therapy.
• Nerve Block of the trigeminal ganglion and its primary divisions is often used as a diagnostic test to predict response to neural block prior to proceeding with
neurolysis.
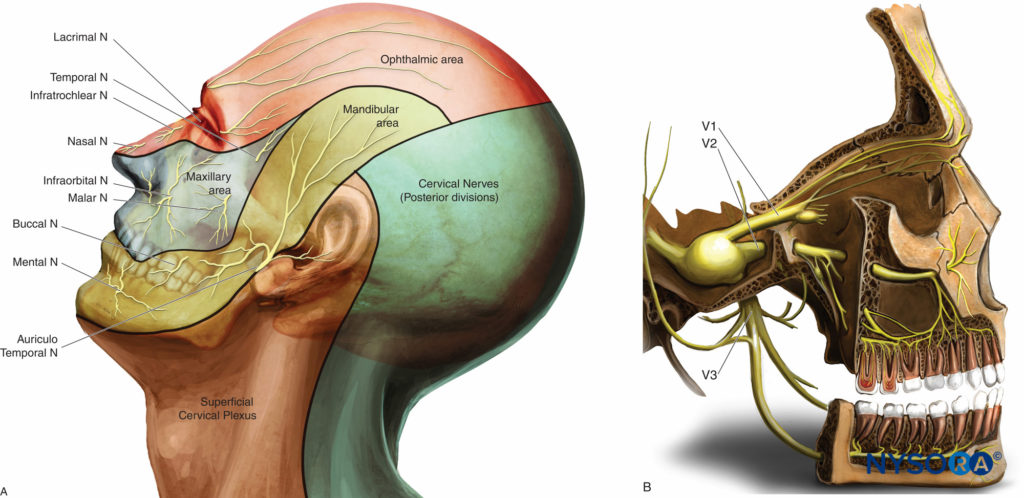
Figure 1. Innervation of the face. A: Dermatomes of the head, neck, and face. B: Distribution of the three branches of the trigeminal nerve.
The Superficial Trigeminal Nerve Blocks
For superficial trigeminal nerve blocks, the local anesthetic solution should be injected in close proximity to the three individual terminal superficial branches of the trigeminal nerve divisions: frontal nerve (of the ophthalmic nerve, V1 division); infraorbital nerve (of the maxillary nerve, V2 division); and mental nerve (sensory terminal branch of the mandibular nerve, V3 division). Each nerve is anatomically close to its respective foramen, usually located on a line drawn sagittally through the pupil (Figure 2).
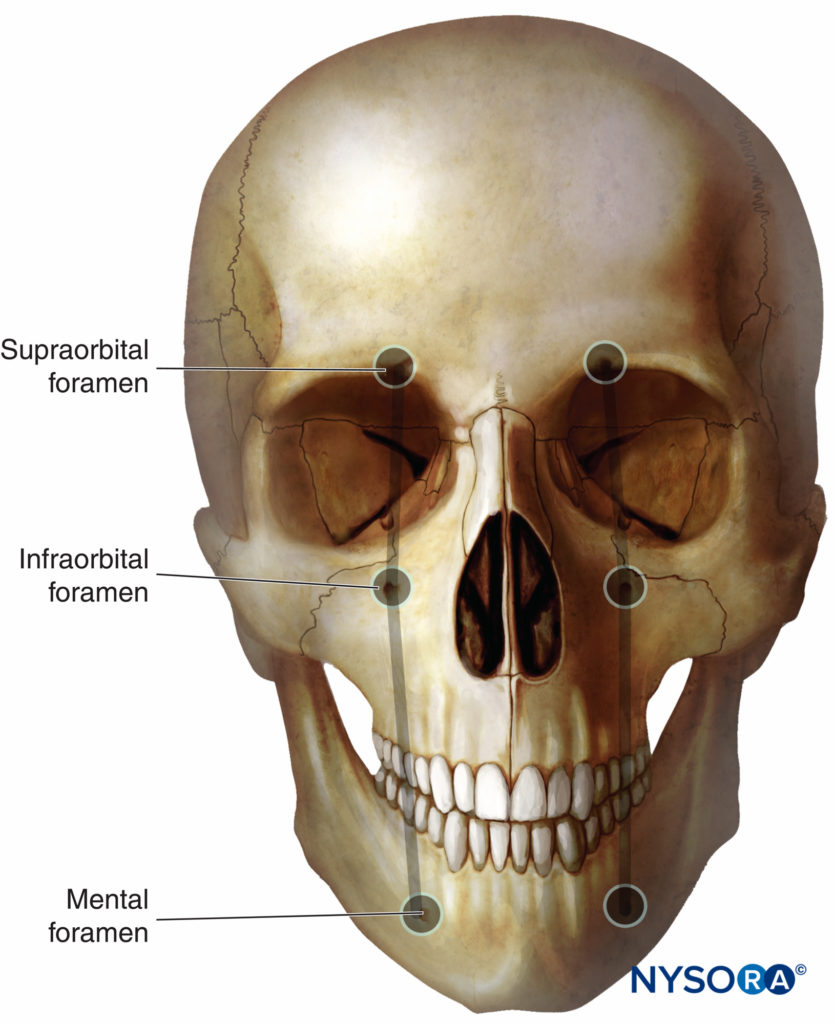
Figure 2. Terminal sensory branches of the trigeminal nerve exit the facial bone through the supraorbital, infraorbital, and mental foramen, which are at the intersection with the vertical line passing over the ipsilateral centered pupil.
Block of the Frontal Nerve (Supraorbital and Supratrochlear Branches)
Anatomy The frontal nerve enters the orbit at the superior orbital fissure and divides into the supraorbital and supratrochlear branches. The supraorbital nerve exits with its vessels through the supraorbital foramen and continues superiorly between the elevator palpebrae superioris and the periosteum. The supratrochlear nerve appears more medial through the supraorbital notch. These two branches supply the sensory innervation to the frontal scalp and forehead, the medial part of the upper eyelid, and the root of the nose (Figures 3A and 3B).
Indication The block of the frontal nerve is useful for lower forehead and upper eyelid surgery such as repair of a laceration, frontal craniotomies, frontal ventriculoperitoneal shunt placement, Ommaya reservoir placement, and plastic surgical procedures, including excision of anterior scalp pigmented nevus, benign tumor with skin grafting, or dermoid cyst excision. Frequently, surgery on one side of the forehead requires a supplemental nerve block of the contralateral supratrochlear nerve because of overlapping distributions of the nerves.
Nerve Block of branches of the ophthalmic nerve has been described for the management of acute migraine headache attacks localized to the ocular and retro-ocular region and in the treatment of pain related to acute herpes zoster.
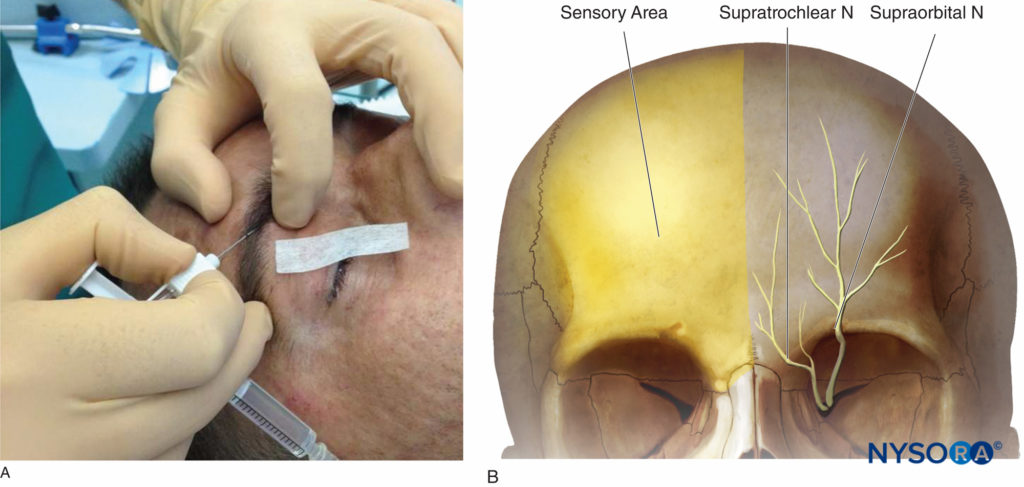
Figure 3. A: Supraorbital and supratrochlear nerve block. B: Sensory area of the supraorbital and supratrochlear nerves.
Classical Landmark Technique The supraorbital foramen can easily be palpated by following the orbit rim 2 cm from the midline in adults (intersection of the medial one-third and the lateral two-thirds). It is located approximately at the same sagittal plane as the pupil in most patients. The needle (25-gauge intradermal needle in adults, 30 gauge in children) is introduced 0.5 cm under the inferior edge of the eyebrow and is directed medially and cephalad. When the needle tip is near the supraorbital notch, after test aspiration, and with caution not to penetrate the foramen, local anesthetic solution (0.5–1 mL) can be injected, creating a subcutaneous wheal. For a supratrochlear nerve block, the landmark is at the top of the angle formed by the eyebrow and the nasal spine where the nerve is in contact with the bone. The supratrochlear nerve can be blocked immediately following supraorbital nerve block, without removing the needle, by directing the needle about 1 cm toward the midline and injecting an additional 0.5 mL of local anesthetic. After the injection, firm pressure is applied for better anesthetic spread and prevention of ecchymosis.
Complications are rarely reported during the performance of this nerve block, and may include hematoma, intravascular injection, and eye globe damage.
NYSORA Tips
The following are specific complications associated with head and neck nerve blocks:
• Subarachnoid or epidural placement of local anesthetic may lead to high spinal and brainstem anesthesia.
