In the current study an MRI simulation of the popliteal block was undertaken to compare the accuracy of needle placement in relationship to the sciatic nerve using the intertendinous and classical approaches.
Based on: Hadzic A, Vloka JD, Singson R, Santos AC, Thys DM. A comparison of Intertendinous and Classical Approaches to Popliteal Nerve Block Using MRI Simulation. Anesth Analg 2002; 94: 1321-4.
|
Introduction Sciatic nerve block in the popliteal fossa (popliteal block) has several advantages over other anesthetic techniques for lower extremity surgery (1). As opposed to the more proximal approaches to the sciatic nerve block, the popliteal block spares the hamstrings muscles and promotes postoperative ambulation. Compared to spinal anesthesia, it results in a unilateral block, carries no risk of “post dural” puncture headache, results in prolonged postoperative analgesia, and it can be performed in patients being treated with anticoagulant therapy. Despite these potential advantages, popliteal block is not often used for lower extremity surgery in the United States (2). The reasons for the infrequent use of this block may be related to inadequate training of residents (2), concerns over operating room efficiency and a highly variable success rate of the block (2-4). The most frequently used technique for popliteal block is the classical, posterior approach, where the needle insertion site is 7 cm above the popliteal fossa crease and 1 cm lateral to the midline of the popliteal fossa triangle (formed by the popliteal fossa crease, the semimembranosus and semitendinosus muscles, and the biceps femoris muscles) (4). The needle is then advanced from posterior to anterior until the sciatic nerve is identified (3). However, these landmarks are rather unclear in many patients and often multiple attempts are required to localize the sciatic nerve using this approach. Consequently, in our clinical practice and training of residents, we have developed a new, intertendinous approach to popliteal block (5). Using this approach, the needle is inserted at the midpoint between the tendons of the biceps femoris and semitendinosus muscles, rather than 1 cm lateral to the midline of the popliteal fossa triangle as in the classical approach. In the current study an MRI simulation of the popliteal block was undertaken to compare the accuracy of needle placement in relationship to the sciatic nerve using the intertendinous and classical approaches. Material & Methods After approval by the Institutional Review Board, 10 healthy, adult volunteers were enrolled in the study after written consent was obtained. The anatomical surface landmarks for needle insertion using the intertendinous and classical approaches to popliteal block were identified by two attending anesthesiologists familiar with popliteal block (authors of the study) and then labeled using magnetic resonance imaging (MRI) contrast markers (vitamin E capsules). The anesthesiologists jointly examined the extremities and agreed upon the landmarks and the insertion points for both approaches in all patients. For the classical technique, the needle “insertion site” (for off-line simulation) was labeled with vitamin E capsules 7 cm above the popliteal fossa crease and 1 cm lateral to the midline of the popliteal fossa triangle (identified by drawing a line along the converging course of the bodies of the semimembranosus and biceps femoris muscles) (4). For the intertendinous approach, the needle “insertion site” was also labeled 7 cm above the popliteal fossa crease, but in contrast to the classical technique, at the mid-point between the tendons of the semimembranosus and biceps femoris muscles (Figure 1). The described landmarks and needle insertion sites were done for both legs in all subjects. 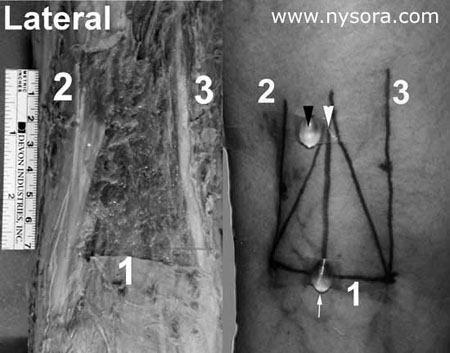
