To investigate the possible role of a common continuous epineural sheath [1], we examined the popliteal fossa in lower legs of cadavers for the existence and continuity of a tissue sheath surrounding the sciatic nerve and its two main divisions.
Based on: “Vloka JD, Hadzic A, Lesser JB, Kitain E, Geatz H, April EW, Thys DM. A Common Epineural Sheath for the Nerves in the Popliteal Fossa and Its Possible Implications for Sciatic Nerve Block. Anesth Analg 1997;84:387-90.”
|
Introduction An unusually quick onset of dense anesthesia is occasionally observed after the sciatic nerve block in the popliteal fossa is performed. However, anesthesia is frequently profound in the distribution of both divisions of the nerve, although the response to nerve stimulation or paresthesia is obtained only in the distribution of either the tibial nerve or common peroneal nerve. To investigate the possible role of a common continuous epineural sheath [1], we examined the popliteal fossa in lower legs of cadavers for the existence and continuity of a tissue sheath surrounding the sciatic nerve and its two main divisions. Anatomy of the Sciatic Nerve 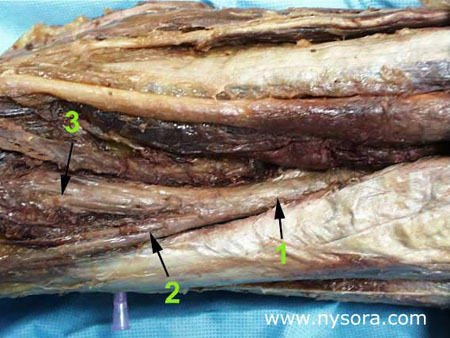 Figure 1
The sciatic nerve (1) is formed from spinal cord segments L4-S2 (and occasionally S3) and consists of two distinct nerves, the tibial nerve (3) and common peroneal nerve (2), which share a common epineural sheath from their origin to the popliteal fossa [2,3], where then divides into the tibial nerve and common peroneal nerve (Figure 1).The tibial nerve is the larger of the two branches and runs parallel and slightly lateral to the midline. Inferiorly, it passes between the heads of the gastrocnemius muscle. The common peroneal nerve follows the tendon of the biceps femoris muscle laterally and travels around the fibular head as it leaves the popliteal fossa. The two nerves innervate the entire leg below the knee except for the antero-medial leg and foot which are innervated by the saphenous nerve (L2-L4). Histology of Peripheral Nerves 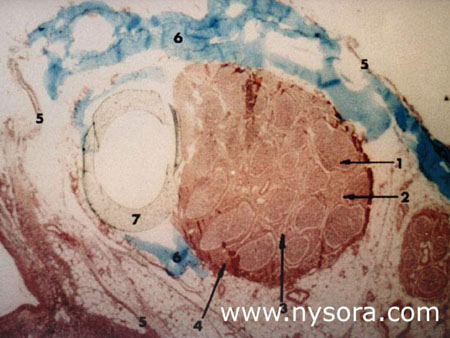 Figure 2. Microscopic view of the cross-section of the tibial nerve at 10 cm below the popliteal crease. 1. Endoneurium 2. Perineurium 3. Intrafascicular epineurium 4. Epifascicular epineurium 5. Epineural tissue (adventitia of the nerve) 6 Injected solution of blue vinyl acetate (BVA) within the epineural tissue 7. Teflon catheter inserted into the epineural adventitia, next to the tibial nerve
The sciatic nerve is formed from spinal cord segments L4-S2 (and occasionally S3) and consists of two distinct nerves, the tibial nerve and common peroneal nerve, which share a common epineural sheath from their origin to the popliteal fossa [2,3], where then divides into the tibial nerve and common peroneal nerve (Figure 1).The tibial nerve is the larger of the two branches and runs parallel and slightly lateral to the midline. Inferiorly, it passes between the heads of the gastrocnemius muscle. The common peroneal nerve follows the tendon of the biceps femoris muscle laterally and travels around the fibular head as it leaves the popliteal fossa. The two nerves innervate the entire leg below the knee except for the antero-medial leg and foot which are innervated by the saphenous nerve (L2-L4).  Figure 3