• Generalized seizures may occur with the injection of even small intra-arterial volumes of local anesthetic (0.5 mL or less) as the arterial blood flow continues directly from the arteries in the head and neck to the brain.
• Hematoma formation.
• Respiratory distress may result from block of the phrenic or recurrent laryngeal nerves, pneumothorax, or loss of sensory or motor function of the nerves to the airway.
Block of the Infraorbital Nerve
Anatomy The terminal branch of the maxillary nerve (V2, the second division of the trigeminal nerve) is called the infraorbital nerve when it reaches the infraorbital fossa. It exits the cranium through the infraorbital foramen in a caudad and medial direction and divides into several sensory branches: the inferior palpebral, the lateral nasal, and the superior labial nerves. The infraorbital artery and vein run parallel in close proximity to the nerve. Territories of the infraorbital nerve include the skin and mucous membrane of the upper lip and lower eyelid and the cheek between them and to the lateral side of the nose (Figures 4A and 4B).
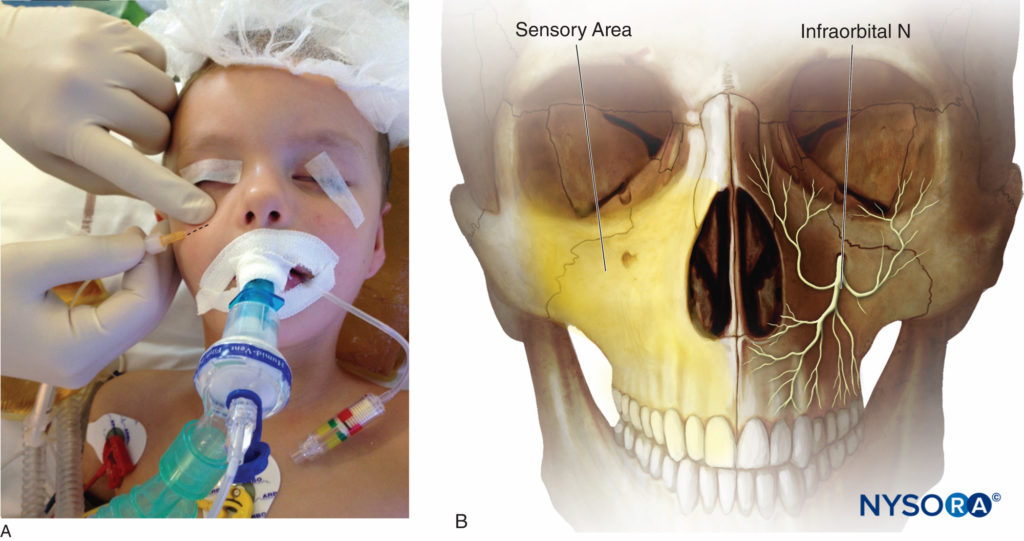
Figure 4. A: Infraorbital nerve block. B: Sensory area of the infraorbital nerve.
Indications Infraorbital nerve block is commonly used in neonates, infants, and older children undergoing cleft lip repair to provide early postoperative analgesia without the potential risk of respiratory depression that may occur when opioid analgesics are used. The other main indications are surgeries of the lower eyelid, the upper lip, the median cheek, endoscopic sinus surgery, rhinoplasty or nasal septal repair, and transsphenoidal hypophysectomy.
NYSORA Tips
• The infraorbital nerve is sensory nerve. As the nerve exits the infraorbital foramen, it supplies the skin of the lower eyelid, nose, cheek, and upper lip.
• It is accompanied by the infraorbital artery and vein.
Classical Landmark Techniques For the classical landmark techniques, two approaches can be used to perform this nerve block: the intraoral and extraoral approaches. Regardless of the chosen technique, it is necessary to prevent the penetration of the foramen to prevent damage to the eyeball. This can be done by keeping a finger on the foramen throughout the procedure.
• For the intraoral approach, the first landmark is the infraorbital foramen, which is localized just below the orbital rim, at the intersection of a vertical line drawn caudally through the center of the pupil and a horizontal line through the nasal alae. The incisor and the first premolar are then palpated. A 25- to 27-gauge needle is inserted into the buccal mucosa in the subsulcal groove at the level of the canine or the first premolar and directed upward and outward into the canine fossa. A finger is kept over the infraorbital foramen to assess the proper location of the needle tip and to avoid damage of the eyeball by accidental cephalad advancement of the needle into the orbit. Then, 1–3 mL of local anesthetic is injected after negative aspiration.
• For the extraoral approach, the infraorbital foramen is palpated (see preceding discussion). A 25- to 27-gauge needle is advanced perpendicularly with a cephalic and medial direction toward the foramen until bony resistance is appreciated. Because the axis of the infraorbital foramen is oriented caudally and medially, a lateral-to-medial approach reduces the risk of penetration of the foramen. A finger is always placed at the level of the infraorbital foramen to avoid further cephalad advancement of the needle, and gentle pressure is recommended to prevent hematoma formation.
Complications Hematoma formation, persistent paresthesia of the upper lip, prolonged numbness of the upper lip, and intravascular placement are possible. A serious (but rare) risk is penetration of the foramen, which may result in nerve damage by compression in the narrow infraorbital canal, or needle penetration of the flimsy orbital floor and damage to the orbital contents. The intraoral approach is not advised in neonates and small infants because of the proximity of the orbit.
Block of the Mental Nerve
Anatomy The mental nerve is the terminal branch of the alveolar nerve (the largest branch of the mandibular nerve, V3). It emerges at the mental foramen and divides into three branches: a descending branch to the skin of the chin and two ascending branches to the skin, labial mucosae of the lower lip, as well as the anterior teeth (Figures 5A and 5B).
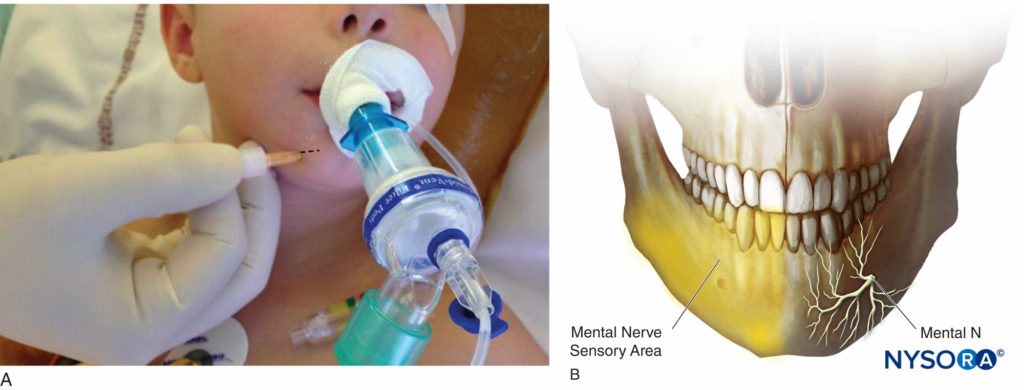
Figure 5. A: Mental nerve block. B: Sensory area of the mental nerve.
Indications Procedures involving hemangiomata, laceration repair, and other surgery involving the lower lip, skin of the chin, and the incisive and canine teeth.
Classical Landmark Technique For the classical landmark technique, the mental foramen is located in line with the pupil on the mental process of the mandible, in regard to the inferior premolar tooth. Puncture with a 25- to 27-gauge needle is performed 1 cm lateral to the foramen palpated. The needle is directed with a lateral-to-medial direction to avoid foramen penetration.
Similar to the infraorbital nerve block, an intraoral route can be utilized: The lower lip is retracted, and the needle is introduced through the mucosa in front of the first inferior premolar tooth. The needle is directed downward and outward toward the mental foramen palpated with the finger.
Complications Hematoma formation and persistent paresthesia have been reported. Less commonly, penetration of the foramen occurs, which may result in permanent nerve damage or vascular injection.
Ultrasound Guidance Technique for Superficial Trigeminal Nerve Blocks
The ultrasound-guided approach to locate the landmark foramina for superficial trigeminal nerve block is feasible. Using a high-frequency linear transducer, bone appears as a hyperechoic linear edge (white line) with an underlying anechoic (dark) shadow. At the foramina of these three nerves, disruption within the hyperechoic line indicates a discontinuity in the bone (“bone gap”). In addition, ultrasound can visualize satellite vessels close to each nerve using the color Doppler function. The real-time view of the injection spread can help avoid intravascular injection, nerve injury by the needle, or injection into the foramen.
To localize the supraorbital notch (foramen), the probe is located transversely above the orbital rim (Figure 6A).
The infraorbital foramen can be visualized by positioning the ultrasound probe horizontally or vertically in the sagittal plane. Fine translational movements from medial to lateral along the lower orbital margin are performed to highlight the disruption of the bone table (Figure 6B).
Finally, the mental foramen is localized using a transverse or sagittal plane with dynamic scanning between the upper and lower borders of the mandible (Figure 6C).