Figure 1. Example on the left: Popliteal block – Intertendinous Approach. Landmarks:1.Popliteal fossa crease 2.Tendon of biceps femoris muscle 3.Tendon of semitendinosus/semimembranosus muscles Example on the right: The black arrow indicates the needle insertion site in the “classical” approach to popliteal block which utilizes the “popliteal fossa triangle” as a landmark. (Milwaukee, WI) software was used by an independent, blinded interpreter. For both approaches, the simulations were performed at 7 cm above the popliteal fossa crease and at an angle perpendicular to the horizontal plane. A line simulating the needle insertion path (simulated or virtual needle) was placed through the labeled “insertion sites” on the image and extended anteriorly in a saggittal plane (perpendicular to the horizontal plane), just as would be done in a popliteal block (Figure 2) (4,5). The order of simulations was random so approximately half of the simulations were first done with the intertendinous and half with the classical approach. The spatial proximity of the needle trajectory to the sciatic nerve and its distance (relationships) to the structures important to popliteal block were measured for each simulation. 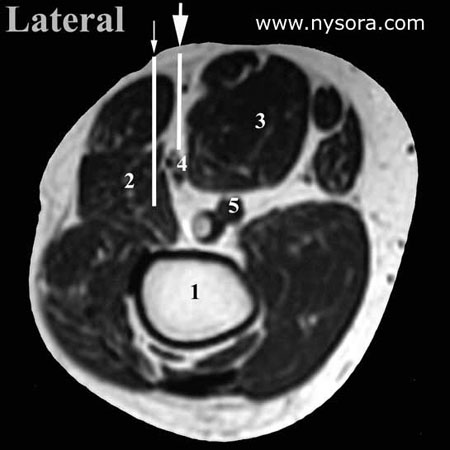
Figure 2. Simulation of the popliteal block using MRI images. The large arrow indicates a typical needle path in the intertendinous approach, whereas the small arrow shows too lateral insertion of the needle is common in the classical (triangle) approach. Data are expressed as means +/- standard errors for continuous measures. Since both approaches were studied in the same volunteers, McNemar chi-square tests were used to evaluate differences between the two approaches for the proportions presented in Table 2. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS for Windows, version 5.0.2, Chicago, IL); p
Table 1: Anatomical measurements Relevant to Popliteal nerve block (n=10).
Table 2: Needle Trajectories Measurements in Relation to Popliteal Fossa Structures
Results The mean age, weight and height of the ten volunteers was 39 +/- 8 years (range 20-60 years), 78 kg +/- 12 kg (range 53-90 kg) and 174 cm +/- 9 cm (range 162-186 cm), respectively. The anatomical measurements of significance to popliteal block are presented in Table 1. The tibial and common peroneal components of the sciatic nerve appeared to be undivided or very close on MRI images at 7 cm above the popliteal fossa crease in all studied extremities. The proportion of simulated needle-to-nerve contacts, as well as other simulated needle insertion characteristics, are presented in Table 2. Simulated needle-to-nerve contact occurred significantly more often with the intertendinous (70%) than with the classical approach (25%). In the remaining 30% of needle simulations which did not contact the sciatic nerve using the intertendinous approach, 10-15° lateral redirection of the simulated needle placed the needle in line with the sciatic nerve, avoiding the risk of intersecting the popliteal artery or vein. In contrast, 75% of needle simulations using the classical approach missed the sciatic nerve and required medial redirection of the needle in order to reach the sciatic nerve. The required medial redirection of the needle (between 10° and 30°) in order to reach the sciatic nerve using the classical approach, carries a risk of intersecting the popliteal artery and vein which are situated medially to the sciatic nerve. Indeed, in three simulations through the classical approach the simulated needle path encountered the popliteal vessels with medial redirections of the needle. Furthermore, passage of the simulated needle through the biceps femoris muscle occurred less often with the intertendinous approach (5%) than with the classical approach (85%), Table 2. Discussion These data suggest that the intertendinous approach to popliteal block provides more accurate localization of the sciatic nerve in the popliteal fossa. Indeed, simulation of needle placement using the intertendinous approach resulted in needle-sciatic nerve contacts almost three times greater than with the classical technique. Furthermore, medial redirection of the needle (toward the popliteal vessels) was required to contact the sciatic nerve using the classical approach as opposed to the lateral redirection with the intertendinous technique. We speculate that the main reason for difficulty in localizing the sciatic nerve using the classical approach is an inability to accurately