This study was performed on 10 adult cadaver legs free of obvious pathology of their lower extremities. The cadavers had been dead from 6 to 18 months. They were embalmed for anatomical purposes using a solution of phenol (13%) as the principal fixative, and glycerin (28%) for retention of water content. The cadavers were positioned prone on the dissecting table, so that the long axis of the legs were horizontal to the table plane, and the feet formed a 90° angle to the horizontal plane (Figure 3). The calf was dissected 10 cm below the popliteal crease and the tibial nerve was exposed in the deep posterior compartment under the soleus muscle . The fascial sheath surrounding the nerve was identified and a 16-gauge catheter was inserted into the sheath 15 cm below the popliteal crease (Figure 4 ). The catheter was advanced until the tip was positioned at a distance of 10 cm distal to the popliteal crease. 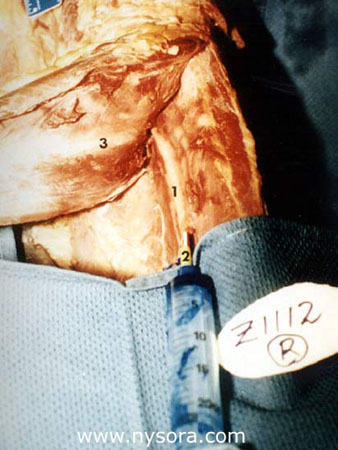 Figure 4 Sheath of the tibial nerve 16-gauge catheter inserted into the nerve sheath Distal part of the soleus muscle dissected 10 cm below popliteal fossa crease
Using the method of sealed envelopes, each leg was randomly assigned to one of the two groups. In group A (n=5), 15 mL of Blue Vinyl Acetate (BVA) solution (Cabisco®, Carolina Biological Supply Company) was injected into the tibial nerve sheath. In group B (n=5), 30 mL of BVA was injected into the tibial nerve sheath (Figure 4 ). Upon injection of the dye the catheters were left in place. One hour later, the dissection was extended into the popliteal fossa and the spread of BVA within the sheath investing the nerves in the fossa was observed (Figure 5). The level of the division of the sciatic nerve into tibial nerve and common peroneal nerve was also determined in each leg.  Figure 5. Posterior aspect of the popliteal fossa. 1. Blue vinyl acetate within the epineural sheath 2. Common epineural sheath covering popliteal nerve 3. Tibial nerve 4. Common peroneal nerve 5. Biceps femoris muscle 6. Semitendinosus muscle 7. Semimembranosus muscle
Tissue samples of tibial nerve, common peroneal nerve and sciatic nerves were excised, embedded in paraffin, cross sectioned and stained with hematoxylin and eosin, or trichrome stains. The samples were examined for anatomical placement of the catheter and distribution of the BVA in relation to the nerves. The difference in extent of the spread of the BVA within the epineural sheaths and external measurements between the two groups was tested using a one sided Student’s t-test. Results The division of the sciatic nerve occurred at a mean of 44 ± 20 mm (range 0 to 73mm) above the popliteal crease, with no significant difference between the two groups. In all 10 legs (5 left and 5 right), sciatic nerve in the popliteal fossa consisted of two separate nerves, the tibial nerve and common peroneal nerve enveloped by a common epineural sheath that accompanied the nerves after their divergence in the fossa. In one leg in each group, the BVA solution did not flow proximally but leaked at the level of the catheter tip, forming a pool of injectate between the intermuscular fasciae. Careful dissection along the tibial nerve revealed that in both legs the catheter tip perforated the sheath, resulting in extraepineural injection. These two legs were excluded from further analysis. In the remaining eight legs, the BVA solution traveled 147 ± 34 mm (group A) and 172 ± 50 mm (group B) proximal within the sheath from the injection point (NS), (Figure 6). 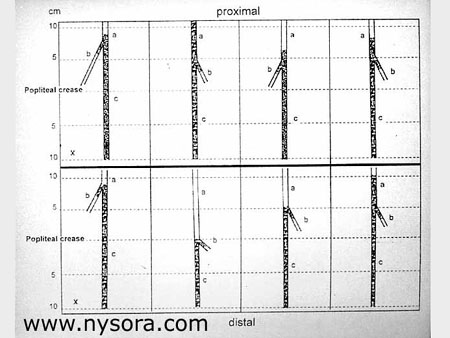 Figure 6.