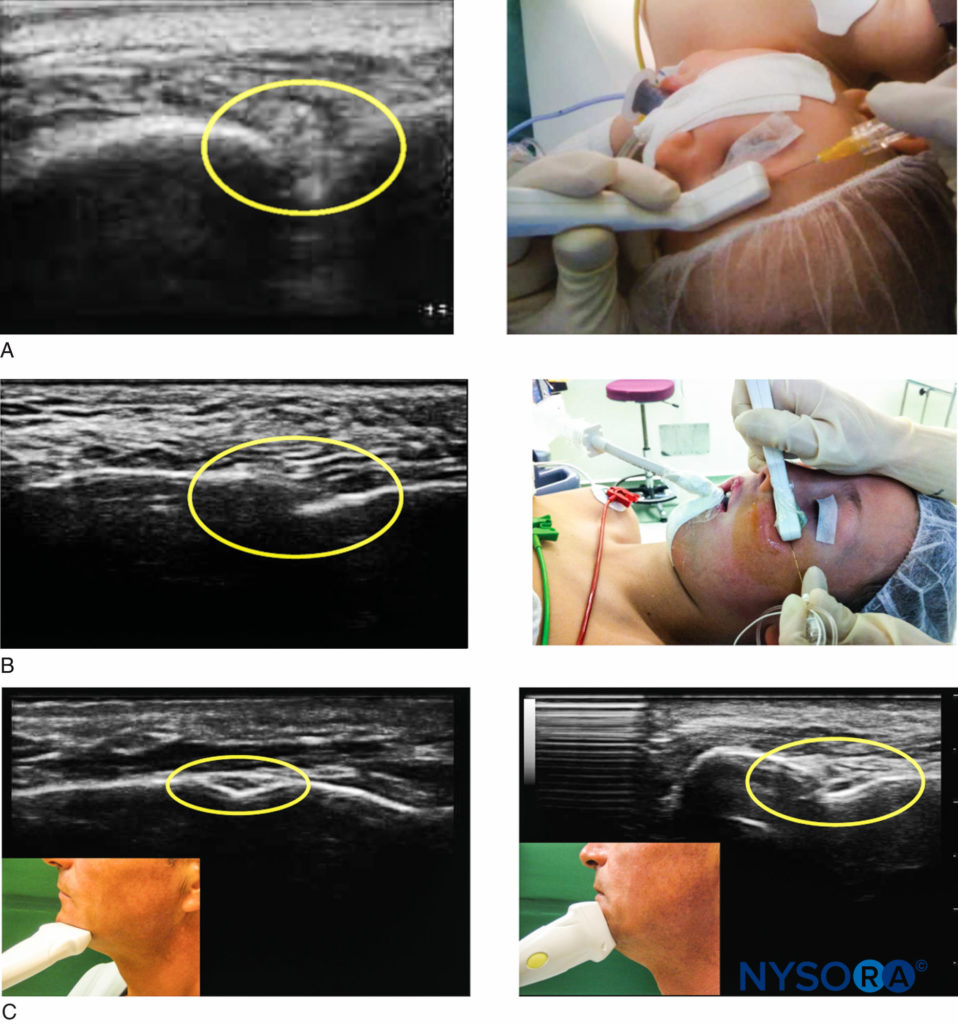
Figure 6. Ultrasound imaging for superficial trigeminal nerve block. A: The supraorbital nerve block under ultrasound guidance. B: The infraorbital nerve block under ultrasound guidance. C: The mental nerve block under ultrasound guidance.
NYSORA Tips
The following are specific complications associated with Superficial Nerves Blocks of the face:
• Facial artery vasospasm.
• Nerve injury is rare and most cases are transient and resolve completely. However, careful attention is needed to avoid injection into foramina whose consequences could lead to permanent neurological damage.
• Intravascular injection and systemic toxicity: Generalized seizures may occur with the injection of even small intraarterial volumes of local anesthetic (0.5 mL or less) as the arterial blood flow continues directly from the face arteries to the brain.
• Ecchymosis and Hematoma formation. This complication can be decreased after superficial nerves blocks techniques by using a 25- or 27- gauge needle and applying a manual pressure immediately after injection.
• Needle tract infection is very infrequent complication.
The Maxillary Nerve Block
Anatomy
The maxillary nerve exits the skull through the foramen rotundum before dividing into terminal branches (Table 1 and Figure 7). Except for the middle meningeal nerve (the intracranial branch that innervates the dura mater), all branches (zygomatic branches, superior alveolar nerve, pterygopalatine and parasympathetic branches, palatine and pharyngeal branches) arise in the pterygopalatine fossa.
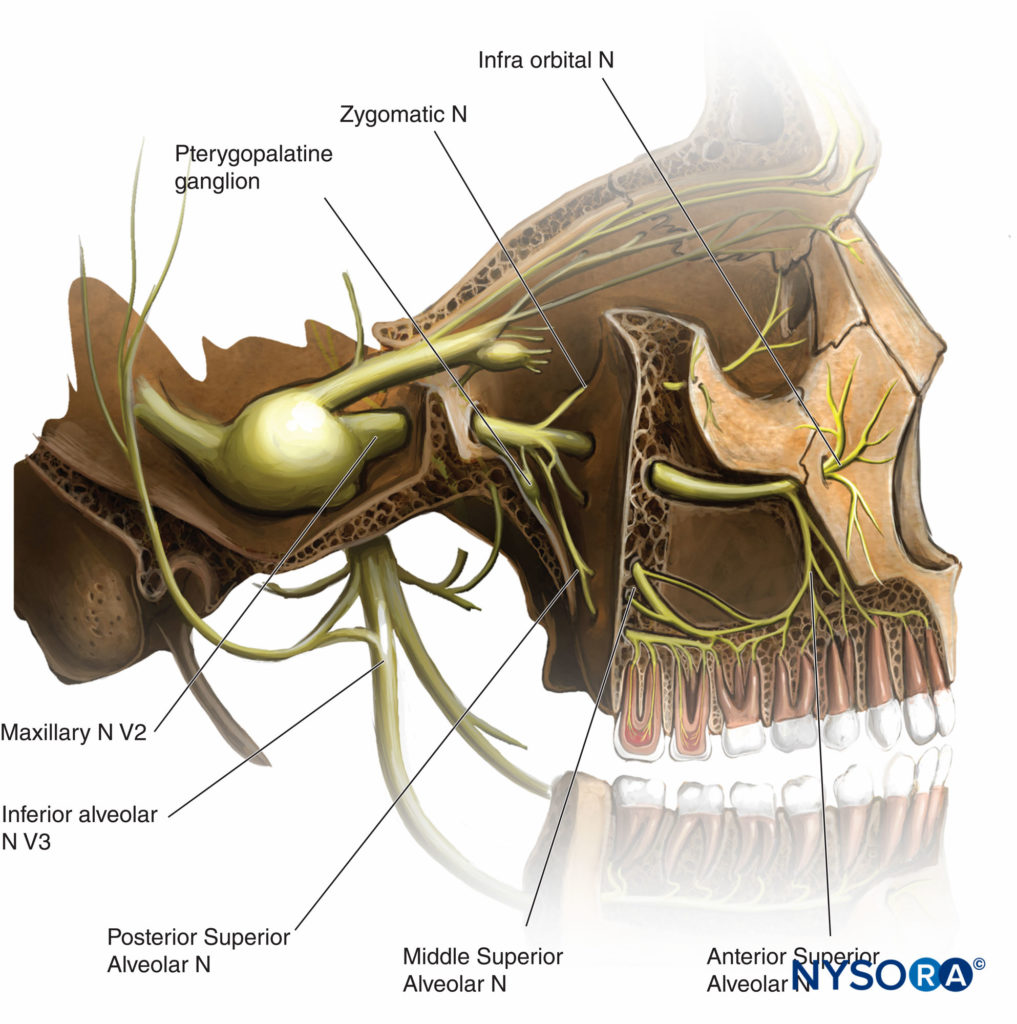
FIGURE 7. The maxillary nerve.
TABLE 1. Branches of the maxillary division.
| 1. Middle meningeal nerve |
| 2. Pterygopalatine nerve • Sensory fibers to the orbit • Nasal branches • Nasopalatine nerve • Greater palatine nerve • Lesser palatine nerve • Pharyngeal branch |
| 3. Zygomatic nerves • Zygomaticofacial • Zygomaticotemporal |
| 4. Posterior superior alveolar nerve |
| 5. Infraorbital nerve • Before exits infraorbital canal • Middle superior alveolar • Anterior superior alveolar • After exits infraorbital canal • Inferior palpebral • Lateral (external) nasal • Superior labial |
Outside the cranial vault, the maxillary nerve supplies sensory branches to
• the skin of the temple and cheek
• the nasal septum and the lateral nasal wall
• the soft and bone palates
• upper teeth and maxillary sinus
• the territory of the infraorbital nerve (previously described)
At the upper part of the pterygopalatine fossa, the maxillary nerve is accessible for a complete maxillary nerve block. The territories supplied by this complete nerve block are the following:
• superficial: lower eyelid, ala of the nose, cheek, upper lip, cutaneous zygomatic, and temporal zone
• deep: superior teeth, palatine zone, maxillary bone
Indications
This nerve block is mainly offered as an adjunct to general anesthesia for major cancer surgery of the maxilla, the ethmoidal sinus, and the pterigomaxillary or infratemporal fossa. In children, bilateral maxillary nerve blocks improve perioperative analgesia and favor the early resumption of feeding following repair of congenital cleft palate. Many other procedures may benefit from a maxillary nerve block, such as maxillary trauma (Lefort I), maxillary osteotomy, or the diagnostic and therapeutic management of trigeminal neuralgias.
Classical Landmark Technique
Many approaches to the classical landmark technique
(Figure 8) have been described.
