Breastfeeding patient
- The presence of anesthetic agents in breastmilk
- The anesthetic management of breastfeeding patients
Definition and mechanisms
- Breastfeeding, or nursing, is the process by which human breast milk is fed to a child and is one of the most effective ways to ensure the health and survival of the infant
- Breastfeeding has many health benefits for the mother and infant
- Women who are breastfeeding may require anesthesia or sedation
- Concerns regarding the passage of medications into breast milk may lead to inconsistent advice resulting in:
- Interruption of feeding for 24 hours or longer
- Pumping and discarding of milk
- Early cessation of breastfeeding
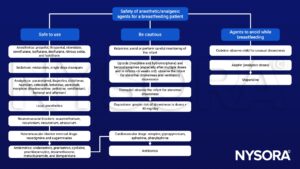
- All anesthetic and analgesic drugs transfer to breastmilk, however, only small amounts are present and in very low concentrations considered clinically insignificant
- It is safe to breastfeed as usual after anesthesia and surgery
- There is no need to express and discard breast milk (“pump and dump”) after anesthesia
Anesthetic agents and breastmilk
- Neonatal agent exposure is expressed by the relative infant dose (RID)
- The RID takes into account maternal and infant weight as well as the concentration of drug in breastmilk and indicates the percentage of drug in the baby relative to the mother
- RID levels < 10% are considered safe
- Nearly all anesthetic agents have RID values significantly less than 10%, except for morphine (9%)
- Certain opioids (i.e., codeine and tramadol) and drug classes (i.e., amphetamines, chemotherapy agents, ergotamines, and statins) are not recommended in breastfeeding mothers
- Due to pharmacogenetic variability in metabolizing codeine or tramadol, there is a risk of a neonatal opioid overdose if an “ultra-metabolizer” mother breastfeeds a “slow metabolizer” neonate
Anesthetic management

Suggested reading
- Mitchell, J., Jones, W., Winkley, E., Kinsella, S.M., 2020. Guideline on anaesthesia and sedation in breastfeeding women 2020. Anaesthesia 75, 1482–1493.
- Wanderer JP, Rathmell JP. 2017. Anesthesia & breastfeeding: more often than not, they are compatible. 127;4.
- General principles for anesthesia and perioperative management for a patient who is breastfeeding. Uptodate.com
- Statement on resuming breastfeeding after anesthesia. 2019. American Society of Anesthesiologists
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com