The dye readily filled the sheath, with minimal or no apparent leakage of the solution outside the sheath. The injectate reached the apparent division of the sciatic nerve in the popliteal fossa, bathing both the tibial nerve and common peroneal nerve in all 8 legs (Figures 5 and 7) except one in group A.  Figure 7. Posterior aspect of the thigh. Skin and subcutaneous tissue removed. 1. Tibial nerve-medial component of the sciatic nerve. 2. Common epineural sheath covering popliteal nerve 3. Common trunk of the sciatic nerve 4. Blue vinyl acetate within the common epineural sheath
 Figure 8. Common epineural sheath (2) encompasses sciatic nerve at its division (1) and extends onto both branches common peroneal nerve and tibial nerve. In all examined legs, the epineural tissue sheath surrounded the sciatic nerve and its main divisions (Figure 8). This tissue formed a virtual fluid conduit, which appeared to communicate among the sciatic nerve, tibial nerve and common peroneal nerve in the fossa. This was evident from the extent of the spread of BVA within the tibial nerve sheath and into the sheath extensions of both the sciatic nerve and common peroneal nerve. Cross-sectional examination of the specimens containing the catheter documented the placement of the catheter within the epineural sheath, and not intraneurally (Figure 4). Histological examination of all 10 nerve specimens at multiple levels from 15 cm to 30 cm above the popliteal fossa showed that the sciatic nerve consists of two distinct nerve bundles, the common peroneal nerve and tibial nerve, which are enveloped by separate epineurium, and contained in a common epineural adventitia (Figure 4). The two components of the sciatic nerve could be traced and separated with minimal traction along entire length of the thigh in all examined extremities. Discussion Our results demonstrate the existence of a continuous epineural sheath surrounding the sciatic nerve and its major divisions, the tibial nerve and common peroneal nerve. This sheath forms a fluid conduit which communicates among the major nerve divisions in the popliteal fossa. We described the existence of an adventitial sheath that encompasses the sciatic nerve at the level of its division to tibial nerve and common peroneal nerve [1], (Figure 8). Injection of five mL of dye into this sheath at the level of the division of the sciatic nerve resulted in spread of the dye 5-10 cm within the sheath without significant leakage outside the sheath. Confirming our previous findings, the present data show that this epineural sheath is virtually continuous, envelops the sciatic nerve, tibial nerve and common peroneal nerve, and allows conduction of solutions injected into the sheath. These anatomical characteristics of the sciatic nerve and its epineural sheath offer a possible explanation to some clinical phenomena often seen during popliteal nerve block. For example, anesthesia is often obtained in both divisions of the sciatic nerve, although paresthesia or the response to the nerve stimulation is obtained in the distribution of either the tibial nerve or the common peroneal nerve. On the other hand, incomplete block, with anesthesia in the distribution of only one division of the nerve after block, under apparently identical clinical circumstances, is also a common occurrence [7]. Since tibial nerve and common peroneal nerve separate at a highly variable distance from the popliteal crease (0 to 115mm) [1], needle inserted at 5 to 7cm above the popliteal fossa crease will be next to only one of the divisions of the popliteal nerve. In the former case, it is possible that the needle tip is positioned within the epineural sheath or above the division of the nerve, resulting in either spread of solution of local anesthetic onto both divisions of the nerve, or a deposition of the local anesthetic close to the main trunk proximal to division. In the latter case, an extraneural injection (injection outside the epineural adventitia) could result in a pool of local anesthetic in the popliteal fossa fat that is close to only one division of the nerve, thus giving rise to partial block. It is important to emphasize that the placement of an intraepineural catheter is not equivalent to intraneural or intrafascicular placement. This was demonstrated histologically (Figure 4) and confirmed by the absence of significant back pressure during the injection of 15 or 30 mL of the BVA solution into the sheath. Several attempts to inject BVA into the fasciculi of the dissected nerve resulted in significant resistance to injection which promptly disappeared after withdrawal of the needle outside the fasciculus. Thus, as previously demonstrated during intraoperative exposure of the peripheral nerves, an inadvertent intraneural injection during neuronal block should be recognized as an increase in resistance to injection in addition to severe pain or paresthesia [8]. However, if the solution of local anesthetic is injected intraepineurally, it should substantially spread within the sheath, resulting in conduction block in the entire popliteal nerve distribution. This mechanism could explain successful nerve block of the sciatic nerve trunk when the response to the nerve stimulation or paresthesia is obtained in the distribution of only one division of the sciatic nerve. REFERENCES:
1. Vloka JD, Hadzic A, Lesser J et al.: Anatomical considerations for sciatic nerve block in the popliteal fossa through the lateral approach. Anesthesiology 1995; 83(3A): A882. 2. Stewart JD, Aguayo AJ: Compression and entrapment neuropathies, Peripheral neuropathy. Edited by Dyck PJ, Thomas PK, Lambert EH, Bunge R. Philadelphia, W.B. Saunders Company, 1984:1435-57. 3. Sunderland S: The sciatic nerve and its tibial and common peroneal divisions. Anatomical and physiological features., Nerves and Nerve Injuries, Churchill Livingstone, 1978:925-66. 4. Fawcett DW: The Nervous Tissue, Bloom and Fawcett a Textbook of Histology. Edited by Fawcett DW. New York, Chapman & Hall, 1984:336-9. 5. Millesi H, Terzis JK: Nomenclature in peripheral nerve surgery, Microreconstruction of Nerve Injuries. Edited by Terzis JK. Philadelphia, W.B. Saunders Company, 1987:3-13. 6. Thomas PK, Olsson Y: Microscopic anatomy and function of the connective tissue components of peripheral nerve, Peripheral Neuropathy. Edited by Dyck PJ, Thomas PK, Lambert EH, Bunge R, W.B. Saunders Company, 1984:97-120. 7. Kilpatrick AWA, Coventry DM, Todd JG: A Comparison of two Approaches to Sciatic Nerve Block . Anaesthesia 1992: 47;155-7. 8. Kempthorne PM, Brown TCK: Nerve blocks around the knee in children. Anaesth Intensive Care 1984;12(1):14-7. |