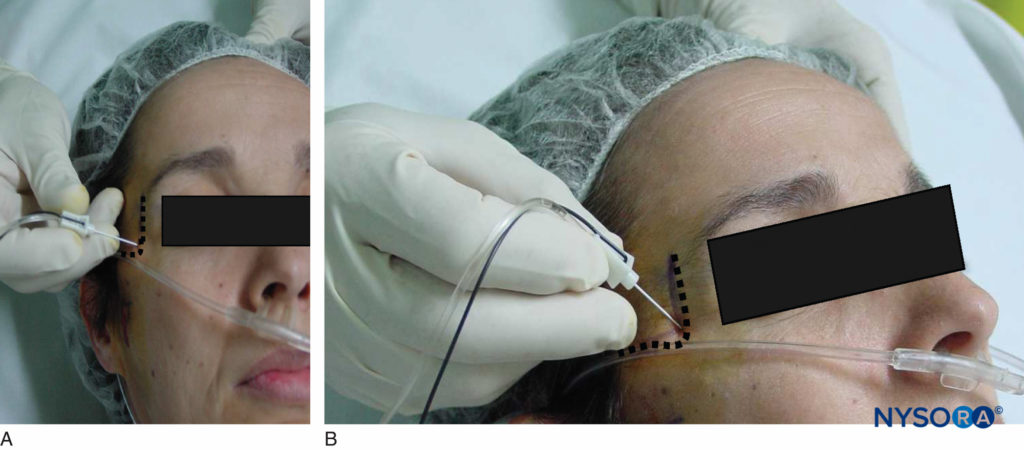
Figure 8. A and B: Suprazygomatic maxillary nerve block.
• The anterior infrazygomatic approach presents significant risks, including puncture of the maxillary artery, puncture of the posterior pharyngeal wall,
submucosal abscess, or intraorbital injection through the superior orbital fissure.
• The suprazygomatic approach seems to be the safest and is easily reproducible in either children or adult patients. The patient is placed supine with the head in a neutral position. The needle entry point is found at the angle formed by the superior edge of the zygomatic arch below and the posterior orbital rim forward. The needle (22 to 25 gauge) is inserted perpendicular to the skin and advanced to reach the greater wing of the sphenoid at a depth of approximately 10–15 mm (Figure 8A). The needle is then reoriented in a caudal and posterior direction (Figure 8B) and advanced a further 35–45 mm to reach the pterygopalatine fossa. After a negative aspiration test for blood, 0.1 mL kg-1 up to maximum of 5 mL of local anesthetic solution is slowly injected.
Nerve stimulation may help locate the pterygopalatine fossa: Nerve stimulation is associated with paresthesia coinciding with the stimulating frequency of the nerve stimulator. In anesthetized children, stimulation of the temporal muscle that results in a mandibular contraction may be noted. The disappearance of the muscle contraction heralds the passage through the temporal muscle and entrance into the pterygomaxillary fossa.
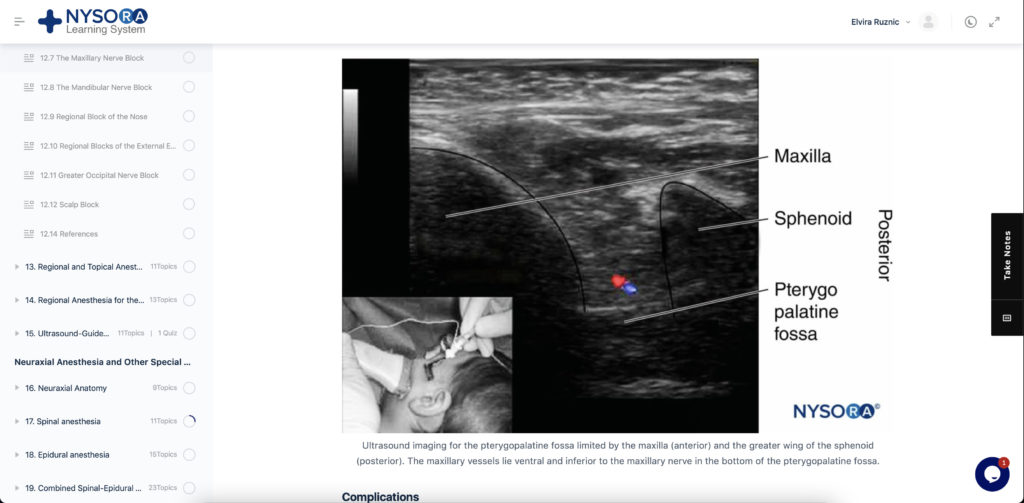
Ultrasound Guidance Technique
The (Figure 9), ultrasound transducer is placed in the infrazygomatic area, over the maxilla, with an inclination of 45° in both the frontal and the horizontal planes. The probe location allows visualization of the pterygopalatine fossa, limited anteriorly by the maxilla and posteriorly by the greater wing of the sphenoid. The needle is advanced using an out-of-plane approach. Real-time ultrasound guidance allows direct localization of the internal maxillary artery, identification of the needle tip, and spread of local anesthetic solution within the pterygopalatine fossa.
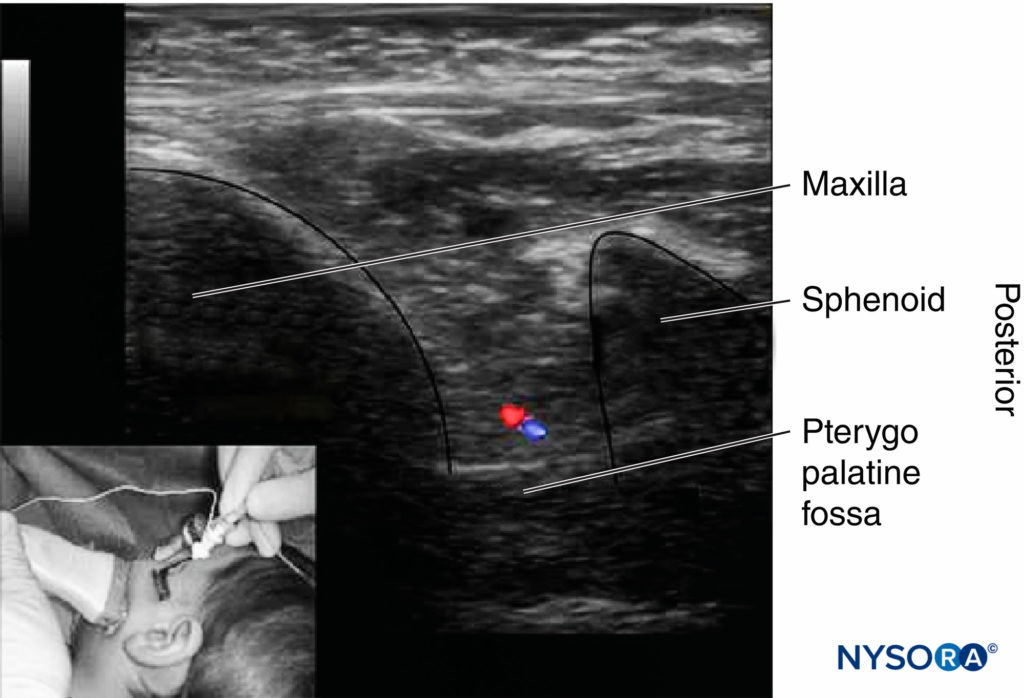
Figure 9. Ultrasound imaging for the pterygopalatine fossa limited by the maxilla (anterior) and the greater wing of the sphenoid (posterior). The maxillary vessels lie ventral and inferior to the maxillary nerve in the bottom of the pterygopalatine fossa.
Complications
Nerve Block failure can occur due to inadequate bony landmarks or inadequate needle tip position external to the pterygomaxillary fossa. Complications include cephalgia, facial paralysis, trismus, and hematoma.
The Mandibular Nerve Block
Anatomy
The mandibular nerve, the largest branch of the trigeminal nerve, exits from the cranium through the foramen ovale of the greater wing of the sphenoid. It divides into an anterior branch, which supplies motor innervation to temporalis, masseter, pterygoids, mylohyoid, tensor tympani, and palati muscles, as well as a sensory branch, the buccal nerve. The large posterior trunk divides into auriculotemporal, lingual, and inferior alveolar nerves (which reach the mental foramen, becoming the mental nerve) (Table 2 and Figure 10).
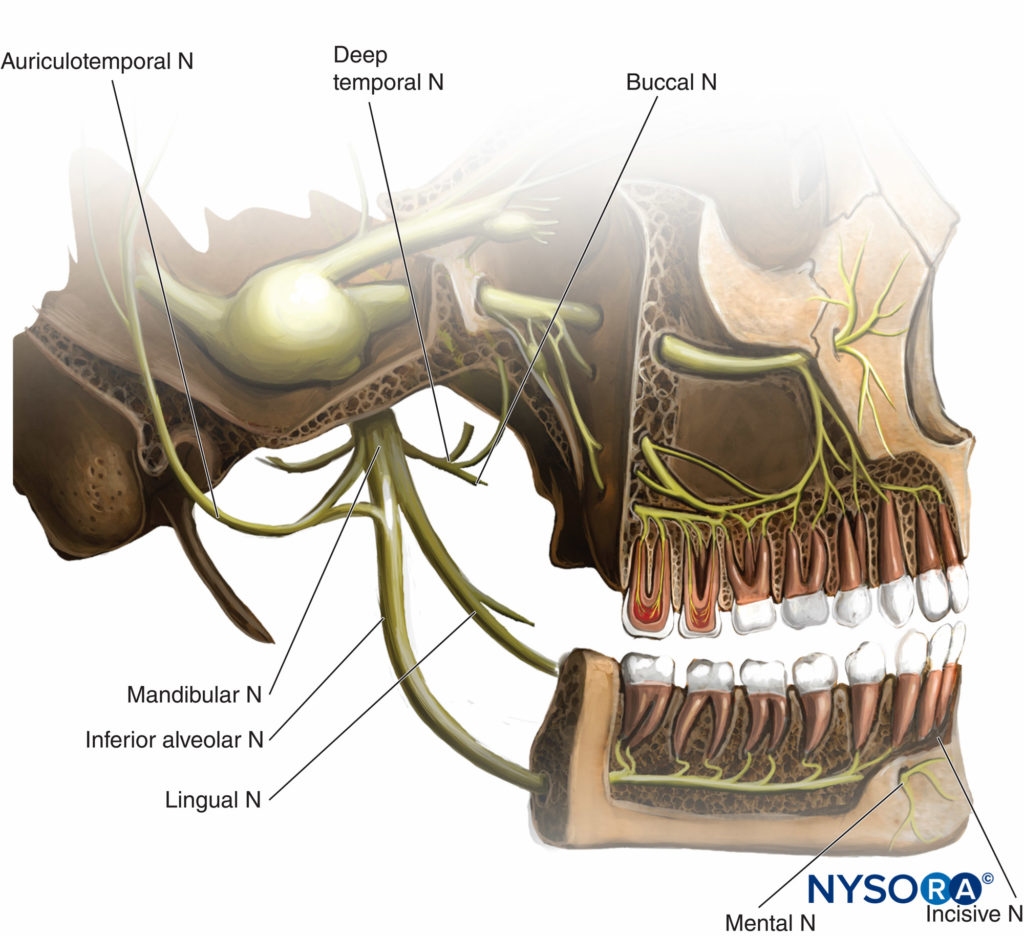
Figure 10. Mandibular nerve division and its relationship with vascular structures close.