identify the boundaries of the popliteal fossa triangle. The base of the triangle is formed by the popliteal fossa crease and the sides by the semitendinosus and semimembranosus muscles medially and the biceps femoris muscle laterally. Whereas the muscular boundaries of the triangle are easily identified in cadavers, they are much more obscure and can be difficult to discern in patients (Figure 1). Consequently, often it is not clear what part of the muscles, tendon or body is palpated in many subjects. In contrast, the tendons of these muscles, which we proposed as landmarks for the intertendinous approach, are easily and accurately identified even in the obese patient (5). Importantly, these tendons do not converge into a triangle (as the muscles do higher in the thigh), but rather follow a near-parallel course in the popliteal fossa. These data and data from our recent clinical study (5) indicate that sciatic nerve is more accurately identified with the intertendinous approach using the tendons as landmarks rather than popliteal fossa triangle as is used in the classical approach to popliteal block. Since the muscle boundaries of the popliteal triangle are often difficult to appreciate with accuracy, it is possible that the tendons are often mistaken as the boundaries of the muscles. In that case, placement of the needle would then be too lateral for needle contact with the sciatic nerve. This medial redirection of the needle which would be required in order to reach the sciatic nerve may carry a higher risk of puncturing the popliteal vessels, especially when longer needles (e.g., 40 mm or longer) are used. In addition, needles inserted using the classical approach more often transect the body of the biceps femoris muscle, which may result in discomfort during the procedure. The use of MRI to compare needle trajectory does not provide information on clinical success of the block, or the difference in the ease of nerve localization between the intertendinous versus classical approaches. Nevertheless, in an earlier clinical study, we demonstrated that the intertendinous approach to popliteal block resulted in a 100% success rate (5). The results of the current study may also have been affected by bias due to the fact that unblinded investigators (two authors of the study) identified the landmarks for both approaches. However, the risk for this bias is small for two reasons. The landmarks for both the intertendinous and classical approaches were identified using “predetermined” criteria and there was uniform agreement between the two investigators with respect to the needle insertion site. Secondly, our finding of high frequency of needle to nerve contact with the intertendinous approach in the current study is in agreement with our earlier clinical study. In summary, under the conditions of our study, the intertendinous approach to popliteal block results in more proximate needle placement to the sciatic nerve in the popliteal fossa. In contrast, relying on the popliteal fossa triangle in the classical approach may result in needle placement which is too lateral to the sciatic nerve. This may require more attempts at nerve localization and redirection of the needle medially which places the popliteal vessels at risk of puncture. REFERENCES: 1. Vloka JD, Hadzic A, Mulcare R, et al. Combined blocks of the sciatic nerve at the popliteal fossa and posterior cutaneous nerve of the thigh for short saphenous vein stripping in outpatients: An alternative to spinal anesthesia. J Clin Anesth 1997;9:618-22. 2. Hadzic A, Vloka JD, Kuroda MM et al. The practice of peripheral nerve blocks in the United States. A national survey. Reg Anesth Pain Med 1998:23:241-6. 3. Rorie DK, Byer DE, Nelson DO, et al. Assessment of block of the sciatic nerve in the popliteal fossa. Anesth Analg, 1980; 59:371-6. 4. Brown DL: Popliteal nerve block. In: Brown DL, ed. Atlas of Regional Anesthesia. Philadelphia: W.B.Saunders Co., 1992:109-13. 5. Hadzic A, Vloka JD. A comparison of the posterior versus lateral approaches to the block of the sciatic nerve in the popliteal fossa. Anesthesiology 1998; 88:1480-6. |
|||||||||||||||||||||||||||||||||||||||