TABLE 2. Branches of the mandibular division.
| 1. Recurrent meningeal nerve |
| 2. Motor nerves • Medial pterygoid • Masseteric • Deep temporal (2) • Lateral pterygoid |
| 3. Buccal nerve • Temporal nerve (upper) • Buccinator nerve (lower) |
| 4. Auriculotemporal nerve • Communication with facial nerve and otic ganglion (to parotid) • Articular nerve |
| 5. Lingual nerve • Via chorda tympani (VII) Taste sensations to the anterior third of tongue |
| 6. Inferior alveolar nerve • Dental • Incisive • Mental |
Mandibular nerve is blocked where the nerve emerges through the foramen ovale. Complete nerve block results in anesthesia of the ipsilateral mandibular bone, lower teeth up to the midline, buccal and lingual hard and soft tissue, anterior two-thirds of the tongue, floor of the mouth, the external acoustic meatus and auricle of the ear in its anterior zone, the skin over the jaw, the posterior part of the cheek, and the temporal area (except the area of the angle of the mandible, which is supplied by the superficial cervical plexus).
Indications
Surgery on the lower lip, the mandible skin or bone (including the lower teeth), and the anterior two-thirds of the tongue can be accomplished with this technique. This nerve block could be useful in patients with cancer or trauma. Nonmalignant chronic pain conditions such as trigeminal, vascular, or postherpetic neuralgia are also good indications for the mandibular nerve block.
Classical Landmark Technique
In the classical landmark technique, the puncture area is bound by the zygomatic arch at the top and the mandibular notch just anterior and below the tragus of the ear. The needle entry point is located between the coronoid and condylar processes of the ramus of the mandible. To avoid the risk of arterial puncture, it is recommended to insert the needle as high as possible in the space between the zygomatic arch and the center of the mandibular notch (Figure 11). After perpendicular skin penetration and advancement of 2–4 cm toward the lateral pterygoid plate, the 22- to 25-gauge needle is advanced posteriorly and inferiorly, guided by mandible elevation twitch. Depth required to contact the mandible should not be more than 5–6 cm. The minimal intensity of stimulation (around 0.5 mA) is determined, and 0.1 mL kg-1 to a maximal of 5 mL of local anesthetic solution is slowly injected after negative blood aspiration. This transcutaneous procedure with neurostimulation is associated with a high success rate.
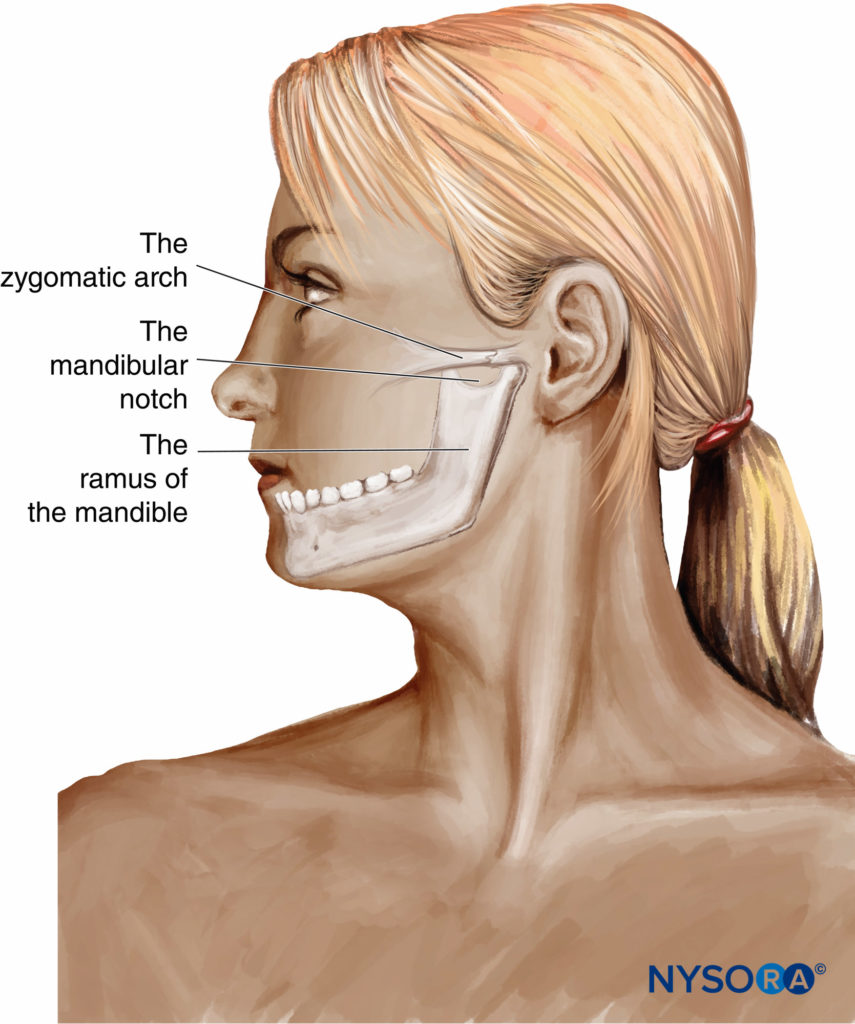
Figure 11. The mandibular nerve block: classical anatomic landmark.
Complications
The risk of puncture of the internal maxillary or middle meningeal arteries (Figure 10) can be high when the needle inserted too high in the space between the coronoid and condylar processes. After an injection of a large volume of local anesthetic solution, transient facial nerve block has been reported, which resolved spontaneously without sequelae.
Regional Nerve Block of the Nose
Anatomy
The innervation of the nose and nasal cavity is complex and involves both the ophthalmic (V1) and maxillary (V2) branches of the trigeminal nerve (Figures 12A and 12B)
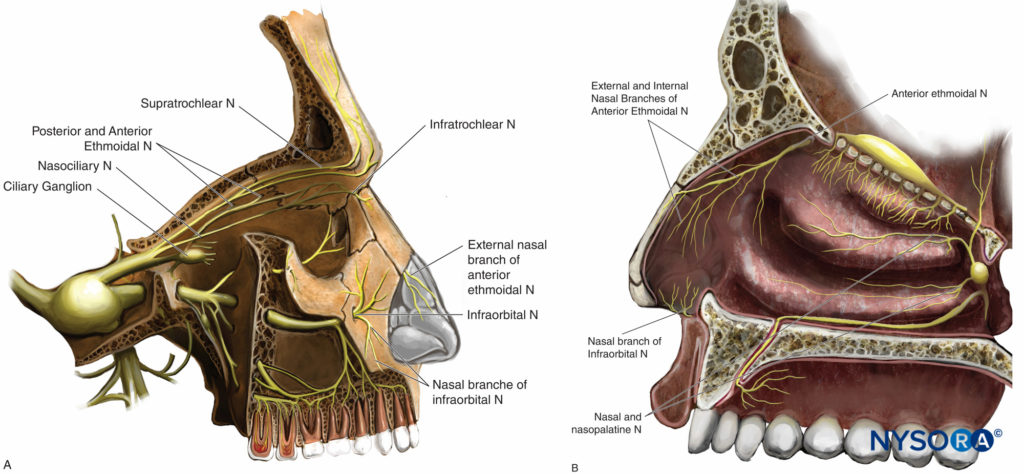
Figure 12. Innervation of the nose and nasal cavity. A: External nose. B: Septum and nasal cavity.
• The nasociliary nerve (a branch of the ophthalmic nerve, V1) gives off, within the orbital cavity, the following branches: the posterior ethmoidal nerve, long ciliary nerves, communicating branches to the ciliary ganglion, the anterior ethmoidal nerve, and the infratrochlear nerve. The ethmoidal branches supply the superior and anterior half of the nasal cavity and the sphenoidal, ethmoidal, and frontal sinuses. Internal and external nasal branches of the anterior ethmoidal nerve supply the anterior part of the septum, the lateral wall of the nasal cavity, the nasal bone, and skin to the tip of the nose.
• The supratrochlear nerve (terminal branch of the frontal nerve, V1) supplies the root of the nose.
• Nasal and nasopalatine divisions of the maxillary nerve (V2) supply the posterior aspect of the septum and nasal cavity.
• The infraorbital nerve (terminal branch of V2) supplies the wings of the nose and the mobile septum.
Indications
Bilateral nerve blocks are often required. In most cases of intranasal surgery and septoplasty, topical anesthesia or infiltration by surgeons is needed to compliment analgesia and decrease bleeding by vasoconstriction using epinephrine.
Current indications for “nasal” nerve block include rhinoplasty, polyp removal, repair of nasal fracture, and repair of nasal skin laceration.
Classical Technique
In the classical technique, the nasociliary nerve is blocked prior to its division into nasal branches of the anterior ethmoidal nerve and the infratrochlear nerve, close to the ethmoidal foramen. At this location, epinephrine-free solutions should be used to avoid the risk of retinal artery spasm. An intradermal (15–30 mm; 25–27 gauge) needle is inserted 1 cm above the medial canthus, halfway between the posterior palpebral fold and the eyebrow. It is then directed medially and backward to contact the bony roof of the orbit. At a depth of 1.5 cm, the needle should be at the anterior ethmoidal foramen; a maximum of 2 mL of local anesthetic solution is then slowly injected after a negative aspiration test. Continuous injection while removing the needle allows for block of the external nasal nerve. Compression of the interior angle of the eye by the finger promotes the diffusion of the solution to the foramen.
The infratrochlear nerve can be blocked by infiltrating at the superomedial border of the orbit and along its medial wall. The external nasal branch of the anterior ethmoidal nerve can also be blocked by infiltration at the junction of the nasal bone and the nasal cartilage.
Accompanied with an infraorbital nerve block and a pterygopalatine ganglion nerve block by topical application of local anesthetic, complete anesthesia of the nasal cavity, septum, and lateral wall of the nose appears effective.
Complications
Most reported complications are minor and transient: palpebral edema, diplopia due to paralysis of the superior obliquus muscle of the eye, ptosis, and ecchymosis at the puncture site or hematoma secondary to ethmoidal vessel puncture. Rare cases of retrobulbar hemorrhage have been described.
REGIONAL NERVE BLOCKS OF THE EXTERNAL EAR
Anatomy
The innervation of the pinna of the ear is mainly provided by the trigeminal nerve and the cervical plexus (Figures 13A and 13B).
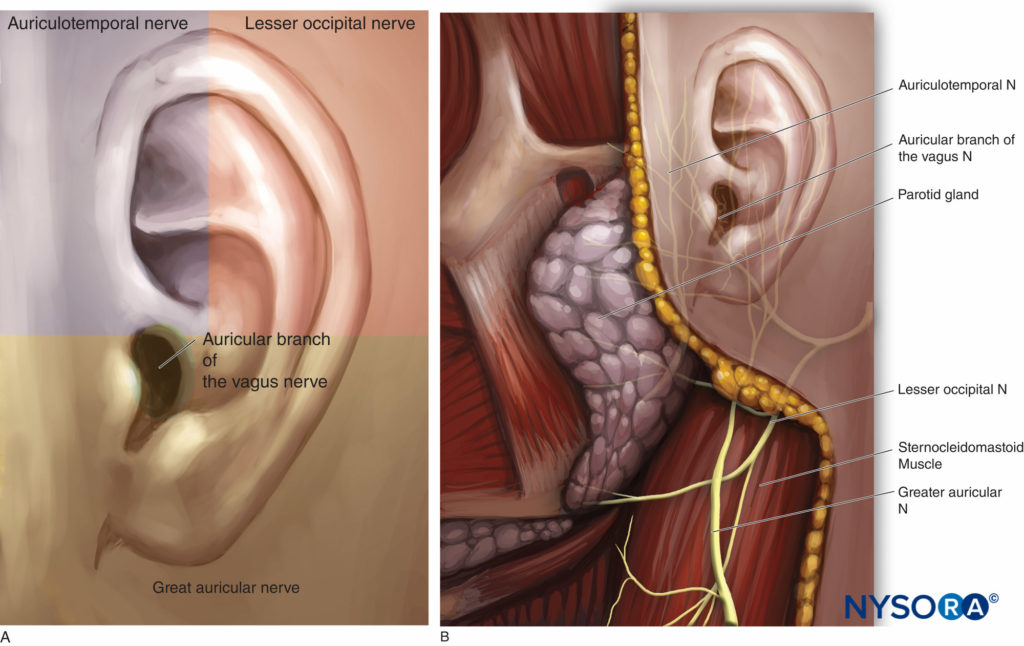
Figure 13. A and B: The innervation of the external ear.
• The superior two-thirds of the anterior surface are supplied by the auriculotemporal branch of the mandibular division of the trigeminal nerve. The auriculotemporal nerve passes through the parotid gland to ascend anterior to the auditory canal with the superficial temporal artery and passing superiorly superficial to the zygomatic arch.
• The posterior surface of the ear and the lower third of its anterior surface depend on the great auricular nerve and the lesser occipital nerve, two branches of the cervical plexus.
• The great auricular nerve arises from the second and third cervical nerve roots, emerges from the posterior border of the sternocleidomastoid muscle, and ascends (dividing into anterior and posterior branches) to the mandible, the parotid gland, and the pinna. It supplies the lower posterior aspect of the auricle, the lobule, and the skin of the angle of the mandible.
• The lesser occipital nerve arises from the ventral primary rami of the second and third cervical roots and gives innervation to the upper part of the earlobe and lateral occipital zone.
• The auricular branch of the vagus nerve (nerve of Arnold) innervates the concha and most of the posterior wall of the external auditory meatus (zona of Ramsay Hunt) as well as the inferior portion of the tympanic membrane.
Indication
This nerve block is useful for analgesia after several painful procedures such as incision and drainage of an abscess or hematoma, suture of lacerations of the ear or the skin surrounding the ear, postauricular incisions such as tympanomastoid surgery and cochlear implants, otoplasty, or surgical correction of “bat ears.”
In children having tympanomastoid surgery, greater auricular nerve block provides analgesia, with lower incidence of postoperative nausea and vomiting secondary to avoidance or reduction in the need for opioids.
Classical Techniques
For classical techniques, regional field nerve block around the auricle allows anesthesia of each nerve branch involved in external ear sensory innervation except the Ramsay Hunt area (Figure 14A).
• The auriculotemporal nerve can be blocked by injecting local anesthetic solution above the posterior portion of the zygoma, anterior to the ear and behind the superficial temporal artery. The needle (27 gauge) is inserted anterior and superior to the tragus. Caution is necessary due to the vicinity of the temporal artery.
• The greater auricular nerve and the lesser occipital nerves can be blocked distally over the mastoid process posterior to the ear. The needle is inserted behind the lower lobe of the ear and advanced following the curve of the posterior sulcus.
• Infiltration with the ring nerve block technique also provides additional efficient analgesia of the external ear (Figure 14B).
The superficial cervical plexus nerve block is anesthetizes the lesser occipital nerve and the greater auricular nerve, two of its terminal branches. This technique is described elsewhere in this volume.
Recently, a nerve block of the auricular branch of the vagus nerve has been described for pain control following myringotomy and tube placement, tympanoplasty, and paper patch for ruptured tympanic membrane. To perform this nerve block, the tragus is everted, a 30-gauge needle is inserted into the tragus, and after aspiration, 0.2 mL of local anesthetic solution is injected (Figure 14C).
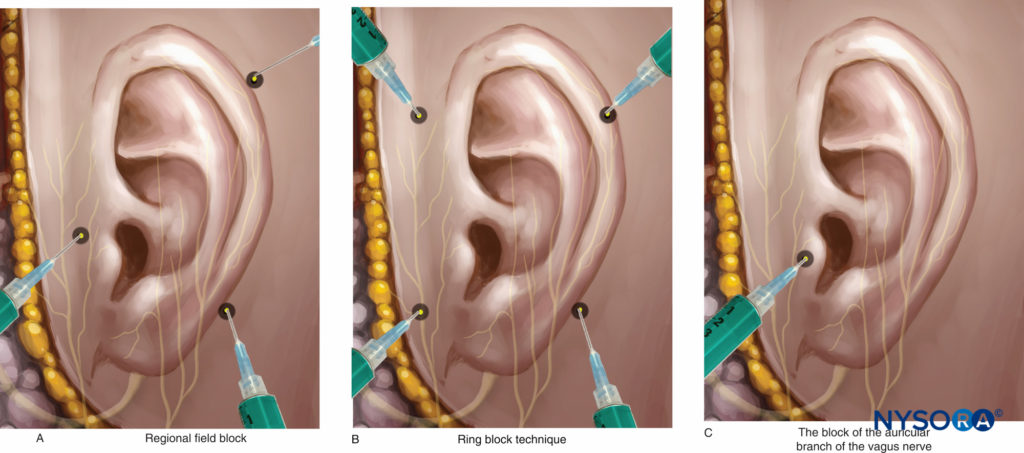
Figure 14. External ear nerve block techniques. A: Regional field nerve block. B: Ring nerve block technique. C: Auricular nerve block.
Complications
Intravascular injections, hematoma, deep cervical nerve block, potential phrenic nerve block, and transient inability to shrug the shoulder are potential adverse effects of the superficial plexus cervical approach behind the sternocleidomastoid muscle.
Bleeding from the needle entry site is rare, and intravascular injection should be avoided by careful aspiration.
HEAD NERVE BLOCKS
Greater Occipital Nerve Block
Anatomy
The greater occipital nerve (GON) arises from the second cervical nerve root that emerges between the atlas and the axis. It ascends between the obliquus capitis inferior and semispinalis capitis before piercing the latter muscle. It then becomes subcutaneous by piercing the trapezius aponeurosis, slightly inferior to the superior nuchal line. At this point, the GON is most often located immediately medial to the occipital artery.
The GON provides cutaneous innervation to the major portion of the posterior scalp from the level of the external occipital protuberance to the vertex.
Indications
This nerve block is useful for pain relief after posterior craniotomies, revision or insertion of a ventriculoperitoneal shunt, as well as for diagnosis and pain treatment secondary to various headache syndromes, such as primary headache, cervicogenic headache, migraine, occipital neuralgia, and tension headache.
Classical Landmark Technique
The GON is located at approximately two-thirds the distance on a line drawn from the center of the mastoid to the external occipital protuberance along the superior nuchal line, where it lies medial to the occipital artery. The pulsation of the occipital artery is easy to palpate. Palpation in this area may elicit a paresthesia or uncomfortable feeling in the distribution of the nerve. A 25- or 27-gauge needle can be used depending on the size of the patient.
The needle is directed at 90° toward the occiput; after aspiration, 1–3 mL of local anesthetic is injected. When the needle is withdrawn, pressure should be maintained over the site of injection to promote soaking the nerve with local anesthetic and to achieve hemostasis. Numbness over the top of the head is a sign of a successful nerve block.
There is considerable interpatient variability in the nerve location, with high variability (1.5–7.5 cm) of the distance of the GON to the midline at a horizontal level between the external occipital protuberance and the mastoid process. More recently, ultrasound guidance has been described to perform this nerve block.
Ultrasound Guidance Technique
In classical distal nerve block technique, at the level of the superior nuchal line, the ultrasound probe was initially placed in a transverse plane with the center of the probe lateral to the external occipital protuberance (Figure 15, area 1).
A more proximal approach at the level of the second cervical vertebra (C2), was developed by Greher and al. At this new site, the GON lies superficial to the obliquus capitis inferior muscle; the relationship of the GON to this muscle appears constant and reliable. The ultrasound transducer is moved down over the atlas (C1) to the location of the spinous process of C2 (that is always bifid). The probe is then moved laterally to identify the obliquus capitis inferior muscle of the neck (Figure 15, area 2). The GON can be easily visualized at this level, crossing the obliquus capitis inferior muscle from caudal to rostral and lateral to medial (Figure 16).
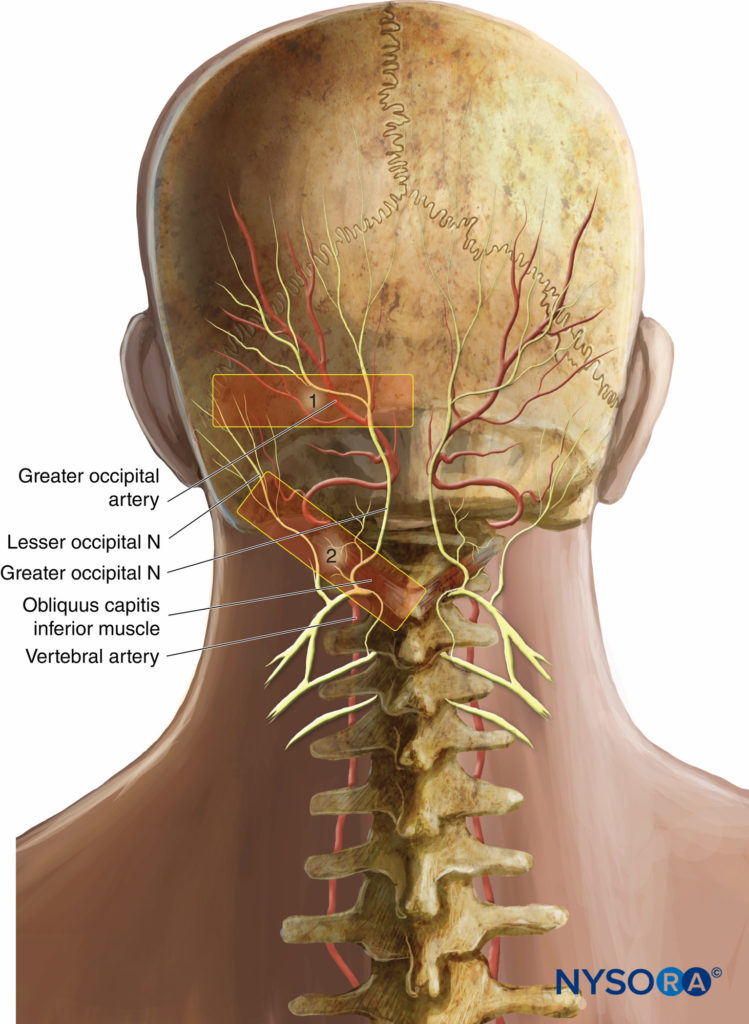
Figure 15 Transducer positions for ultrasound-guided nerve blocks of the GON. 1, Classic nerve block site at the superior nuchal line; 2, new nerve block site at C2, over the obliquus capitis inferior muscle.
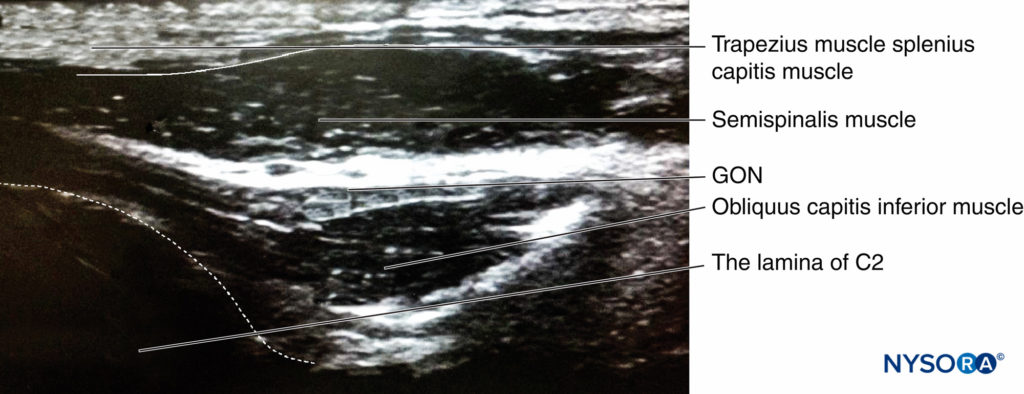
Figure 16. Sonogram of greater occipital nerve. The probe is placed along the long axis of the obliquus capitis inferior muscle (Figure 15, 2).
Complications
There are relatively few complications because of the superficial location of the nerve. Intravascular injection is always possible and prevented by performing careful aspiration prior to injection. Caution needs to be taken because the vertebral artery and the spinal cord are close proximity to the GON. The vertebral artery is lateral to the GON deep to the obliquus capitis inferior muscle and the lamina of the atlas, while the spinal cord is medial and again deep to the muscle.
Scalp Nerve Block
Anatomy
The “scalp nerve block” is classically described with potential block of seven nerves, including branches from cervical spinal rami and from the trigeminal division (Figure 17).
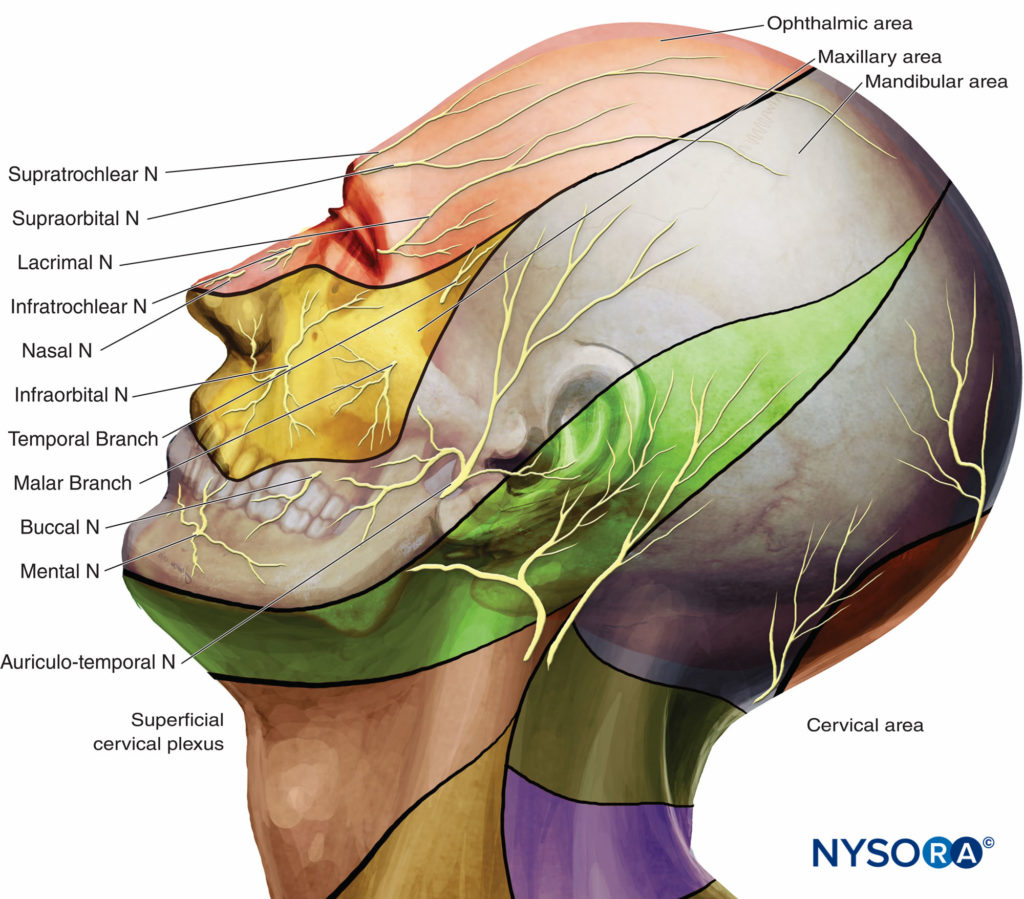
Figure 17. Innervation of the scalp.
• Greater occipital, lesser occipital, and great auricular nerves originate from the ventral and the dorsal rami of C2 and C3 spinal nerves. The GON travels up to the vertex, and the lesser occipital nerve innervates skin behind the ear.
• The ophthalmic division of the trigeminal nerve gives off, via the frontal nerve, supraorbital and supratrochlear nerves, which innervate the skin from the forehead to the lamboidal suture.
• The zygomaticotemporal nerve is one of the two branches of the zygomatic nerve that arise from the maxillary division of the trigeminal nerve. It innervates a small area of the forehead and temporal area.
• The auriculotemporal nerve arises from the mandibular division of the trigeminal nerve. It innervates the posterior portion of the skin of the temple.
Indication
Scalp nerve blocks are used in adults and children for a variety of head and neck procedures as well as in neurosurgery or in diagnostic and therapeutic management of chronic pain (eg, headache disorders of muscular and nervous etiology).
Common reasons for providing anesthesia to the scalp are repair of a laceration, foreign body removal, or exploration of scalp wounds and drainage of abscesses or subdural hematomas.
In neurosurgery, adverse hemodynamic reactions can occur during a craniotomy due to algogenic or reflexogenic events (insertion of the cranial pins of the Mayfield head holder, incision of the scalp, craniotomy, and dural incision). These reactions can be modulated by local or regional anesthesia, with the additional benefit of postoperative analgesia.
Local anesthesia for scalp blockad is essential in intraoperative anesthetic management of patients undergoing awake craniotomy Local scalp nerve blocks are particularly useful when the patient’s cooperation is needed for functional testing during the neurosurgical procedure, such as during epilepsy surgery and deep brain stimulation for Parkinson’s disease, resections of lesions located close to or within functionally essential motor, cognitive, or sensory cortical areas.
Infiltrational Anesthesia
All the nerves involved in the sensitivity of the scalp become superficial and accessible to anesthetic. To nerve block the entire scalp, a circumferential infiltration of local anesthetic solution (with 1:200,000 epinephrine) above an imaginary line drawn from the occipital protuberance to the eyebrows, passing along the upper border of the ear, is necessary. Approximately 30 mL are required to perform this ring nerve block around the scalp.
“Regional Nerve Blocks” Technique
For the “regional nerve blocks” technique, the supraorbital and supratrochlear nerves are blocked with an intradermic needle as they emerge from the orbit.
• The auriculotemporal nerves are blocked 1.5 cm anterior to the ear at the level of the tragus (see the section on regional nerve blocks of the external ear).
• The postauricular branches of the greater auricular nerves are blocked 1.5 cm posterior to the ear at the level of the tragus (see the section on regional nerve blocks of the external ear).
• Great and lesser occipital nerves are blocked by infiltrating along the superior nuchal line, approximately halfway between the occipital protuberance and the mastoid process (see the section on GON nerve block).
Complications
The most common complication associated with scalp anesthesia is hematoma formation at the site of injection. Careful aspiration is suggested to avoid a potentially intravascular injection; because of the high vascularity of the scalp, the use of a diluted anesthetic solution with 1:100,000 or 1:200,000 epinephrine is usually considered safe to prevent toxic plasma drug levels.
CONCLUSION
A number of nerve block procedures can be used for surgical procedures performed on the face and scalp. The entire face area can be anesthetized using five simple nerve blocks, providing adequate anesthesia for skin procedures as well as perioperative pain management of orthopedic, craniofacial, and cancer surgery.
This text is a sample of content from the Compendium of Regional Anesthesia on the NYSORA LMS.
NYSORA’s Compendium of Regional Anesthesia is simply the most comprehensive, and practical curriculum on Regional Anesthesia from A to Z, featuring NYSORA’s Premium content. As opposed to textbooks and e-books, the Compendium is continuously updated and features NYSORA’s newest videos, animations, and visual content.
The Compendium is one of several gold-standard educational courses on NYSORA’s Learning System (the NYSORA LMS), and registration to NYSORALMS.com is free. The FULL access to the Compendium, however, is based on an annual subscription, as it requires an army of illustrators, video editors, and an educational team to continue making it the BEST tool for education on everything regional anesthesia. While you can think of the compendium as an ebook on steroids, a quick test drive will give you a real-time feel of how incredible the Compendium really is. Your subscription will transform the way you read about regional anesthesia:
- Learn visually: Everything regional, including spinal, epidural, and nerve block procedures and management protocols
- Review step-by-step techniques instructions for over 60 nerve blocks
- Access NYSORA’s fabled illustrations, animations, and videos (such as Reverse Ultrasound Anatomy)
- Access RA info on any device via the desktop platform and mobile app
- Get real-time updates
- Review infographics for exam preparation (e.g. EDRA)
- Use the Community feed with real case discussions, images and videos are posted and discussed by subscribers and world’s top experts alike.
Even if you do not wish to subscribe to the Compendium, do register to the NYSORA LMS, be the first to know what’s new in regional anesthesia, and get involved in case discussions.
Here’s what the activity feed on NYSORA LMS looks like:
We are convinced that once you experience the Compendium on the NYSORA LMS, and you’ll never go back to your old books, and your subscription will support keeping NYSORA.com free for the rest of the world.
Additional Reading
- Suresh S, Bellig G: Regional anesthesia in a very low-birth-weight neonate for a neurosurgical procedure. Reg Anesth Pain Med 2004;29:58–59.
- Suresh S, Wagner AM: Scalp excisions: getting “ahead” of pain. Pediatr Dermatol 2001;18:74–76.
- Dimitriou V, Iatrou C, Malefaki A, Pratsas C, Simopoulos C, Voyagis GS: block of branches of the ophthalmic nerve in the management of acute attack of migraine. Middle East J Anesthesiol 2002;16:499–504.
- Gain P, Thuret G, Chiquet C, et al: Facial anesthetic nerve blocks in the treatment of acute pain during ophthalmic zoster. J Fr Ophtalmol 2003; 26:7–14.
- Bosenberg AT: Nerve Blocks of the face and neck. Tech Reg Anesth Pain Manag 1999;3:196–203.
- Bosenberg AT, Kimble FW: Infraorbital nerve block in neonates for cleft lip repair: Anatomical study and clinical application. Br J Anaesth 1995; 74:506–508.
- Prabhu KP, Wig J, Grewal S: Bilateral infraorbital nerve block is superior to peri-incisional infiltration for analgesia after repair of cleft lip. Scand J Plast Reconstr Surg Hand Surg 1999;33:83–87.
- Higashizawa T, Koga Y: Effect of infraorbital nerve block under general anesthesia on consumption of isoflurane and postoperative pain in endoscopic endonasal maxillary sinus surgery. J Anesth 2001;15: 136–138.
- McAdam D, Muro K, Suresh S: The use of infraorbital nerve block for postoperative pain control after transsphenoidal hypophysectomy. Reg Anesth Pain Med 2005;30:572–573.
- Tsui BC: Ultrasound imaging to localize foramina for superficial trigeminal nerve block. Can J Anaesth 2009;56:704–706.
- Mesnil M, Dadure C, Captier G, et al: A new approach for peri-operative analgesia of cleft palate repair in infants: the bilateral suprazygomatic maxillary nerve block. Paediatr Anaesth 2010;20:343–349.
- Han KR, Kim C, Chae YJ, Kim DW: Efficacy and safety of high concentration lidocaine for trigeminal nerve block in patients with trigeminal neuralgia. Int J Clin Pract 2008;62:248–254.
- Sola C, Raux O, Savath L, Macq C, Capdevila X, Dadure C: Ultrasound guidance characteristics and efficiency of suprazygomatic maxillary nerve blocks in infants: A descriptive prospective study. Paediatr Anaesth 2012; 22:841–846.
- Giles WC, Iverson KC, King JD, Hill FC, Woody EA, Bouknight AL: Incision and drainage followed by mattress suture repair of auricular hematoma. Laryngoscope 2007;117:2097–2099.
- Brown DJ, Jaffe JE, Henson JK: Advanced laceration management. Emerg Med Clin North Am 2007;25:83–99.
- Suresh S, Barcelona SL, Young NM, Seligman I, Heffner CL, Cote CJ: Postoperative pain relief in children undergoing tympanomastoid surgery: Is a regional nerve block better than opioids? Anesth Analg 2002;94:859–862, table of contents.
- Cregg N, Conway F, Casey W: Analgesia after otoplasty: Regional nerve block vs local anaesthetic infiltration of the ear. Can J Anaesth 1996; 43:141–147.
- Suresh S, Voronov P: Head and neck blocks in infants, children, and adolescents. Paediatr Anaesth 2012;22:81–87.
- Loukas M, El-Sedfy A, Tubbs RS, et al: Identification of greater occipital nerve landmarks for the treatment of occipital neuralgia. Folia Morphol (Warsz) 2006;65:337–342.
- Greher M, Moriggl B, Curatolo M, Kirchmair L, Eichenberger U: Sonographic visualization and ultrasound-guided block of the greater occipital nerve: A comparison of two selective techniques confirmed by anatomical dissection. Br J Anaesth 2010;104:637–642.
- Pinosky ML, Fishman RL, Reeves ST, et al: The effect of bupivacaine skull nerve block on the hemodynamic response to craniotomy. Anesth Analg 1996;83:1256–1261.
- Nguyen A, Girard F, Boudreault D, et al: Scalp nerve blocks decrease the severity of pain after craniotomy. Anesth Analg 2001;93:1272–1276.
- Bilotta F, Rosa G: “Anesthesia” for awake neurosurgery. Curr Opin Anaesthesiol 2009;22:560–565.
- Sinha PK, Koshy T, Gayatri P, Smitha V, Abraham M, Rathod RC: Anesthesia for awake craniotomy: A retrospective study. Neurol India 2007;55:376–381.






